Documents
| Date | Title | Description | Description | Program/Initiative | Topic | Type of Document | Document Link | ||||||||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| January, 2026 | DAP Certificate of Accreditation (December 2025, Expiry date: November 2026.) | Laboratory | Certification Documents | Download | |||||||||||||||||||||||
| December, 2025 | Doxycycline for the Prevention of Bacterial Sexually Transmitted Infections Initiative - Indicators Report 2024 | Drug Treatment Program | Download | ||||||||||||||||||||||||
| December, 2025 | Guidance for the use of Pre-Exposure Prophylaxis (PrEP) for the prevention of HIV acquisition in British Columbia | Important Information
Guidelines updated: December 2025
Therapeutic Guidelines Menu | PrEP | PrEP Documents and Forms, Therapeutic Guidelines | Download | ||||||||||||||||||||||
| December, 2025 | Laboratory Requisition Form, Hepatitis C Resistance Testing | Hepatitis, Laboratory Test Order Forms | Download | ||||||||||||||||||||||||
| November, 2025 | PrEP Semi-Annual Report for British Columbia – Second Quarter 2025 | Drug Treatment Program | PrEP | PrEP Quarterly Report | Download | ||||||||||||||||||||||
| October, 2025 | Update to HPV Immunization Eligibility | Drug Treatment Program | Notice to Prescribers | Dear Doctor Letter | Download | ||||||||||||||||||||||
| September, 2025 | Patient Information Sheet for Drug Treatment Program Participants | Drug Treatment Program | PrEP | PrEP Documents and Forms | Download | ||||||||||||||||||||||
| August, 2025 | PrEP Semi-Annual Report for British Columbia – Fourth Quarter 2024 | Drug Treatment Program | PrEP | PrEP Quarterly Report | Download | ||||||||||||||||||||||
| August, 2025 | BC-CfE Drug Treatment Program Monthly Report (December 2024) | Drug Treatment Program | DTP Status Report | Download | |||||||||||||||||||||||
| August, 2025 | BC-CfE Drug Treatment Program Monthly Report (November 2024) | Drug Treatment Program | DTP Status Report | Download | |||||||||||||||||||||||
| August, 2025 | BC-CfE Drug Treatment Program Monthly Report (October 2024) | Drug Treatment Program | DTP Status Report | Download | |||||||||||||||||||||||
| January, 2025 | Mpox letter to DTP prescribers | Letter to prescribers | Dear Doctor Letter | Download | |||||||||||||||||||||||
| December, 2024 | BC-CfE Drug Treatment Program Monthly Report (September 2024) | Drug Treatment Program | DTP Status Report | Download | |||||||||||||||||||||||
| December, 2024 | BC-CfE Drug Treatment Program Monthly Report (August 2024) | Drug Treatment Program | DTP Status Report | Download | |||||||||||||||||||||||
| December, 2024 | CAP certification (Until 2026) | Laboratory | Certification Documents | Download | |||||||||||||||||||||||
| December, 2024 | BC-CfE Quarterly Report - Second Quarter 2024 | Drug Treatment Program | BCCfE Reports | Download | |||||||||||||||||||||||
| November, 2024 | BC-CfE Drug Treatment Program Monthly Report (July 2024) | Drug Treatment Program | DTP Status Report | Download | |||||||||||||||||||||||
| November, 2024 | BC-CfE Drug Treatment Program Monthly Report (June 2024) | Drug Treatment Program | DTP Status Report | Download | |||||||||||||||||||||||
| November, 2024 | BC-CfE Drug Treatment Program Monthly Report (May 2024) | Drug Treatment Program | DTP Status Report | Download | |||||||||||||||||||||||
| November, 2024 | BC-CfE Drug Treatment Program Monthly Report (April 2024) | Drug Treatment Program | DTP Status Report | Download | |||||||||||||||||||||||
| September, 2024 | BC-CfE Quarterly Report - First Quarter 2024 | Drug Treatment Program | BCCfE Reports | Download | |||||||||||||||||||||||
| September, 2024 | HIV Monitoring Semi-Annual Report, Second Quarter 2024 |
| STOP HIV/AIDS | ||||||||||||||||||||||||
| September, 2024 | PrEP Semi-Annual Report for British Columbia – Second Quarter 2024 | Drug Treatment Program | PrEP | PrEP Quarterly Report | Download | ||||||||||||||||||||||
| July, 2024 | BC-CfE Drug Treatment Program Monthly Report (March 2024) | Drug Treatment Program | DTP Status Report | Download | |||||||||||||||||||||||
| July, 2024 | BC-CfE Drug Treatment Program Monthly Report (February 2024) | Drug Treatment Program | DTP Status Report | Download | |||||||||||||||||||||||
| July, 2024 | Cabotegravir plus rilpivirine (PrCabenuva) in PLWH with viremia (June 2024) | Download | |||||||||||||||||||||||||
| June, 2024 | BC-CfE Drug Treatment Program Monthly Report (January 2024) | Drug Treatment Program | DTP Status Report | Download | |||||||||||||||||||||||
| May, 2024 | BC-CfE Pharmacovigilance 2023 Annual Report | Pharmacovigilance Initiative | Download | ||||||||||||||||||||||||
| May, 2024 | BC-CfE Resources for Providers (Poster) | Resource for Providers | Dear Doctor Letter | Download | |||||||||||||||||||||||
| May, 2024 | PrEP Semi-Annual Report for British Columbia – Fourth Quarter 2023 | Drug Treatment Program | PrEP | PrEP Quarterly Report | Download | ||||||||||||||||||||||
| April, 2024 | BC-CfE Drug Treatment Program Monthly Report (December 2023) | Drug Treatment Program | DTP Status Report | Download | |||||||||||||||||||||||
| April, 2024 | HIV Drug Treatment Program Enrolment Form | Drug Treatment Program | Download | ||||||||||||||||||||||||
| March, 2024 | BC-CfE Drug Treatment Program Monthly Report (November 2023) | Drug Treatment Program | DTP Status Report | Download | |||||||||||||||||||||||
| March, 2024 | BC-CfE Drug Treatment Program Monthly Report (October 2023) | Drug Treatment Program | DTP Status Report | Download | |||||||||||||||||||||||
| March, 2024 | HIV Monitoring Semi-Annual Report, Fourth Quarter 2023 |
| STOP HIV/AIDS | ||||||||||||||||||||||||
| February, 2024 | BC-CfE Quarterly Report - Fourth Quarter 2023 | BCCfE Reports | Download | ||||||||||||||||||||||||
| February, 2024 | BC-CfE Quarterly Report - Third Quarter 2023 | BCCfE Reports | Download | ||||||||||||||||||||||||
| December, 2023 | BC-CfE Drug Treatment Program Monthly Report (September 2023) | Drug Treatment Program | DTP Status Report | Download | |||||||||||||||||||||||
| December, 2023 | Doxycycline for B-STI Prevention – Enrolment and Prescription Form | Doxycycline | Download | ||||||||||||||||||||||||
| December, 2023 | Laboratory Requisition Form, British Columbia | Laboratory | Laboratory Test Order Forms | Download | |||||||||||||||||||||||
| December, 2023 | Laboratory Requisition Form, Outside British Columbia | Laboratory | Laboratory Test Order Forms | Download | |||||||||||||||||||||||
| December, 2023 | Respiratory syncytial virus (RSV) vaccine guideline statement | Therapeutic Guidelines Menu | Therapeutic Guidelines | Download | |||||||||||||||||||||||
| December, 2023 | Doxycycline for Bacterial STI Prevention | Click here to link to information about this initiative | Notification of Initiative Launch | Dear Doctor Letter | Download | ||||||||||||||||||||||
| December, 2023 | Opportunistic Infection Therapeutic Guidelines | Therapeutic Guidelines MenuCANDIDIASISCRYPTOCOCCOSISMYCOBACTERIUM AVIUM COMPLEX (MAC)PNEUMOCYSTIS PNEUMONIA (PCP)SYPHILISTOXOPLASMOSISWHAT’S NEW IN THE GUIDELINESTreatment of Late Latent Syphilis Updated: November 2024 Page 12-13, Latent Syphilis: Retreatment of people with late latent syphilis or syphilis of unknown duration may be indicated when the timing of second or third doses falls outside of an optimal range. A table is provided to guide assessment | |||||||||||||||||||||||||
| November, 2023 | BC-CfE Drug Treatment Program Monthly Report (August 2023) | Drug Treatment Program | DTP Status Report | Download | |||||||||||||||||||||||
| November, 2023 | Doxycycline for B-STI Prevention Patient Information Sheet | Doxycycline | Download | ||||||||||||||||||||||||
| November, 2023 | SPH Ambulatory Pharmacy Map and Hours of Operation | PrEP | PrEP Documents and Forms | Download | |||||||||||||||||||||||
| November, 2023 | BC-CfE Drug Treatment Program Monthly Report (July 2023) | Drug Treatment Program | DTP Status Report | Download | |||||||||||||||||||||||
| November, 2023 | BC-CfE Drug Treatment Program Monthly Report (June 2023) | Drug Treatment Program | DTP Status Report | Download | |||||||||||||||||||||||
| October, 2023 | PrEP Semi-Annual Report for British Columbia - Second Quarter 2023 | Drug Treatment Program | PrEP | PrEP Quarterly Report | Download | ||||||||||||||||||||||
| September, 2023 | HIV Drugs available through the BC-CfE | Antiretrovirals and other select medications are available through the BC-CfE’s HIV Treatment Program. These medications may be requested by submitting an HIV Drug Request Prescription Form. Requests will be assessed according to BC-CfE therapeutic guidelines. Clinical justification and/or supportive documentation may be required. Individuals will obtain, at no cost, medications offered through the BC-CfE’s Drug Treatment Program. A request for restricted, or non-BC-CfE formulary medications, may be submitted with full documentation supporting the request. These will be subject to clinical review on a case-by-case basis, for consideration of exceptional coverage. HIV Drugs available through the BC-CfE ART Regimens for Initial Therapy and for Switching ART in Virologically Stable Suppressed Adults HIV Treatment Program Enrolment Form HIV Drug Request Prescription Form Cabenuva® Recommendations (May 2024) Cabenuva® Request Form Cabenuva® Considerations for the Client https://www.youtube.com/embed/eki7EU27_EU | Drug Treatment Program | Treatment as Prevention¨ | |||||||||||||||||||||||
| September, 2023 | HIV/AIDS Drug Request Prescription Form | The HIV/AIDS Drug Request Prescription Form (PDF) may be downloaded here. Paper copies of the form may be requested from the BC-CfE HIV Drug Treatment Program. Information about how to complete the prescription form can be found in the next section. For information on how to use this form, and to learn about program eligibility, enrolment, and obtaining HIV medication in BC, please click here. | Drug Treatment Program | HIV Clinical Care | Download | ||||||||||||||||||||||
| September, 2023 | BC-CfE Pharmacovigilance 2022 Annual Report | Pharmacovigilance Initiative, Quality and Safety | Download | ||||||||||||||||||||||||
| September, 2023 | BC-CfE Quarterly Report - Second Quarter 2023 | BCCfE Reports | Download | ||||||||||||||||||||||||
| September, 2023 | BC-CfE Drug Treatment Program Monthly Report (May 2023) | Drug Treatment Program | DTP Status Report | Download | |||||||||||||||||||||||
| August, 2023 | BC-CfE Drug Treatment Program Monthly Report (March 2023) | Drug Treatment Program | DTP Status Report | Download | |||||||||||||||||||||||
| August, 2023 | BC-CfE Drug Treatment Program Monthly Report (April 2023) | Drug Treatment Program | DTP Status Report | Download | |||||||||||||||||||||||
| August, 2023 | BC-CfE Quarterly Report - First Quarter 2023 | BCCfE Reports | Download | ||||||||||||||||||||||||
| July, 2023 | Care of HIV Positive Pregnant Women and Interventions to Reduce Perinatal Transmission Guidelines | Therapeutic Guidelines MenuSupportive non-directive counseling regarding reproductive choices, high risk prenatal care, modified management of labour and delivery, and postpartum and infant care are all important components in the comprehensive care of the HIV infected woman and her infant. The provision of pregnancy and reproductive health care in HIV infected women should involve a collaboration with individuals experienced in the management of high risk pregnancy and HIV care of women and infants. In British Columbia (BC), the Women and Family HIV Centre (Oak Tree Clinic), a program of BC Women’s Hospital and Health Centre, provides clinical care and guidance for this population of HIV infected and exposed adults and children. The interdisciplinary team at the Oak Tree Clinic works in partnership with the BC Centre for Disease Control for surveillance and with the BC Centre for Excellence in HIV/AIDS for drug therapy and overall provincial coordination. Longitudinal surveillance on pregnancy outcomes in HIV positive women are tracked in BC through information provided by clinicians throughout the province who care for HIV positive pregnant women and their infants. This is vital for the continuous quality improvement of antiretroviral prescribing in pregnancy. | Therapeutic Guidelines | Download | |||||||||||||||||||||||
| June, 2023 | Cabotegravir and Rilpivirine Extended-Release Injectable Suspensions (Cabenuva(R)) | Cabenuva(R) Recommendations (May 2024) Cabenuva(R) Request Form (Jan 2025) Considerations for the Client (May 2023) | Considerations for the Prescriber | Dear Doctor Letter | |||||||||||||||||||||||
| June, 2023 | BC-CfE Drug Treatment Program Monthly Report (February 2023) | Drug Treatment Program | DTP Status Report | Download | |||||||||||||||||||||||
| June, 2023 | BC-CfE Drug Treatment Program Monthly Report (January 2023) | Drug Treatment Program | DTP Status Report | Download | |||||||||||||||||||||||
| June, 2023 | BC-CfE Drug Treatment Program Monthly Report (December 2022) | Drug Treatment Program | DTP Status Report | Download | |||||||||||||||||||||||
| May, 2023 | BC-CfE Quarterly Report - Fourth Quarter 2022 | BCCfE Reports | Download | ||||||||||||||||||||||||
| April, 2023 | PrEP Semi-Annual Report for British Columbia - Fourth Quarter 2022 | Drug Treatment Program | PrEP | PrEP Quarterly Report | Download | ||||||||||||||||||||||
| April, 2023 | HIV Monitoring Semi-Annual Report, Fourth Quarter 2022 |
| STOP HIV/AIDS | ||||||||||||||||||||||||
| March, 2023 | BC-CfE Drug Treatment Program Monthly Report (November 2022) | STOP HIV/AIDS | DTP Status Report | Download | |||||||||||||||||||||||
| March, 2023 | Therapeutic Guidelines for Antiretroviral (ARV) Treatment of Adult HIV Infection |
DOWNLOAD: Therapeutic Guidelines for Antiretroviral (ARV) Treatment of Adult HIV Infection (PDF)
March 2023
These guidelines were developed by the British Columbia Centre for Excellence in HIV/AIDS (BC-CfE) and the Committee for Drug Evaluation and Therapy (CDET) for HIV care providers and provide recommendations for the treatment of adult HIV infection in BC. The BC-CfE encourages providers to exercise clinical judgment on a case by case basis and individualize care where appropriate.
The therapeutic guidelines document includes the following sections:
Guideline for Antiretroviral Therapy Regimens for Initial Therapy and for Switching ART in Virologically Stable Suppressed Adults
This section regular BC-CfE Drug Treatment Program formulary options for initial ART in adults with HIV infection as of Fall 2019, taking into consideration the CDETâs Scientific Review and recommendations as well as cost considerations. In the event where ART regimen switch is being considered in virologically suppressed individuals with no known resistance mutations or intolerance to specific agents, these ART options should also be considered. Prescribers requesting alternative ART are expected to provide justification and appropriate supportive documentation with the prescription request. Consistent with Pharmacare practices, the BC-CfE encourages the use of generics, including voluntary de-simplification of ART regimens, where appropriate.
BC-CfE Eligibility Criteria for Emtricitabine-Tenofovir Alafenamide (FTC/TAF; Descovy¨)
This section summarizes clinical criteria for BC-CfE Drug Treatment Program eligibility for FTC/TAF 200-25 mg and FTC/TAF 200-10 mg tablets. Justification and supportive documentation should accompany the HIV Drug Treatment Program Prescription Request Form for FTC/TAF.
Scientific Review and Recommendations for the Therapeutic Guidelines
This section includes the BC-CfE CDET review of the available evidence and scientific recommendations regarding the use of antiretroviral therapy (ART) in adults with HIV-1 infection
| |||||||||||||||||||||||||
| March, 2023 | BC-CfE Drug Treatment Program Monthly Report (October 2022) | Drug Treatment Program | DTP Status Report | Download | |||||||||||||||||||||||
| March, 2023 | BC-CfE Quarterly Report - Third Quarter 2022 | BCCfE Reports | Download | ||||||||||||||||||||||||
| December, 2022 | BC-CfE Drug Treatment Program Monthly Report (September 2022) | Drug Treatment Program | DTP Status Report | Download | |||||||||||||||||||||||
| December, 2022 | BC-CfE Drug Treatment Program Monthly Report (August 2022) | Drug Treatment Program | DTP Status Report | Download | |||||||||||||||||||||||
| December, 2022 | BC-CfE Drug Treatment Program Monthly Report (July 2022) | Drug Treatment Program | DTP Status Report | Download | |||||||||||||||||||||||
| November, 2022 | PrEP Semi-Annual Report for British Columbia - Second Quarter 2022 | PrEP | PrEP Quarterly Report | Download | |||||||||||||||||||||||
| November, 2022 | BC-CfE Quarterly Report - Second Quarter 2022 | BCCfE Reports | Download | ||||||||||||||||||||||||
| November, 2022 | BC-CfE Drug Treatment Program Monthly Report (June 2022) | Drug Treatment Program | DTP Status Report | Download | |||||||||||||||||||||||
| November, 2022 | BC-CfE Drug Treatment Program Monthly Report (May 2022) | Drug Treatment Program | DTP Status Report | Download | |||||||||||||||||||||||
| October, 2022 | BC-CfE Drug Treatment Program Monthly Report (April 2022) | Drug Treatment Program | DTP Status Report | Download | |||||||||||||||||||||||
| October, 2022 | BC-CfE Drug Treatment Program Monthly Report (March 2022) | Drug Treatment Program | DTP Status Report | Download | |||||||||||||||||||||||
| September, 2022 | A tale of two pandemics: COVID-19 and its impact on HIV |
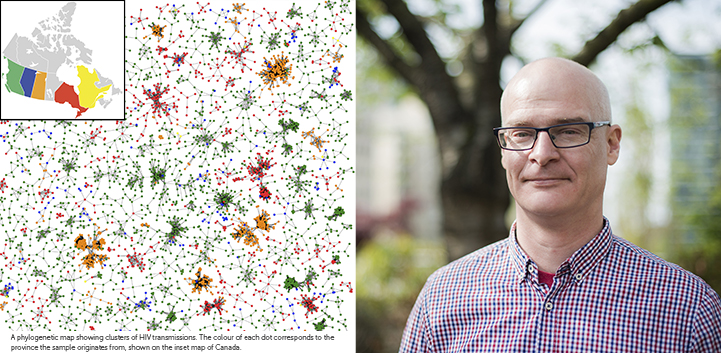
Founded with a mandate that includes persistent monitoring of viral diseases, the BC Centre for Excellence in HIV/AIDS (BC-CfE) has developed world-leading expertise in this increasingly crucial area of public health. As the SARS-CoV-2 virus swept around the planet in March of 2020, the BC-CfE's Molecular Epidemiology and Evolutionary Genetics Group, led by Senior Scientist, Jeffrey Joy, expanded its focus from HIV and viral hepatitis to include COVID-19, exploring its global, national, and regional spread and the impact it had on both HIV treatment and populations at risk of acquiring HIV. Briefly, using viral genome sequences and associated clinical characteristics integrated with evolutionary theory and methods, Dr. Joy and the Molecular Epidemiology and Evolutionary Genetics Group study how viruses evolve and adapt, monitor their transmission at multiple epidemic scales, and evaluate effectiveness of public health interventions in curbing their spread. In a pair of complementary studies (performed with assistance of funding by CIHR, Genome Canada and Genome British Columbia) released in summer 2022, the group took aim at understanding Canadian SARS-CoV-2 transmission and the impact of COVID lockdown on HIV transmission in our at-risk populations. COVID-19 Transmission in CanadaFirstly, using SARS-CoV-2 phylogenetic trees (family trees of the virus causing COVID-19 based on virus genome sequences) they carefully analyzed COVID-19 variant transmission into and across Canada and evaluated the impact that international travel restrictions had in curbing new introductions of the virus. This study was the subject of an article published in the journal eLife entitled: Genomic epidemiology of the first two waves of SARS-CoV-2 in Canada. "Large-scale SARS-CoV-2 genomic epidemiology analyses in Canada have so far been limited to a study on the early epidemic within Quebec," says lead author Angela McLaughlin, Research Assistant at the British Columbia Centre for Excellence in HIV/AIDS and PhD candidate in Bioinformatics at the University of British Columbia (UBC). "We wanted to elaborate on this research with a national-scale analysis for the first and second COVID-19 waves. Specifically, we evaluated the impact of international travel restrictions in March 2020 on international importations of the virus into Canada and on viral persistence into 2021." Their analysis tested the hypothesis that international travel restrictions enacted in March 2020 effectively reduced international importations of SARS-CoV-2 into Canada, yet ongoing introductions contributed to COVID-19 persistence into early 2021, exacerbated by highly transmissible B.1.1.7 and other VOC sublineages. They found that within 4 weeks from the implementation of travel restrictions, the rate of sublineage importation had dropped 10.3 fold. The restrictions drastically reduced, but did not eliminate transmission events attributable to international sources across all provinces. Comparing the first and second waves of the pandemic in Canada, it was noted that in the first wave, early sublineages had the opportunity to become established and resulted in large transmission chains. However, the second wave lasting from August 2020 to February 2021 was driven by cases from newly seeded sublineages, suggesting travel restrictions were insufficient to prevent new outbreaks when domestic prevalence was low. Restricting travel to and from locations with high relative COVID-19 prevalence, particularly attributable to emerging variants of concern, can be an effective tool to protect the healthcare system from being overwhelmed, but must be weighed against economic, social, and other impacts. Ongoing genomic surveillance in Canada and abroad to characterize changes in viral transmission and genetic variants are critical to inform evidence-based public policy on COVID-19 interventions. Impacts of COVID on HIV Transmission in British ColumbiaCollaborating with colleagues at the British Columbia Centre for Disease Control (BCCDC) and Vancouver Coastal Health (VCH), the BC-CfE's Molecular Epidemiology and Evolutionary Genetics Group led a second high profile study focusing specifically on the impact that the lockdown period that occurred early in the pandemic had on HIV transmission in British Columbia. The article titled: "Impact of SARS-CoV-2 lockdown on expansion of HIV transmission clusters among key populations: a retrospective phylogenetic analysis" carefully examined transmission patterns of HIV prior to, during, and after the lockdown. Looking at the interaction between the pandemics, this article revealed the impact of COVID-19 lockdown restrictions on individuals living with or at-risk of HIV infection and how the measures responding to one pandemic had consequences on another. A potential positive side effect of the restrictions was that the drastic increase in amount of time spent at home likely led to a dramatic reduction in contact rates and a corresponding reduction in risk of HIV transmission in some populations at risk of acquiring HIV. Conversely, populations characterized by non-sexual transmission routes such as needle sharing may have experienced an increased risk of HIV transmission due to the limited access to health services such as harm reduction sites and clinics that were shut or offered reduced hours and/or capacity during the lockdown. Investigating the hypothesis that differential trends in rates of transmission of HIV resulted from the implementation of lockdowns because of the reduced access to HIV management and prevention services, the article noted that a reduction in new infections diagnosed during the COVID-19 pandemic may relate to a decrease in willingness to seek sexual health services. The findings of the study indicate that populations of men who have sex with men (MSM) experienced a decline in detected HIV transmission based on cluster growth, to a level rarely seen in the previous 3 years, supporting the idea that reduced social contacts and increased time at home favourably reduced transmission. However, amongst people who inject drugs, the analysis revealed a contrasting pattern with a peak of HIV transmission higher than observed in the same time periods in the previous 3 years. Notably, clusters associated with populations of people who inject drugs (PWID) continued to experience elevated growth well beyond the initial period of instability in health service availability, indicating that the effects of such gaps can be long-term and difficult to counterbalance. The long-term downstream effects of these disruptions to engagement with HIV care services are yet to be seen, but studies estimate the negative impacts to be substantial. Lead author, Rachel Miller, Research Assistant at the BC-CfE and recent MSc graduate in Bioinformatics from UBC noted, "The difference in transmission revealed between at-risk populations highlights the need for persistence and increased vigilance in caring for our vulnerable populations during crises or times of public health emergency. Providing services to this group should be more like the treatment and care of those with diabetes or other chronic conditions because the consequences of interruption can be long-term and severe." Increasing vigilance and using innovative, targeted solutions are necessary to offset potential negative impacts on HIV treatment and prevention stemming from current and future pandemics or other major public health events.
| Forecast Newsletter | Download | |||||||||||||||||||||||
| September, 2022 | HIV Monitoring Semi-Annual Report, Second Quarter 2022 |
| STOP HIV/AIDS | ||||||||||||||||||||||||
| August, 2022 | BC-CfE Pharmacovigilance 2021 Annual Report | Pharmacovigilance Initiative, Quality and Safety | Download | ||||||||||||||||||||||||
| August, 2022 | BC-CfE Quarterly Report - First Quarter 2022 | BCCfE Reports | Download | ||||||||||||||||||||||||
| August, 2022 | PrEP Semi-Annual Report for British Columbia - Fourth Quarter 2021 | PrEP | PrEP Quarterly Report | Download | |||||||||||||||||||||||
| July, 2022 | Reducing barriers to care for those living with HCV in the Downtown East Side of Vancouver |
July 28th was World Hepatitis Day, an annual, purposeful opportunity to raise awareness of the global burden of viral hepatitis and to spark action. This year's theme is ‘I Can't Wait', which highlights the urgency from the global community to improve access to life-saving treatments. Around the world, every 30 seconds someone dies from a hepatitis related illness, despite the fact that the hepatitis C virus (HCV) is now generally considered a curable disease. Relatively new and well-tolerated direct-acting antivirals (DAAs) have a cure rate of 95 percent, however, there are still significant barriers to get treatment to those in need. Using its proven Treatment as Prevention strategy, the BC-CfE is raising awareness of HCV and its treatment in several ways. Most recently, the BC-CfE launched Hep C Connect, a pilot project funded by Gilead Sciences. Started in November 2021, it provides nurse-led, low barrier HCV testing, education, and linkage to care to clients of the Hope to Health (H2H) supervised consumption site located at 611 Powell Street. Beyond testing, the overarching aim of Hep C Connect is to enhance linkage to care and retention amongst unattached and underserved clients diagnosed with HCV in the Downtown East Side (DTES). Clients are offered rapid antibody testing and, if positive, same day, in-house, confirmatory HCV RNA testing. Pre- and post-test counselling, as well as follow-up and linkage to care is provided by an LPN. Hep C Connect provides a unique integration of HCV related services including low-barrier HCV education, community-based harm reduction services, and in house, same day testing, reducing barriers which often discourage people, especially in the DTES, from accessing lifesaving HCV treatment. As of this month, Hep C Connect has served a total of 148 clients; 51 of which had no existing attachment to primary care; 51 tested for HCV RNA with 24 clients who tested positive for HCV RNA, 5 of which have begun treatment. The program recently expanded to serve a higher volume of clients and extend the length of follow up from 6 to 12 months. Clinical Research Coordinator, Shaughna Cooper, with the BC-CfE's Viral Hepatitis Research Program (VHRP) said, "While clients may be coming to the H2H supervised consumption site primarily to access harm reduction supplies or consume drugs in a safe environment, Hep C Connect provides them with the ability to connect with staff about HCV and to learn more about their status. Given the complexity of challenges clients are facing, HCV tends to get deprioritized in the face of more immediate concerns which is why it is crucial to have low barrier access to testing and treatment available." Cooper also said, "Our hope is that Hep C Connect and the evaluation research that is produced from it helps to demonstrate the need for a standard integration of harm reduction services and pathway to HCV care as there's a dearth of similar programs at the moment." Per-SVR, short for PrEseRvation of Sustained Virologic Response, is another VHRP study and was launched in 2016 to evaluate the roll-out of DAAs in BC, following a request by provincial Ministry of Health. The Per-SVR study follows individuals who have recently cleared HCV following completion of DAA treatment and monitors their health outcomes, health care engagement, and reinfection events over time. This study will generate impactful data which will be important to tailor the provincial response to the HCV epidemic and, importantly, measure the impact on clients as well. Phindile Tshabalala, a Clinical Research Coordinator with the VHRP said ‘The scope of the Per-SVR study extends beyond understanding the prevalence of HCV reinfections within marginalised and disenfranchised communities. This is a four-year, longitudinal study that identifies the societal factors influencing access to care and examines the acute influence of policy on the access, availability, and point-of-care treatment for underserved populations. Community-centred healthcare is the foundation on which the Per-SVR study operates. Our relationship with participants goes far beyond the correlational, observational, and simple collection of data. We do this by building meaningful and long- standing relationships with our participants—the only way to ensure the continued improvement of health and wellbeing in our community. We try our best to provide consistent, accessible client care as it is essential to, and the only modality effective in, combatting HCV.' To mark the day the VHRP team strengthened bonds with the community and raised awareness about HCV testing, treatment and its studies as well as the services offered at H2H providing lunch, refreshments and educational materials and naloxone training.
| Forecast Newsletter | Download | |||||||||||||||||||||||
| July, 2022 | BC-CfE Drug Treatment Program Monthly Report (February 2022) | Drug Treatment Program | DTP Status Report | Download | |||||||||||||||||||||||
| July, 2022 | BC-CfE Drug Treatment Program Monthly Report (January 2022) | Drug Treatment Program | DTP Status Report | Download | |||||||||||||||||||||||
| June, 2022 | Celebrating 30 years of excellence |
This year the BC Centre for Excellence in HIV/AIDS (BC-CfE) is celebrating its 30th anniversary. Since its inception in 1992, the advancements made by BC-CfE staff and its international collaborators have transformed HIV from a rapidly progressing fatal disease, to a chronic and manageable illness that is highly, and easily, preventable. Given a provincial mandate by the Ministry of Health to "improve the health of British Columbians through the development, on-going monitoring and dissemination of comprehensive investigative and treatment programs for viral diseases," the BC-CfE built a centralized registry that served as a foundation to deliver on that mandate and more. This registry remains at the core of the BC-CfE's operations today and has enabled the research, monitoring and evaluation that sets the BC-CfE apart. Among the pivotal moments in BC-CfE history, the discovery and introduction of highly active antiretroviral therapy (HAART) ranks among the top. The widespread adoption of HAART following its worldwide introduction at the 1996 Vancouver International AIDS Conference was life-changing for those living with HIV/AIDS. Prior to HAART, the life expectancy of a 20-year-old person diagnosed with HIV was under 10 years. Following the implementation of HAART, life expectancy increased to more than 50 years. The groundwork for this revolutionary advancement was laid over a decade before the BC-CfE was officially established, when the outlook for people living with HIV/AIDS was quite bleak. In 1981, when HIV cases first appeared in North America, a group of dedicated healthcare providers at St. Paul's Hospital came together to tackle this mysterious illness and in 1986 formed a comprehensive primary care clinic and specialized research unit which is now known as the John Ruedy Clinic. Among this team, was Dr. Julio Montaner, current Executive Director and Physician-in-Chief of the BC-CfE, who arrived in Canada in 1981 to begin a career in respiratory medicine. As his pulmonary training coincided with HIV's emergence, little did he know that the clinical cases he would see and solve in the 1980s, would not only inform a 40-year career as one of the world's preeminent HIV/AIDS researchers, but also lead to his leadership of an organization devoted to improving and prolonging the lives of those living with HIV in British Columbia. After the effectiveness of HAART, the BC-CfE went on to help shape local and global policy with its Treatment as Prevention (TasP) strategy. In British Columbia, thanks to the BC-CfE's advocacy, the Seek and Treat for Optimal Prevention of HIV/AIDS (STOP HIV/AIDS) program was launched and successfully utilized TasP to improve HIV testing, linkage to care and treatment uptake. Adopted by the United Nations, Dr. Montaner was directly involved in shaping the TasP inspired policy that was the UNAIDS 90-90-90 target by 2020. The 90-90-90 target calls for 90 percent of people living with HIV to be diagnosed through testing, 90 percent of those diagnosed with HIV to be on ART treatment, and 90 percent of those on treatment to achieve sustained virologic suppression, which means they are unable to transmit HIV. BC exceeded this goal which has now become the 95-95-95 goal by 2025, which it is also expected to achieve. Throughout its three decades, research has been the driving force behind the numerous innovations and discoveries. The Clinical and Research Laboratory has developed and pioneered tests that have become the standard. An Epidemiological and Population Health program with a broad spectrum of research keeps advancing the expertise and stature of the BC-CfE. In addition to HIV/AIDS treatment, research and innovation, the BC-CfE has been a champion of numerous social causes, including a role in the fight for Insite, North America's first supervised injection site, that went to the Supreme Court of Canada (and won); advocating for decriminalization of drugs long before the current opioid overdose public health crisis; and fighting for special access for yet-to-be approved treatments for its patients along the way. Rather than rest on the remarkable achievements related to HIV/AIDS, the BC-CfE continued to apply its expertise with TasP to accomplish more. Implementing a pre-exposure prophylaxis (PrEP) program in 2018 to further reduce HIV incidence in BC; developing a wholistic, comprehensive approach to care for poorly reached and poorly engaged clients in Vancouver's Downtown East Side at its Hope to Health Research & Innovation Complex; and partnering with other health organizations to apply its expertise & lead quality improvement initiatives that share and apply the TasP strategy to other viral and social contagions are some examples of the extraordinary work that the BC-CfE has done and continues to do today. Over the coming months, the BC-CfE will be celebrating its anniversary through various events and publications featuring those who were a part of the story. Please join the BC-CfE in celebrating 30 years of excellence. Continue to visit our website and follow our social media channels as we thank our clients, the staff, numerous supporters, partners, and friends who've made our work possible. | Forecast Newsletter | Download | |||||||||||||||||||||||
| May, 2022 | BC-CfE's Thrive team awarded CAHR-CANFAR award |
Each year the Canadian Foundation for AIDS Research (CANFAR) and the Canadian Association for HIV Research (CAHR) present the CAHR-CANFAR Excellence in Research Awards. This year's award for Community-Based Research (CBR) was given to the Peer Research Associates (PRA) of the BC-CfE's Thrive team. Thrive was a BC-CfE led CBR study with a three-year duration and funded by the Canadian Institutes of Health Research (CIHR), focused on older adults living with HIV (OALHIV) accessing home and community care (HCC). Recognizing that OALHIV (i.e., over the age of 50) now constitute over 50 percent of all people accessing HIV treatment in BC and as they age, the need for supportive care in non-acute settings, including HCC, is increasing, the Thrive research study was created to better support people's ability to thrive during all stages of life. This honour is given to "highlight and celebrate the contributions of Canadian researchers in HIV/AIDS research in Canada and internationally", and demonstrates the power of perspective and insight gained by the Thrive team by speaking to, and learning from, those with lived/living experience. The PRA members of the Thrive team includes Sharyle Lyndon, Antonio Marante, Patience Magagula, and Claudette Cardinal. On winning the award, Sharyle Lyndon said, "What makes this research so valuable is that when we (HIV/AIDS long-term survivors) were diagnosed we were told to make our arrangements to die, not to prepare to get old. Many of us spent what we had (physically, emotionally, and financially) to do so with dignity, but also to help those that lived on past us." She added, "As I have learned and shared often, all the experiences I encounter—both good and bad—can be of help to others." Lyndon notes, "The Thrive project has allowed me to believe that my hopes for this to be true are seeing fruition. And my dream is that this research will continue and will fall into the hands of people in a position of power to make some, if not all, the necessary changes." In addition to her work as a Thrive PRA, Patience Magagula is also the founder of the Afro-Canadian Positive Network of BC, and has been on the board of directors and committees of organizations like the Pacific AIDS Network and Canadian Treatment Action Council. Upon arrival from South Africa as a refugee to Canada, Magagula had only recently been diagnosed. Her doctor at the time incorrectly told her it was a crime in Canada to not disclose one's HIV/AIDS status to sexual partners. This misinformation led to her believing that HIV/AIDS itself was illegal in Canada, and for years she kept her status to herself, as a shameful, and isolating, secret. About her work with Thrive, Magagula said, "I believe that our research works against institutional racism that heightens HIV transmission in marginalized communities. We'll achieve our goals to alleviate the challenges of fear, concerns, and worry that impacts people's lives." Claudette Cardinal identifies as a Cree Indigenous woman and connects her involvement with Thrive to the teachings of her late grandmother, who taught her to pray for the sick. On working with Thrive, she said, "Research is a natural extension of this desire to understand and to improve the world in which we live. Our connection to the Land reminds us we are all aging, and what better way to do that than connecting with our peers. The Thrive team has helped with working in collaboration with OALHIV, my peers, the community, and providers." Antonio Marante has been living with HIV for more than two decades. His role in Thrive was to help recruit participants and he found that he was able to do so successfully because of the shared experience of living with HIV. Speaking with someone who is also living with HIV enabled Thrive participants to open up more during interviews, and led to deeper sharing of their journeys of living with HIV while accessing HCC services. Marante said, "Even though Canada provides high standards in healthcare, HCC requires more attention from policymakers, such as providing more service hours for patients who require it, having a fair HCC assessment, and enabling healthcare provider collaborations." Currently, the Thrive team has wrapped up data collection, having interviewed OALHIV and providers. Thrive is now in the knowledge translation phase, sharing the findings with participants, AIDS service and community organizations, and through publications and conferences. Thrive is a relevant study that needs to continue because we have just touched the surface. Our small and mighty team worked together virtually during the pandemic, and we all learned how to thrive within the Thrive study. We need more advocacy to rekindle the fire within and create more spaces for older adults with HIV to live within. It was an honour to hear from all who shared with us. | Forecast Newsletter | Download | |||||||||||||||||||||||
| May, 2022 | Antiretroviral Adverse Drug Reaction Report form | To report a suspected adverse drug reaction (“side effect”) to an antiretroviral medication, download and complete the Antiretroviral Adverse Drug Reaction Report form and fax or mail it to the BC-CfE Pharmacovigilance Initiative (address shown on the top of the form). To learn more about HIV drug safety monitoring and adverse drug reaction reporting, click here. | Drug Treatment Program, Pharmacovigilance Initiative, Quality and Safety | Download | |||||||||||||||||||||||
| April, 2022 | BC-CfE brings innovative stimulant use disorder treatment to Downtown Eastside |
BC has been under a public health emergency due to drug-related overdoses for six years now. Of the 9,400 lives lost to illicit drug toxicity in the province in that time, most deaths have occurred due to opioids, specifically fentanyl. However, the use of stimulants such as cocaine and methamphetamine, and the harms associated with this use, have been steadily increasing across Canada, with BC the most affected province. Data from 2016-2018 shows polysubstance use is very common among overdose fatalities. 49 per cent of those who died from overdoses were found to have cocaine in their system and 31 per cent had amphetamines or methamphetamine. Stimulant use also imposes a significant burden on acute care health services through frequent emergency room visits and through psychiatric admissions due to stimulant-induced psychosis. Due to these harms, for both individuals and society, the BC Centre for Excellence in HIV/AIDS (BC-CfE), in partnership with Vancouver Coastal Health, applied to Health Canada to implement and evaluate an integrated program of contingency management and cognitive behavioural therapy (CBT) for people with stimulant use disorder (SUD) who need help to reduce use or abstain from using stimulants. The application was successful and participants will soon be recruited through the Hope to Health Research and Innovation Centre (H2H). Opened in late 2019, H2H provides harm reduction, supervised consumption, safer drug supply including injectable opioid agonist therapy and primary care services to residents of Vancouver's Downtown East Side (DTES). Despite being open for less than three years, demand for the programs offered at H2H has grown rapidly. DTES residents suffer the highest rate of death due to illicit drug overdoses in BC, and there is a striking 15-year disparity in life expectancy between DTES residents and residents of neighbouring areas. SUD is the second most common diagnosis among H2H's primary care clients. Many of the clients this program plans to recruit will be unstably housed or homeless, and also face other barriers to accessing care. Due to this, the BC-CfE will ensure that individuals with lived experience of SUD and challenges with homelessness will be actively involved in designing, implementing and evaluating the program through the H2H Client Advisory Committee. With 30 per cent of H2H clients self-identifing as Indigenous, researchers will also ensure that all individuals involved have completed Indigenous cultural competency safety training. It's hoped the program will be able to help up to 120 clients. The contingency management portion of the program will reward participants for achieving their health goals, whereas CBT helps participants learn and identify reasons for their substance use. Participants will work with counsellors to develop effective coping strategies to prevent or reduce future stimulant use by exploring the positive and negative consequences of continued drug use, self-monitoring to recognize cravings early, and identifying situations that might put one at risk for use. By using contingency management and CBT concurrently, researchers hope for longer-lasting psychological benefits. The project has three objectives. The first is to build an interdisciplinary team to implement an integrated program of contingency management and CBT at H2H, including a dedicated counsellor trained in CBT, a peer support worker, and a licensed practical nurse to administer the contingency management component. The second objective is to measure uptake, retention and completion of both program components. The third objective will be to measure stimulant and other illicit or prescribed drugs at enrollment, program exit, and one month after program completion and other important health outcomes. Succeeding at these three objectives, means BC-CfE researchers will be able to measure the uptake and completion of this program and determine if the contingency management component may also improve completion of CBT. The BC-CfE is forging a new path with this program. Several psychological or behavioural interventions have been demonstrated to be effective in reducing stimulant use. However, these methods have not been well studied among marginalized, unstably housed or homeless populations with polysubstance-use and mental health challenges, such as DTES residents. The experiences and data which will be collected from this project will directly provide evidence on the effectiveness of integrated stimulant use disorder treatment programs and the potential for further expansion of these services to reduce stimulant use in Vancouver and elsewhere. | Hope to Health Primary Care Clinic, Hope to Health Supervised Consumption Site (SCS) | Forecast Newsletter | Download | ||||||||||||||||||||||
| April, 2022 | BC-CfE CDET Statement on the use of COVID-19 vaccines in Persons Living with HIV | People living with HIV (PLWH) aged 5 years or older should be fully vaccinated for COVID-19, regardless of CD4 count provided that they do not have contraindications to the available age-appropriate vaccines (see below). Although the evidence was mixed in earlier studies, more recently, multiple large studies have indicated that PLWH are at increased risk of serious illness and death due to COVID-19. To date, there appears to be no significant difference in the safety profile of the authorized COVID-19 vaccines in PLWH compared to the general population. | Download | ||||||||||||||||||||||||
| April, 2022 | BC-CfE Drug Treatment Program Monthly Report (December 2021) | Drug Treatment Program | DTP Status Report | Download | |||||||||||||||||||||||
| March, 2022 | BOOST continues to improve lives for those living with opioid use disorder |
The BC Centre for Excellence in HIV/AIDS' (BC-CfE) QI team, led by Senior Medical Director Dr. Rolando Barrios, launched the Best-Practices in Oral Opioid agoniSt Therapy Collaborative (BOOST) in 2017 as a partnership between the BC-CfE and Vancouver Coastal Health. As BOOST grew, more than 40 healthcare teams across BC joined the Collaborative, which has since evolved into the BOOST QI Network. QI stands for quality improvement, and by operating under a quality improvement model the teams work together to help people living with opioid use disorder (OUD) overcome any barriers to treatment, and to provide the support needed to start, and consistently continue, using Opioid Agonist Therapy (OAT). This therapy provides treatments including prescribing buprenorphine, Slow Release Oral Morphine, and methadone to treat opioid dependency, reduce drug-related harms, support long-term recovery, and, most importantly, prevents death. Currently, an average of more than six people die every day in BC due to overdoses. Last year was the deadliest year yet of this province's overdose crisis, with 2,224 deaths, an increase of 26 per cent from 2020. It was back in the Spring of 2016 when overdoses due to illicit drugs became the leading cause of unnatural deaths in BC. This was when the province declared a public health emergency that continues to be in place. Since the start of the official public health emergency, there's been more than 8,800 overdose deaths. In fact, according to the B.C. Centre for Disease Control, drug toxicity comes second only to cancers in terms of total potential years of life lost (a measure of premature death) in our province. As a point of comparison, COVID-19 ranks 12th. The highly-potent opioid fentanyl, and its analogues, are now noted as a factor in about 84 per cent of overdose deaths in BC. Ten years ago, it was noted in only about five per cent of deaths. As this is the current reality, the BOOST QI Network is needed now more than ever. Doctors, nurse practitioners, social workers and mental health workers, which comprise the teams supporting those on OAT, need the latest and most helpful information they can possibly get. BOOST helps provide this information through its QI Network. The process of initiating and continuing on OAT can be overwhelming for many clients due to the need for frequent prescription pick-ups and follow-up healthcare appointments. Healthcare workers in the BOOST QI Network often provide much-needed daily check-ins with clients, and, thanks to the QI process, can learn the most effective ways for keeping their clients engaged in care and consistent with their individual requirements for OAT. BOOST's many learning events, which transitioned to virtual due to the COVID-19 pandemic, featured personal stories told by families and persons affected by or living with OUD. By listening to these families and their stories, and learning from people with direct experience of OUD, members of BOOST could improve their daily workflows to better serve their clients. The TasP strategy's emphasis on treatment has been embedded within the BOOST QI Network from the very start. And now, as the effects of the COVID-19 pandemic continue to significantly worsen BC's ongoing opioid crisis, the application of TasP to OUD is saving lives. People who use drugs in all parts of BC are currently facing an increasingly toxic drug supply when buying street drugs. COVID-19 has also increased unemployment, social isolation, and has exacerbated mental health and addiction issues. As evidence shows, a significant proportion of individuals with OUD will reduce illicit opioid use and remain in treatment longer with appropriate doses of OAT such as methadone, buprenorphine/naloxone or slow-release oral morphine. Other predictors of treatment success include a shorter time period from diagnosis of OUD to treatment, and a longer duration of treatment. By learning through, and growing, the BOOST QI Network, more teams will be able to provide equitable access to integrated, evidence-based care to help clients with OUD. The Collaborative's goals are to see 95 per cent of clients with an active OAT prescription, 95 per cent of those clients with an active OAT prescription retained on therapy for greater than three months, and 100 per cent of BOOST teams equipped with a process to monitor and incorporate the patient voice in their quality improvement work. Recently, the BOOST QI Network has had its funding extended for another year by Health Canada's Substance Use and Addictions Program. The new funding will go to Interior Health for a project called the Interior BOOST Collaborative. This project is slated to start in May of this year. As illicit drug toxicity increases, and as death tolls continually break records, continuing any and all efforts to save lives from OUD is essential. BOOST's key focus, retention of clients on Opioid Agonist Therapy (OAT), plays a critical role in saving lives. | Forecast Newsletter | ||||||||||||||||||||||||
| March, 2022 | BC-CfE Drug Treatment Program Monthly Report (November 2021) | Drug Treatment Program | DTP Status Report | Download | |||||||||||||||||||||||
| February, 2022 | Hope to Health's holistic approach improving lives in the Downtown Eastside |
Since opening in late 2019, the BC Centre for Excellence in HIV/AIDS' (BC-CfE) Hope to Health Research and Innovation Complex (H2H) has offered comprehensive health care to residents of Vancouver's Downtown Eastside. For H2H clients, holistic means a team of healthcare professionals, including doctors, nurses, social workers, and peer research associates, will help with not only medical care, but also in providing psychosocial supports. This can include helping clients find stable housing, income and social support, and providing behavioural interventions, like educating clients in safer substance use. Located on the 600 block of Powell Street, H2H is comprised of three buildings. At 625 Powell is the primary care clinic. When H2H opened the goal was for up to 1,400 clients with complex needs to have what is referred to as a "medical home". This concept means offering care centred on individual clients' needs, within their community, and integrated with other health services. By having a medical home, and by building a trusting relationship with clients, better health outcomes can be achieved. Clients who come in to H2H will be met by one of two Integrated Care Teams (ICT), which are both supported with shared clinical services, and one triage team, that determines the immediate needs of each client. The data shows the top diagnosis for H2H clients is Mental Health and Substance Use Disorders, whether that disorder is use of opioids, alcohol, or stimulants. The other diagnoses include chronic hepatitis C infection, hypertension, dyslipidemia (high cholesterol), and HIV. The philosophy of comprehensive care at H2H is summed up by the slogan of "Enroll, Engage and Empower". Enrolling clients at H2H has succeeded quickly and fully, with a client roster now standing at 1250, close to the original goal of 1,400. Engaging clients means they continue to see H2H as a place of consistency, where they trust their healthcare providers and are able to be honest about their medical needs without fear of judgment or stigma. Through the systematic method of Quality Improvement, the staff of H2H has decreased disengagement in care at H2H from 42 percent to 15 percent. Research has proven that increased engagement in care improves client outcomes and decreases the use of acute care, such as hospital emergency rooms. Empowering clients means they are able to set health goals for themselves and craft a care plan with their doctor to meet these goals. The latest available data from H2H shows the percentage of clients with documented health goals and a care plan is above 80 per cent. For clients with substance use issues, empowerment may mean that they want to stop using street drugs and be prescribed a safer supply. Doctors at H2H can help with this goal by offering opioid agonist therapy (OAT), proven to be an effective treatment for illicit opioid use. OAT involves a client switching from dangerously toxic drugs acquired illegally, to taking the opioid agonists methadone, buprenorphine (Suboxone®) or slow-release oral morphine. These prescribed medications help to prevent withdrawal and reduce cravings for opioids. OAT helps H2H clients stabilize their lives and greatly reduces drug use related harms. For clients who continue to use illicit drugs, the H2H building at 611 Powell features a Supervised Consumption Site where clients can bring in their own substances and use them under the supervision of trained staff. By using brand new needles, clean water, and being in a stigma-free indoor space, clients injecting their drugs are considerably safer than if they were using outdoors. Those using at the safer consumption site are also at far less risk of suffering a fatal overdose, as the nurses supervising them will act quickly to reverse overdoses should they occur. In a time of record high drug-related deaths, there has not been a single fatal overdose at H2H. At 647 Powell the H2H on-site laboratory is led by Dr. Zabrina Brumme. The laboratory tests client's blood samples to monitor genetic changes in viruses within their bodies, which could lead to more effective tailored therapy. Other testing includes therapeutic drug level monitoring, an important tool for investigating drug absorption, treatment adherence, toxicities, and side-effects. Opportunities to support the work at 625 and 611 Powell are being explored by the laboratory to further personalize and enhance client care. Dr. Rolando Barrios is the BC-CfE's Senior Medical Director and has worked in the Downtown Eastside for decades. As the lead physician of H2H, Dr. Barrios said, "Enrolling, engaging and empowering clients at H2H isn't just a slogan. The staff at H2H truly work hard to help our clients realize their own health goals. | Hope to Health Primary Care Clinic, Hope to Health Supervised Consumption Site (SCS), Laboratory | Forecast Newsletter | Download | ||||||||||||||||||||||
| February, 2022 | HIV Monitoring Semi-Annual Report, Fourth Quarter 2021 |
| STOP HIV/AIDS | ||||||||||||||||||||||||
| February, 2022 | BC-CfE Drug Treatment Program Monthly Report (October 2021) | Drug Treatment Program | DTP Status Report | Download | |||||||||||||||||||||||
| February, 2022 | BC-CfE Guidelines for the use of Paxlovid® and ARVs | Safety considerations for nirmatrelvir/ritonavir (Paxlovid¨) use in persons living with HIV whether or not on antiretroviral treatment, or persons at risk of HIV while on PrEP who are diagnosed with COVID-19 infection The COVID-19 therapy Paxlovid¨ consists of the antiviral medication nirmatrelvir co-packaged with the pharmacokinetic enhancer (âboosterâ) ritonavir, taken as a twice daily, oral, five-day treatment course, with dosage adjustment required for renal impairment (see prescribing information). Nirmatrelvir/ritonavir treatment is initiated as soon as possible following a positive SARS-CoV-2 test result. Eligibility criteria for nirmatrelvir/ritonavir vary between Canadian provinces and will likely evolve over time. Also, eligibility in British Columbia may be expanded as drug supply increases. Therefore, prescribers are strongly encouraged to refer to current nirmatrelvir/ritonavir prescribing information and local guidelines for treatment eligibility and general contraindications/precautions. In British Columbia, see the BC Centre for Disease Control website: http://www.bccdc.ca/health-professionals/clinical-resources/covid-19-care/clinical-care/treatments | Pharmacovigilance Initiative | Download | |||||||||||||||||||||||
| December, 2021 | BC-CfE Drug Treatment Program Monthly Report (September 2021) | Drug Treatment Program | DTP Status Report | Download | |||||||||||||||||||||||
| December, 2021 | BC's success story shows strength of Treatment as Prevention |
On December 1st we celebrate World AIDS Day, an opportunity to reflect on our challenges and successes four decades into the battle against HIV/AIDS. Around the world there are nearly 38 million people living with HIV and about 1.5 million new infections per year. A recent report by the World Health Organization estimates the number of people with the virus being treated with antiretrovirals had risen to 27.5 million – an increase of almost 10% over the last year. Encouraging but not enough. In BC, we have much to be proud of given the success of the BC Centre for Excellence in HIV/AIDS' (BC-CfE) Treatment as Prevention (TasP) strategy on the impact of HIV/AIDS, here and globally. On last year's World AIDS Day, we were proud to announce, alongside BC's Minister of Health Adrian Dix, that our province had surpassed the United Nations' 90-90-90 Target; with 92 per cent of people living with HIV in BC diagnosed, 91 per cent of them on highly active antiretroviral therapy (HAART), and 95 per cent of those on HAART (approximately 7,500 people) achieving virological suppression, meaning they have undetectable levels of HIV in their blood and bodily fluids. Reaching these thresholds has played a key role in reducing AIDS related morbidity and mortality in BC by over 90% since the peak of the epidemic in the early 90's. Furthermore, this success has also greatly reduced the likelihood of new HIV cases in BC, because people living with HIV who are virologically suppressed through HAART do not transmit the HIV virus. Since January 2018, BC further expanded its HIV control efforts by adding fully subsidized pre-exposure prophylaxis (PrEP) to the TasP strategy. PrEP involves one pill (containing two specific antiretroviral drugs) taken daily by individuals who are at increased risk of contracting HIV, based on a set of pre-defined criteria. Daily use of PrEP reduces the risk of acquiring HIV by over 95%. Today, the BC-CfE's PrEP program has over 4,700 active participants across all of BC's health authorities, and is among the largest in Canada and, indeed, the world. As a result of the combined impact of HAART and PrEP, BC is on track to see its lowest number of new HIV infections over three decades in 2021, at approximately 120 cases (a 20% decrease from the previous year). This proves once again that sustained investments in TasP (a strategy first proposed by the BC-CfE 15 years ago, and since widely adopted around the world) stops progression of HIV infection to AIDS, avoids premature deaths, and prevents HIV transmission, all within a cost-averting framework. Continued fostering of BC's fully subsidized HAART and PrEP programs, with adequate support and full involvement of all relevant stakeholders, will be critical to ensuring the long-term success of BC's anti-HIV/AIDS strategy. The disruptions created by the COVID-19 pandemic illustrate this point. It has been widely reported that measures needed to address COVID-19, particularly lockdowns early in the epidemic, impacted nearly all aspects of everyday life as well as access to health care services. HIV care was no exception. The BC-CfE documented decreases in laboratory monitoring and access to HAART and PrEP in the first phase of the epidemic. These trends were confirmed with data from a survey of Vancouver's gay and bisexual men whereby 33 per cent of participants reported avoiding health services because of concerns about COVID-19 exposure. However, prompt implementation of corrective measures allowed for these trends to be reversed within weeks without ill effects. Earlier this year the United Nations called for a redoubling of the global efforts to "End AIDS as an epidemic by 2030", defined as decreasing AIDS-related mortality and new HIV infections globally by 90%, using 2010 as the baseline. The campaign was launched in 2015 with a goal of reaching the BC-CfE-proposed 90-90-90 Target by 2020. However, by the end of 2020, most of the world had failed to meet the UN 90-90-90 Target for a variety of reasons, including weak political leadership, insufficient investments, and emerging challenges posed by COVID-19. As a result, UNAIDS estimates the failure to meet the 90-90-90 Target led to an additional one million AIDS-related deaths, and three million new HIV infections globally. Despite these shortcomings, the United Nations successfully challenged the international community to expand the global effort by embracing the 95-95-95 by 2025 Target, as originally proposed by the BC-CfE. UNAIDS estimates that by meeting the 95-95-95 Target the number of people newly infected with HIV will fall from 1.7 million in 2019 to 370,000 by 2025, and the number of people dying from AIDS-related illnesses would be reduced from 690,000 in 2019 to 250,000 in 2025. "Ending AIDS as an epidemic by 2030" remains within reach. The question remains whether we have the political will and focus to deliver on the promise of the BC-CfE proven TasP strategy at a global level. On this World AIDS Day, we encourage every British Columbian to join the BC-CfE as we commit to do our part to motivate our political leaders find the courage and resources to deliver on this promise. To not do so would represent an inexcusable failure. Julio Montaner, OC, OBC, MD | CANOC, Laboratory, Momentum, SHAPE Study | Treatment as Prevention® | Forecast Newsletter | Download | |||||||||||||||||||||
| December, 2021 | BC-CfE Drug Treatment Program Monthly Report (August 2021) | DTP Status Report | Download | ||||||||||||||||||||||||
| December, 2021 | PrEP Semi-Annual Report for British Columbia - Second Quarter 2021 | PrEP | PrEP Quarterly Report | Download | |||||||||||||||||||||||
| November, 2021 | Collaborative study examines COVID-19 vaccine immune responses in people living with HIV |
BC Centre for Excellence in HIV/AIDS (BC-CfE) researchers, collaborating with counterparts at Simon Fraser University, the University of BC, Providence Health Care and the CIHR Canadian HIV Trials Network (CTN) recently published a study looking at COVID-19 vaccine immune responses in people living with HIV (PLWH). Due to the explosive growth of COVID-19 variants, and the ongoing discussion about third vaccine shots and their necessity, the researchers released their findings earlier than originally planned. The need to expedite the research was also spurred by the timeline for decisions regarding additional COVID-19 vaccine doses for some key populations in BC including PLWH. By providing local data, the collaborative hoped to generate data that would assist decision-makers. Titled, "Humoral immune responses to COVID-19 vaccination in people living with HIV receiving suppressive antiretroviral therapy", the publication is currently in its pre-print stage pending peer review. The study recruited 100 people living with HIV, all of whom were on suppressive antiretroviral therapy and where 98% of this group had a CD4+ T cell count greater than 200 cells/mm3, (a CD4+ T cell count below 200 cells/mm3 is an indicator of immunodeficiency). The study also recruited 152 individuals without HIV, ranging from 22 to 88 years of age, as a control group. Participants provided blood samples prior to COVID-19 vaccination, if feasible, one month after the first vaccine dose, and one month after the second dose. The researchers measured the levels of circulating antibodies against the receptor-binding domain (RBD) of the SARS-CoV-2 spike protein, the ability of these antibodies to disrupt the interaction between RBD and its cellular receptor ACE2, and the ability of these antibodies to block infection of cells by SARS-CoV-2, the virus that causes COVID-19, after one and two doses of COVID-19 vaccine. Study results indicated that after a single COVID-19 vaccine dose, and after accounting for sociodemographic, health and vaccine-related variables, the antibody responses to COVID-19 vaccines in people living with HIV were lower than those of controls, although the magnitude of this difference was relatively modest. However, after two COVID-19 vaccine doses, this effect disappeared. That is, after two doses of COVID-19 vaccine, the antibody responses of people living with HIV were comparable to those of controls. The study found that, rather than HIV, older age, a higher number of chronic health conditions, and having received two doses of the AstraZeneca vaccine (as opposed to a mixed or dual mRNA vaccine regimen), were the most significant correlates of weaker antibody responses after two doses. Importantly, among PLWH the researchers observed no significant relationship between either their most recent nor their lowest ever recorded CD4+ T-cell counts and responses to COVID-19 vaccination following two vaccine doses. This indicates that, for PLWH who are currently receiving suppressive antiretroviral therapy, having had low CD4+ T-cell counts in the past will not necessarily compromise their immune responses to COVID-19 vaccines presently. In concluding their study, the researchers interpreted the results as suggesting that PLWH whose viral loads are well-controlled on antiretroviral therapy and whose CD4+ T-cell counts currently are in a healthy range should generally not require a third COVID-19 vaccine dose as part of their initial immunization series. The study notes how other factors such as older age, co-morbidities, type of initial vaccine regimen and durability of vaccine responses will influence when PLWH may benefit from additional doses. The researchers also emphasize that the study's findings may not be generalizable to PLWH who are not receiving treatment and/or whose CD4+ T-cell counts are currently less than 200 cells/mm3, and that further studies of these groups are needed. Dr. Zabrina Brumme, the BC-CfE Laboratory Director and the lead author of this study, said "In the coming weeks and months, we will be continuing this study to monitor the durability of these responses, and we look forward to sharing additional results as they come in" This study was made possible through funding from Genome BC, the Michael Smith Foundation for Health Research, the BCCDC foundation for Public Health, the Canada Foundation for Innovation and the Public Health Agency of Canada through the COVID-19 Immunity Task Force. It is also part of a pan-Canadian study of immune responses in PLWH headed by Dr. Aslam Anis of the CIHR Canadian HIV Trials Network. The views expressed in this publication are those of the researchers and not necessarily those of the funding agencies. | CHIWOS, Epidemiology and Population Health, Laboratory | Forecast Newsletter | Download | ||||||||||||||||||||||
| November, 2021 | BC-CfE Drug Treatment Program Monthly Report (July 2021) | DTP Status Report | Download | ||||||||||||||||||||||||
| November, 2021 | BC-CfE Drug Treatment Program Monthly Report (June 2021) | DTP Status Report | Download | ||||||||||||||||||||||||
| October, 2021 | Improving patient engagement and retention in healthcare at Hope to Health |
A BC Centre for Excellence in HIV/AIDS (BC-CfE) research team is working to evaluate how a new primary care clinic can keep clients engaged in health care among residents of Vancouver's Downtown East Side (DTES). The "Hope to Health Engagement and Retention Evaluation (HERE) Study" is being conducted from the Hope to Health (H2H) Research and Innovation Centre located on Powell Street. Opened in late 2019, the Research and Innovation Centre was developed with an integrated, team-based approach to primary health care, based on the best evidence for service design in engaging under-served and marginalized urban core populations. The DTES is one of the lowest income neighbourhoods in Canada with median household incomes of approximately $23,000 and is characterized by high levels of homelessness and unstable housing. The population of the DTES is heavily overrepresented by people living with mental illnesses and substance use disorders, as well as pervasive trauma and structural violence. Other chronic medical conditions, including HIV and HCV infection, are hyper-endemic with prevalence estimates of 30% and 70% respectively. DTES residents have also been greatly impacted by the opioid crisis, with the highest rate of death due to illicit drug overdoses in BC, at over 100 deaths/100,000 population. There is a striking 15-year disparity in life expectancy between residents of the DTES and residents of neighbouring areas of Vancouver. DTES residents often rely on DTES community health centres (CHCs), or clinics outside of the neighbourhood in order to access primary healthcare services, as there are very few family-practice or walk-in clinics in the area. However, CHCs face tremendous challenges in engaging and retaining clients with complex medical and psychiatric needs, a challenge made even more difficult by limited capacity to enroll new clients. As such, many DTES residents predominantly access health care through emergency services at one of the three hospitals in central Vancouver. Following hospital care, many patients discharged do not have an identified primary healthcare provider, which leads to limited outpatient follow-up and frequent re-admission. Recent estimates from Vancouver Coastal Health (VCH), suggest that about 7,500 residents of the DTES are unattached or poorly attached to clinical services. The relatively recent establishment of the BC-CfE's H2H Primary Care Clinic and the HERE Study represents an extraordinary opportunity to address these pervasive health systems gaps affecting DTES residents. Dr. David Moore, the Principal Investigator of the study and a clinician at H2H noted, "This H2H Primary Care Clinic provides an ideal environment for clinicians, researchers and members of the community to study ways to better engage DTES residents in effective primary health care." The HERE Study will be using the WelTel mobile health intervention platform. WelTel is designed to be patient-centered, empowering people to manage their own health needs and take part in their healthcare decisions via a two-way automated check-in text messaging system. BC-CfE clinicians and researchers with the HERE Study will adapt the WelTel platform and experience, capitalizing on substantial in-kind donations of 1,400 refurbished mobile phones and data plans through Telus' Mobility for Good program for the specific needs of the DTES population. The HERE study represents a critical opportunity to gather the detailed data required to evaluate interventions specific to this unique client population, and allows researchers to share lessons learned with providers serving similar clients in urban settings across Canada. | Clinical Education & Training, Epidemiology and Population Health, Hope to Health Primary Care Clinic, Laboratory | Forecast Newsletter | Download | ||||||||||||||||||||||
| October, 2021 | PrEP Enrolment & Prescription Request Form | PrEP | PrEP Documents and Forms | Download | |||||||||||||||||||||||
| September, 2021 | BC-CfE Drug Treatment Program Monthly Report (May 2021) | DTP Status Report | Download | ||||||||||||||||||||||||
| September, 2021 | BC-CfE updates its Primary Care Guidelines |
The BC Centre for Excellence in HIV/AIDS (BC-CfE) created the first edition of its Primary Care Guidelines for the Management of HIV/AIDS in Adults in British Columbia back in 2011. Now, 10 years later, thanks to the diligent work of the Primary Care Guidelines Working Group (a working group appointed by the Committee for Drug Evaluation and Therapy), the most recently updated version of the guidelines is now available for health care providers throughout the province to become more actively involved in the diagnosis and care of people living with HIV (PLWH). The Primary Care Guidelines play a key role in the BC-CfE's ongoing commitment to providing the most current information and research regarding the management of HIV. The guidelines were developed by consensus amongst a committee of experts, based on interpretation of current best practices for the primary care of PLWH and related conditions. An expert committee composed of primary care and infectious disease physicians, a nurse practitioner, a pharmacist, and a person living with HIV prepared the original guidelines in 2011. Since then, the guidelines have been consistently reviewed and revised to ensure the information and advice provided is as current and up-to-date as possible. This summer saw the most recent review of the guidelines by a working group consisting of family, public health, and infectious disease physicians, and a peer navigator. The working group updated epidemiological information, baseline assessment and investigations, immunization recommendations, as well as issues related to co-morbidities and the health of women and transgender individuals. Specialty topics were reviewed by experts on the matter. Thankfully, today, HIV infection is no longer a death sentence. Due to effective antiretroviral drug regimens, HIV is now seen as a chronic manageable medical condition. Early diagnosis and initiation of antiretroviral therapy (ART) has dramatically improved the management of HIV infection and has led to substantial reductions in HIV-related morbidity and mortality. Research shows that a 20-year-old living with HIV and receiving ART in the U.S. or Canada can expect to live into their early 70s, a life expectancy approaching that of the general population. In addition, there is now clear evidence that the widespread use of ART prevents HIV transmission. Even after repeated sexual exposures without using condoms, PLWH who are receiving ART and who have maintained a very low plasma HIV viral load do not transmit HIV. This is true for both heterosexual couples and men who have sex with men. However, in order for ART to be effective to the point where PLWH cannot transmit HIV, individuals must be fully engaged in care, right from an initial assessment to long-term retention in care and virologic suppression. This concept, which stems from the BC-CfE's strategy of Treatment as Prevention (TasP), is known as the HIV Cascade (or Continuum) of Care. The HIV Cascade of Care is the framework for assessing progress in HIV care and treatment in BC. Following these strategies has led to BC being one of the few jurisdictions in the world which has successfully surpassed the 90-90-90 UNAIDS target for 2020: 90% of people living with HIV (PLWH) in BC being diagnosed, 90% of those diagnosed receiving ART, and 90% of those on ART having an extremely low HIV viral load. As of the latest estimates, BC stands at 92%, 91%, and 94% on each respective benchmark. Studies suggest that as many as 50% of HIV transmission events may occur from people who are in the acute and very early stages of illness. This means early detection and diagnosis of HIV infection is absolutely critical in preventing further transmission. The BC-CfE's Primary Care Guidelines for the Management of HIV/AIDS in Adults in British Columbia helps all British Columbians, not just those living with HIV, by providing practical and easily accessible information and resources for primary care providers. Dr. Silvia Guillemi, Clinical Advisor with the BC-CfE and Primary Care Guideline Working Group member and contributing author, said, "We are proud to release the latest revised version of the BC-CfE's Primary Care Guidelines for the Management of HIV/AIDS in Adults in British Columbia. The Primary Care Guidelines working group reviewed the most up-to-date data on the primary care of PLWH, and these guidelines were developed with the support of the BC-CfE Clinical Education team. We are thankful for the contributions of experts on special topics like women and transgender health, and to the BC family physicians and nurse practitioners that reviewed and provided feedback for these guidelines." | Epidemiology and Population Health, Hope to Health Primary Care Clinic, Therapeutic Guidelines Committee | Forecast Newsletter | Download | ||||||||||||||||||||||
| August, 2021 | HIV Monitoring Semi-Annual Report, Second Quarter 2021 |
| STOP HIV/AIDS | ||||||||||||||||||||||||
| August, 2021 | BC-CfE researchers attend world's most influential meeting on HIV research |
The 11th International AIDS Society (IAS) Conference on HIV Science took place from July 18th to the 21st and BC-CfE researchers attending the virtual conference used the opportunity to present their latest findings. Taking place virtually from Berlin, IAS 2021 saw around 6,000 participants and opened with remarks from German Chancellor Angela Merkel and included a panel discussion on the COVID-19 and HIV pandemics with global health experts including Dr. Anthony Fauci, the director of the U.S. National Institute of Allergy and Infectious Disease. IAS 2021 saw conference delegates showcase the latest advances in basic, clinical and operational HIV research. The virtual setting allowed the global community of scientists, activists, and policy makers to convene safely during the COVID-19 pandemic. On the topic of Treatment as Prevention, multiple sessions showcased the latest research on PrEP usage, its monitoring, and creating personalized care. Other discussions centered on the benefits and drawbacks of long-acting injectables and antiretroviral-containing vaginal rings. In social and behavioural science presentations, global experts reflected on HIV service delivery systems in Zambia, community-led quality improvement programs in Vietnam, and improvements in viral suppression in Uganda. Several studies presented examined the intersection of the HIV and COVID-19 pandemics, such as evidence from Uganda showing how women face increased risk of gender-based violence and HIV during COVID-19 lockdowns. And as issues of COVID-19 vaccine uptake continue to dominate headlines around the world, IAS presenters discussed HIV vaccine innovation. One presentation on HIV vaccines looked at potential implications for future vaccine development if current candidates fail. Rachel Miller, a Graduate Student in the BC Centre for Excellence in HIV/AIDS (BC-CfE) Molecular Epidemiology and Evolutionary Genetics Group, won a scholarship to attend IAS 2021. She also won the prestigious annual "International AIDS Society and Merck Sharpe & Dohme Prize for Operational and Implementation Research in Differentiated Service Delivery" for her abstract titled "SARS-CoV-2 Lockdown Associated with Expansion of HIV Transmission Clusters Among Key Populations". The prize recognizes "outstanding research that addresses key knowledge gaps and links new evidence to strategic programme priorities in differentiated service delivery". Miller's award winning abstract, which includes Dr. Julio Montaner (BC-CfE Executive Director and Physician-in-Chief) and Dr. Jeffrey Joy (BC-CfE Research Scientist specializing in evolutionary genetics and bioinformatics) as senior co-authors, represents the combined efforts of the BC-CfE as a whole, and showcases the strengths of the BC-CfE's partnerships across health authorities and agencies. It brought together researchers from the BCCDC, Vancouver Coastal Health, the Faculty of Health Sciences at Simon Fraser University, and the Bioinformatics Program and the Department of Medicine at the University of British Columbia. Within the BC-CfE, Miller worked with the Molecular Epidemiology and Evolutionary Genetics Group, the Laboratory Program, and the HIV Drug Treatment Program. The research examined how COVID-19 related public health guidelines potentially introduced barriers to care and services for people living with, or at risk of acquiring HIV. Researchers synthesized available data from BC's HIV programs together with publicly available data to test SARS-CoV-2 related impacts on HIV transmission over the last year. Following the implementation of lockdown restrictions in late March 2020, there were statistically significant declines in antiretroviral therapy ART initiation, pre-exposure prophylaxis (PrEP) prescriptions, plasma viral load tests, HIV testing episodes, and new HIV diagnoses. Thankfully, the declines seen for nearly all of these metrics rebounded within the following three months, although below pre-lockdown levels. Phylogenetic analyses revealed increased growth and increases in multiple indicators of transmission events in a limited number of clusters involving people who inject drugs, relative to clusters characterized by gbMSM populations. The difference in level of transmission seen between these groups may be due to differences in how the impact of the restrictions varies by population. For example, while the gbMSM population likely experienced unprecedented decreases in level of contact as a result of restrictions, people who inject drugs likely experienced reduced access to services like supervised consumption sites and harm reduction supplies. The increased HIV transmission, though limited, shows the need for innovative and targeted solutions to offset potential negative impacts of COVID-19, or any pandemic-related lockdowns on HIV treatment and prevention efforts. | Hope to Health Primary Care Clinic, Laboratory, Viral Hepatitis Research Program (VHRP) | Harm Reduction, Hepatitis, Treatment as Prevention® | Forecast Newsletter | Download | |||||||||||||||||||||
| August, 2021 | BC-CfE Drug Treatment Program Monthly Report (April 2021) | Drug Treatment Program | DTP Status Report | Download | |||||||||||||||||||||||
| August, 2021 | BC-CfE Drug Treatment Program Monthly Report (March 2021) | Drug Treatment Program | DTP Status Report | Download | |||||||||||||||||||||||
| August, 2021 | BC-CfE Pharmacovigilance 2020 Annual Report | Pharmacovigilance Initiative, Quality and Safety | Download | ||||||||||||||||||||||||
| July, 2021 | PrEP Quarterly Report for British Columbia - Fourth Quarter 2020 | PrEP | PrEP Quarterly Report | Download | |||||||||||||||||||||||
| July, 2021 | BC-CfE and Vancouver Coastal Health Collaborate on new Treatment Optimization of Psychosis (TOP) Collaborative |
The Treatment Optimization of Psychosis (TOP) Collaborative officially launched on Wednesday, June 23rd. TOP is a quality improvement initiative led by the BC Centre for Excellence in HIV/AIDS (BC-CfE) in partnership with Vancouver Coastal Health's (VCH) Mental Health and Substance Use Services. TOP aims to systematically share, measure and implement best practices in the treatment of psychosis in community settings rather than in hospitals. Teams from across the VCH region will come together to achieve similar goals over the course of 12 months – connecting people living with psychosis with the best possible treatment, care and monitoring in their own communities, while raising awareness of effective clozapine treatment. Clozapine is the only treatment approved by Health Canada for people who live with treatment-resistant psychosis (TRS). Compared with other medications, clozapine is about twice as likely to succeed in reducing their symptoms. However, a small percentage of people may have side effects and require extra supports. TOP is designed to help teams develop the expertise to offer this treatment to all clients who could benefit from it. The TOP team noticed how this medication was severely underutilized in BC compared to other jurisdictions and seeks to change this. For example, in Australia and New Zealand clozapine usage is estimated to be about 30% in TRS, but only 17% in BC. Bob Chapman, Interim Vice President of Vancouver Community for VCH said, "We know that many people living with mental health challenges often receive other treatments before the ideal treatment option. This quality improvement initiative will bring greater awareness of the efficacy and safety of medication and help to ensure that health-care practitioners can best support their clients who may benefit from optimized treatment options." With nearly 80% of adults in BC having at least one dose of COVID-19 vaccine, and more than one million people in BC fully vaccinated, the COVID-19 pandemic in BC is hopefully nearing its end. However, those living with mental health challenges suffered disproportionately negative impacts throughout the pandemic as physical distancing, isolation, and instability in work and relationships took their tolls. The new ambitious goal thus became known as the UN 90-90-90 Target. By the end of 2020, B.C. and a few other jurisdictions around the world had met or surpassed the target, with consequent significant favourable impact on their respective rates of AIDS related morbidity/mortality as well as HIV transmission. The original plan called for the UN 90-90-90 Target to become the UN 95-95-95 Target as of the end of 2020. In the VCH region, psychosis is the number one cause of readmission to acute psychiatry within 30 days of discharge. TOP has the potential to improve the health of individuals and decrease the use of acute care as research indicates that for appropriately selected patients, clozapine is associated with 18.6 fewer inpatient days per year per client treated. Hon. Sheila Malcolmson, BC Minister of Mental Health and Addictions said, "For too long, it's been hard for people experiencing psychosis to access care. This new training program will improve care and treatment, and might reduce the need for hospital care. I am grateful for Vancouver Coastal Health and the BC Centre for Excellence in HIV/AIDS, supporting families and people living with psychosis." TOP's origins are rooted in the experiences and accomplishments of the Treatment as Prevention (TasP) strategy pioneered by the BC-CfE. TasP created a legacy of health-system improvement in B.C. through programs such as the Seek and Treat for Optimal Prevention HIV/AIDS Program and the BOOST Collaborative (Best-Practices in Oral Opioid agoniSt Therapy). The TOP Collaborative will follow the same approach in its implementation to shift initiation of psychiatric care from hospital to community settings; build capacity at each participating community mental health and substance use team in the VCH region; and improve the quality of care for clients living with psychosis. The scope of TOP is large, as all VCH community adult mental health and substance use teams, Assertive Community Treatment, and Early Psychosis Intervention teams will be included in the collaborative. This means Strathcona, West End, Kitsilano, South, North East, Grandview-Woodlands, Ravensong, Early Psychosis Intervention, Vancouver Coastal Assertive Community Treatment teams, and Sechelt Mental Health and Addiction Services will each send several delegates for learning events and have these delegates disseminate the knowledge they gain. TOP participants will take part in eight continuing medical education events for physicians, clinical staff, and administrative support staff; TOP learning sessions, focused on how to create and sustain clinical changes; action periods where information learned is implemented; and four one-hour webinars focused on topics covered in the learning sessions. Hardeep Thind, Coastal Regional Manager, British Columbia Schizophrenia Society said, "it's really important for families to have good, accurate information – I believe providing this training will assist frontline staff and help them be more confident in sharing information on clozapine." | Laboratory, Momentum, RETAIN, STOP HIV/AIDS | Forecast Newsletter | Download | ||||||||||||||||||||||
| July, 2021 | BC-CfE Pharmacovigilance 2019 Annual Report | Pharmacovigilance Initiative, Quality and Safety | Download | ||||||||||||||||||||||||
| June, 2021 | UNAIDS calls for greater focus on ending inequalities to end AIDS with new 95-95-95 Target |
In 2014, an ambitious new strategy was developed, under the leadership of BC Centre for Excellence in HIV/AIDS (BC-CfE) Executive Director & Physician-in-Chief Dr. Julio Montaner with the support of the BC-CfE, under the auspices of the United Nations Joint AIDS Program (UNAIDS). This was formally endorsed by UNAIDS after extensive international consultations. The new strategy had the specific goal of ending AIDS as an epidemic concern by 2030, defined as decreasing AIDS related mortality and HIV new infections globally by 90% using 2010 as the baseline. The short-term goal of the strategy was to ensure that at least 90% of people living with HIV (PLHIV) were diagnosed, at least 90% of those diagnosed were on antiretroviral therapy (ART), and at least 90% of those on ART were virally suppressed (meaning they cannot transmit the virus) by the end of 2020. The new ambitious goal thus became known as the UN 90-90-90 Target. By the end of 2020, B.C. and a few other jurisdictions around the world had met or surpassed the target, with consequent significant favourable impact on their respective rates of AIDS related morbidity/mortality as well as HIV transmission. The original plan called for the UN 90-90-90 Target to become the UN 95-95-95 Target as of the end of 2020. Of note, by World AIDS Day, Dec. 1st 2020, the BC-CfE was proud to announce, alongside BC's Minister of Health Mr. Adrian Dix, that BC had surpassed the 90-90-90 Target, with an estimated 92% of PLHIV in BC diagnosed, 91% of them on ART, and 95% virally suppressed; and as a result BC had decreased AIDS related morbidity and mortality by over 90% and HIV new infections by over 85%. This provided tangible proof that the strategy works as originally intended. However, as of the end of 2020 most of the world had failed to met the UN 90-90-90 Target. Regrettably, the were a number of factors that contributed to this, most notably insufficient international political leadership, flattening of global investments following the 2008 economic crisis, and more recently the COVID pandemic, Failing to meet the UN 90-90-90 Target by 2020 created significant anxiety in the field, as well as considerable concern regarding next steps. The new report, titled Addressing inequalities and getting back on track to end AIDS by 2030, details how the global HIV response which was unfortunately already off track in 2019, has been further undermined by COVID-19. Currently, 38 million people are living with HIV and more than 12 million people are awaiting life-saving HIV treatment. In the report, UN Secretary-General Guterres calls for enhanced global solidarity to close the HIV resource gap and increase annual HIV investments in low and middle-income countries to $29 billion (USD) by 2025 with a renewed aim to achieve the UN 95-95-95 Target globally. "It is imperative to break out of an increasingly costly and unsustainable cycle of achieving some progress against HIV but ultimately not enough to bring about an end to the pandemic," said Guterres in the report. "Inequalities are the key reason why the 2020 global targets were missed. By ending inequalities, transformative outcomes can be achieved for people living with HIV, communities and countries." The United Nations General Assembly High-Level Meeting next month will be a key moment for Member States like Canada to recommit towards the goal of ending the AIDS epidemic as a global public health threat. As UNAIDS Executive Director Winnie Byanyima said, "No country can defeat the colliding pandemics of HIV and COVID-19 on its own. Such global challenges can only be defeated through global solidarity and shared responsibility." Canada's Federal Minister of Health Hon. Patty Hajdu voiced her support for the targets saying "We remain committed to our 95-95-95 targets, moving toward reconciliation with Indigenous peoples, and to reducing stigma and discrimination. By bringing together domestic and international partners, we can redouble our collective efforts to improve the health of all our citizens and finish the fight against HIV and AIDS." "Ending AIDS as a public health threat by 2030 is still within reach—many countries are showing that rapid progress against HIV is possible when evidence-informed strategies and human rights-based approaches are adopted," said Byanyima. "But it requires bold political leadership to challenge and address the social injustices and inequalities that continue to make certain groups of people and entire communities highly vulnerable to HIV infection." | Forecast Newsletter | Download | |||||||||||||||||||||||
| June, 2021 | BC-CfE Drug Treatment Program Monthly Report (February 2021) | DTP Status Report | Download | ||||||||||||||||||||||||
| June, 2021 | BC-CfE Drug Treatment Program Monthly Report (January 2021) | Drug Treatment Program | DTP Status Report | Download | |||||||||||||||||||||||
| April, 2021 | BC-CfE awarded the 2020 Doctors of BC's Excellence in Health Promotion Award |
The BC Centre for Excellence in HIV/AIDS (BC-CfE) is the winner of the 2020 Doctors of BC's Excellence in Health Promotion Award – Non-Profit category. Dr. Ian Gillespie, Chair on the Council on Health Promotion, said, "We felt that the BC-CfE's Treatment as Prevention (TasP) initiative exemplifies Excellence in Health Promotion by advocating for widespread HIV testing and providing access to free HIV treatment for all medically eligible HIV-positive individuals." Doctors of BC is a voluntary association of 14,000 physicians, residents and medical students working together to, "promote a social, economic, and political climate in which members can provide British Columbians with the highest standard of health care." On the awards, the organization says, "These awards are presented annually by Doctors of BC to recognize and celebrate those who work tirelessly and passionately on meaningful initiatives. They are individuals, non-profit organizations, and corporations in our communities that work to make our province a healthier, safer place to live. They devote time and energy to ensuring vulnerable populations have access to the health care they need, the isolated are engaged in community events, and the young actively participate in health promotion initiatives, among many others." Furthermore, "successful nominees must have demonstrated a concern for health and safety through specific actions or initiatives. These actions must show ingenuity and creativity, and have resulted in change with the potential for positive, long-term improvement." In its summary of why the BC-CfE was chosen for the award, the Doctors of BC wrote, "A world leader in HIV/AIDS research and prevention, The BC-CfE has a track record of almost three decades spent dedicated to the health and safety of British Columbians. The organization's globally recognized TasP to End the AIDS Epidemic in BC and Beyond strategy advocates for widespread HIV testing and facilitates access to free medical treatment for thousands of eligible individuals in BC. TasP has exceeded its target goals and seen a dramatic decrease in HIV diagnoses and AIDS morbidity and mortality." BC-CfE leadership, some of whom have worked in the field of HIV/AIDS since its very earliest days, stress how the Centre has played a pivotal role in shaping not only BC's HIV/AIDS control strategy, but the world's, with its 90-90-90 Target standing out as a shining example. After publicizing and formally introducing TasP in the Lancet in 2006, the BC-CfE's 90-90-90 Target was eventually adopted by the United Nations organization responsible for HIV/AIDS, UNAIDS. When originally set, 90-90-90 would have seen 90% of all people living with HIV knowing their HIV status, 90% of all those diagnosed put on sustained antiretroviral therapy (ART), and 90% of all people on ART achieving viral suppression, a state where they cannot transmit HIV, by the year 2020. While this ambitious goal was unmet in much of the world, it was met here in BC. Dr. Julio Montaner, the BC-CfE's Executive Director and Physician-in-Chief announced the stunning accomplishment on last year's World AIDS Day in a joint press conference with BC's Health Minister Adrian Dix and Providence Health Care's President and CEO Fiona Dalton. Thanks to the work of the BC-CfE and the support of its governmental partners, BC not only met its 90-90-90 goals, but surpassed this target resulting in even further reductions in HIV/AIDS related morbidity and mortality as well as HIV transmission. In 2018, the Centre added publicly funded pre-exposure prophylaxis (PrEP) to its TasP strategy, specifically targeting men who have sex with men (MSM) at high risk for HIV infection. Having enrolled about 5,000 high risk MSM clients on PrEP, the number of HIV diagnoses in MSM residing in BC dropped by more than 30%. As BC endures two ongoing pandemics, COVID-19 and the opioid overdose crisis, the BC-CfE continues to advance HIV/AIDS control through TasP and PrEP as well as expanding services within Vancouver's Downtown Eastside with its Hope to Health Research and Innovation Centre. This Centre recently secured multi-year funding from Ottawa, BC's Ministry of Health, Vancouver Coastal Health, and generous philanthropic donors to pursue work focused on HIV, hepatitis C virus, mental health, and addictions. Doctors of BC bestow their awards on "Any individuals or group, non-profit, or corporation that has demonstrated a concern for health and safety through specific actions and/or initiatives that exemplify creativity and initiative to improve and protect the health and safety of British Columbians, and/or have results bringing about measurable change with the potential for positive, long-term improvement." As Dr. Gillespie said, "We consider The BC Centre for Excellence in HIV/AIDS a very deserving recipient of the award, please accept my congratulations on this exceptional achievement." | COAST, Laboratory | Forecast Newsletter | Download | ||||||||||||||||||||||
| April, 2021 | BC-CfE Drug Treatment Program Monthly Report (December 2020) | Drug Treatment Program | DTP Status Report | Download | |||||||||||||||||||||||
| April, 2021 | Laboratory Requisition Form, Untimed Drug Level Pilot Program, British Columbia | Laboratory | Laboratory Test Order Forms | Download | |||||||||||||||||||||||
| April, 2021 | Therapeutic Drug Monitoring Instructions (Research Study) | For study participation approval, contact jrclab@bccfe.ca | Laboratory | Laboratory Test Order Forms | Download | ||||||||||||||||||||||
| April, 2021 | Doravirine (Pifeltro(R)) and Doravirine-lamivudine-tenofovir disoproxil fumarate (Delstrigo(R)) | Formulary Addition | Dear Doctor Letter | Download | |||||||||||||||||||||||
| April, 2021 | Provincial Best Practice in HIV Case Management | Therapeutic Guidelines MenuProvincial Best Practice in the Re-engagement and Engagement in Treatment for Antiretroviral Interrupted and Naïve Populations (RETAIN)This document aims to provide a standardized practice in re-engagement and engagement in treatment for antiretroviral interrupted and naïve populations (RETAIN). The objective is to provide comprehensive support for people living with HIV who have become disengaged from care, or have delayed engagement in HIV care following diagnosis. | RETAIN, STOP HIV/AIDS | Therapeutic Guidelines | Download | ||||||||||||||||||||||
| April, 2021 | Blood and Body Fluid Exposure Management, BC CDC, Communicable Disease Control, April 2021 | PEP | Download | ||||||||||||||||||||||||
| March, 2021 | The BC-CfE mourns Carl P. Vanderspek |
The BC Centre for Excellence in HIV/AIDS (BC-CfE) is mourning the passing of its dear friend and generous supporter Carl P. Vanderspek. Having achieved tremendous success in business, he sought out champions and causes whose success would have great impact and his support of the BC-CfE was central to this philosophy. Many years ago, Carl met Dr. Julio Montaner, the BC-CfE's Executive Director and Physician-in-Chief. As Carl and Dr. Montaner's relationship grew, Carl became a key supporter for the projects and policies espoused by Dr. Montaner. Carl saw the promise of BC-CfE's Treatment as Prevention not only for HIV/AIDS, but also for hepatitis C, mental illnesses and substance use. Putting his entrepreneurial skills to work, Carl sought to help motivate the bureaucracy, minimize the red tape, and avoid the interminable wait times that typically accompany the establishment of new innovative programs. In this regard, he played a central role in strategically advising Dr. Montaner in his quest, and most critically, in the establishment of a new clinical research and innovation centre in Vancouver's Downtown Eastside, known as the Hope to Health (H2H) Research and Innovation Complex. Donald Mackenzie, a personal friend and director of Carl's foundation, the 625 Powell Street Foundation, described him as one of the most humble people you could ever meet, despite his incredible business successes. Donald shared how Carl would often say, "I do the easy work, I just write the cheques!" Not one to ever seek the spotlight, Carl declined formal recognition for his support, but behind the scenes he enjoyed celebrating the success of those he supported. Carl was very hands-on in overseeing the projects to which he was committed. At the H2H Complex, Carl ensured he had an office, so he could be on-site to monitor the extensive renovations required and the progress of the subsequent work. He enjoyed frequently engaging with Dr. Montaner and his colleagues, to discuss the optimal layout for H2H and potential ways to optimize the wrap-around services offered at H2H to improve the lives of those living in Vancouver's Downtown Eastside. Carl was a big picture visionary, and a strategic thinker. His input, guidance and commitment were invaluable to the success of our efforts. Carl was often frustrated with what he saw as the glacial pace of the system in helping communities most in need. He was committed to breaking down barriers and cutting through red tape to make sure projects got done and care delivered. He was a true man of action. In Dr. Montaner, Carl had found a friend, a partner, and a cause to champion, to fight for, and to support. Dr. Montaner provided Carl the ideal opportunity to leave a lasting impact in Vancouver, in BC, and the world. A theme emerges when speaking to those closest to Carl, and it's his desire to leave the world a better place, and for the improvements into which he poured his efforts to continue to flower and grow. "Carl was a true friend, a wise counsel, and magnanimous supporter. He played a critical role in enabling us to make our dreams a reality. He will be dearly missed. However, we look forward to continuing to work productively with his 625 Powell Street Foundation to ensure we see the fruits of his efforts flourish at the Hope to Health Research and Innovation Complex for a long time to come", said Dr. Montaner. Carl's desire was not that of a legacy, but instead to provide people and organizations with the tools they needed to do the great work he knew they could carry on. Carl's sentiment is nicely captured by a quote from the Dalai Lama, who said, "Just as ripples spread out when a single pebble is dropped into water, the actions of individuals can have far-reaching effects." Carl P. Vanderspek was a man of great successes, few words and simple tastes. A man who could have exclusively spent his final years enjoying his time with his beloved wife Margaret, their family, his dog, and a wide-range of pass-times. However, beyond that, he was fully committed to support his preferred champions and their causes, as he believed by enabling great success it will spur on others to achieve success. We are forever indebted to Carl for his overwhelming generosity and his unwavering dedication to making the world a better place. We are confident that Carl's ripples will be felt wide and far. | Clinical Education & Training, Hope to Health Primary Care Clinic, Laboratory | Forecast Newsletter | Download | ||||||||||||||||||||||
| March, 2021 | BC-CfE Drug Treatment Program Monthly Report (November 2020) | Drug Treatment Program | DTP Status Report | Download | |||||||||||||||||||||||
| March, 2021 | HIV Monitoring Semi-Annual Reports, Fourth Quarter 2020 |
| STOP HIV/AIDS | ||||||||||||||||||||||||
| February, 2021 | Federal funding helps BC-CfE expand safer drug supply in Downtown Eastside |
Federal, provincial, and local officials gathered over Zoom on February 1st to announce more than $15 million in federal funding for four safer drug supply projects for people at risk of overdose in BC. $3.6 million of this funding, awarded by Health Canada's Substance Use and Addictions Program (SUAP), will support an evidence-informed innovative Safer Drug Supply Program at the BC-CfE's Hope to Health Research & Innovation Complex in Vancouver's Downtown Eastside (DTES). BC-CfE staff at the complex will prescribe and provide pharmaceutical-grade medication as an alternative to the increasingly toxic illegal supply in circulation. BC, under a public health emergency declared in the Spring of 2016 due to the significant rise in opioid-related overdose deaths, has seen more than 6,500 people fatally overdose since the declaration. Now, with the concurrent public health emergency of the COVID-19 pandemic, the problem of fatal overdoses is getting worse. COVID-19 has made BC's street drug supply more toxic, while simultaneously increasing barriers to services. The latest data from the BCCDC indicates that as many as five British Columbians are dying every day as a result of overdoses Starting in October 2019, the Hope to Health Complex has offered primary care to DTES residents with the support of an interdisciplinary team of physicians, nurses, social workers, counsellors, and peer navigators. The model of care provides ‘wrap-around' healthcare to clients, ensuring they receive the full continuum of care under one roof. Over 800 clients have been registered since opening. Starting October 2020, the Hope to Health Complex added a Supervised Consumption Site, as an important new service and an additional entry point to the array of services provided. The new SUAP funding and the Risk Mitigation Interim Guidelines, allows the BC-CfE to expand access to methadone and hydromorphone as well as other pharmacological alternatives to street drugs among individuals chronically using illegal street drugs. Fiona Dalton, President and CEO of Providence Health Care said, "PHC welcomes this exciting news regarding the much-needed expansion of safer drug supply in the DTES led by the BC Centre for Excellence at the Hope to Health Complex. Helping people transition from the increasingly toxic supply of street drugs to pharmacological alternatives will save lives. This support from Health Canada's Substance Use and Addictions Program is much-needed as BC escalates efforts to control the opioid overdose crisis." Dr. Julio Montaner, the BC-CfE's Executive Director and Physician-in-Chief, said, "We are grateful for the support from Heath Canada's Substance Use and Addictions Program, a timely investment as we continue to battle British Columbia's opioid overdose crisis. In this context, the expansion of safer drug supply in the Downtown Eastside of Vancouver represents a critically important next step. This program expands the holistic nature of the supports we offer at the Hope to Health Complex, in collaboration with the BC-Government, Providence Health Care and Vancouver Coastal Health. Established with generous funding from two anonymous philanthropic donors, the Hope to Health Complex offers innovative primary health care, a dedicated oral opioid substitution program, and an ophthalmology clinic, as well as the newly established Supervised Consumption Site and the Safer Drug Supply program. Our ultimate goal is to expand and sustain the gains we have made in the control of HIV/AIDS in BC, and to continue to expand these efforts to the area of viral hepatitis, within an environment where mental health and substance use are highly prevalent and in urgent need of further innovative programs." The Zoom announcement of the SUAP funding saw Dr. Hedy Fry, Member of Parliament for Vancouver Centre, speak on behalf of Canada's Minister of Health, Patty Hajdu. Dr. Fry said, "The pandemic has magnified the effects of an already devastating overdose crisis across Canada. In B.C., we've been expanding services as well as advocating for additional federal resources and I'm pleased that Health Canada is working with us to help separate more people from the toxic drug supply. I'm grateful to the frontline organizations whose critical work is so vital to B.C.'s overdose response and the people they serve." Dr. Fry was joined by Sheila Malcolmson, BC's Minister of Mental Health and Addictions, and Dr. Patricia Daly, the Chief Medical Health Officer of Vancouver Coastal Health. All three agreed on the tenet that substance use disorder is a health condition that can be managed and treated if people are provided with services and supports that best meet their needs. The BC-CfE is doing its part to reduce overdose deaths by providing those living with opioid use disorder with a safer, medical alternative from a licensed prescriber and also by connecting people with critical health and social services. | COAST, Hope to Health Primary Care Clinic, Hope to Health Supervised Consumption Site (SCS) | Forecast Newsletter | Download | ||||||||||||||||||||||
| February, 2021 | BC-CfE Drug Treatment Program Monthly Report (October 2020) | Drug Treatment Program | DTP Status Report | Download | |||||||||||||||||||||||
| February, 2021 | BC-CfE Drug Treatment Program Monthly Report (September 2020) | Drug Treatment Program | DTP Status Report | Download | |||||||||||||||||||||||
| January, 2021 | BC-CfE Committee for Drug Evaluation and Therapy supports use of COVID-19 vaccines for people living with HIV |
The BC Centre for Excellence in HIV/AIDS (BC-CfE) Committee for Drug Evaluation and Therapy (CDET) recently completed its evaluation of all of the available data regarding the use of Pfizer and Moderna COVID-19 mRNA vaccines for persons living with HIV (PLWH). Based on the committee's expert opinion, the BC-CfE supports the use of Pfizer and Moderna COVID-19 mRNA vaccines to protect PLWH aged 18 years or older against COVID-19 related disease, if they meet current public health criteria for priority groups and if they have no contraindications to the product. Health Canada said the two COVID-19 vaccines it has so far approved are safe, effective and will save lives. In explaining the efficacy of the vaccines, Health Canada said, "Vaccines do more than protect the people getting vaccinated, they also protect everyone around them. The more people in a community who are vaccinated and protected from COVID-19, the harder it is for the virus to spread." Both Pfizer and Moderna vaccines are the mRNA type. This kind of vaccine, according to Health Canada, "teach our cells how to make a protein that will trigger an immune response without using the live virus that causes COVID-19. Once triggered, our body then makes antibodies. These antibodies help us fight the infection if the real virus does enter our body in the future." Although data for use of the mRNA vaccines in PLWH is limited, CDET expects similar vaccine responses to those without HIV. These mRNA vaccines are not known to be associated with more serious adverse events amongst immunocompromised individuals, however, it should be noted immune response may potentially be sub-optimal in those that are immunocompromised. PLWH on antiretroviral therapy with an undetectable HIV plasma viral load and CD4 count above 200 cells per cubic millimeter of blood (cells/mm3) are likely to have an intact immune response. CD4 cells are a type of white blood cell which play a key role in the immune system and when a person is living with HIV the virus attacks the CD4 cells in their blood. A healthy immune system normally has a CD4 count ranging from 500 to 1,600 cells/mm3. The efficacy and safety of Pfizer and Moderna COVID-19 mRNA vaccines is less clear amongst individuals with a detectable HIV plasma viral load or CD4 count below 200 cells/mm3. This is because PLWH who met these criteria were not included in these vaccine studies. CDET says these individuals may be offered the vaccine after risk/benefit counselling under the guidance of experienced health practitioners. B.C.'s vaccination strategy has been developed based on recommendations from the National Advisory Committee on Immunization (NACI). The strategy is focused on protecting those most vulnerable to severe illness first. The first groups to get vaccinated between December and February include: residents, staff, and essential visitors to long-term care and assisted-living residences; those in hospital or community awaiting a long-term care placement; health care workers providing care for COVID-19 patients; and remote and isolated Indigenous communities. Starting next month until March, the immunization program will expand to include many groups the BC-CfE serves. These include: seniors, age 80 and above; Indigenous (First Nations, Métis and Inuit) seniors, age 65 and above; people experiencing homelessness and/or using shelters; provincial correctional facilities; adults in group homes or mental health residential care; long term home support recipients and staff; hospital staff, community GPs and medical specialists; and other Indigenous communities not vaccinated in first priority group. BC's Provincial Health Officer Dr. Bonnie Henry says achieving herd immunity will become more of a government priority during the spring. This will be when more doses of the Pfizer and Moderna vaccines are available and two more COVID-19 vaccines are approved by Health Canada. As the government of BC says, "Herd immunity could be reached once 60 to 70% of the population is vaccinated. When people in British Columbia decide to get the COVID-19 vaccine, they are not only protecting themselves from the virus, they are also protecting everyone around them. If a majority of British Columbians get the COVID-19 vaccine, this would reduce transmission rapidly." | Clinical Research | Forecast Newsletter | Download | ||||||||||||||||||||||
| December, 2020 | BC-CfE Drug Treatment Program Monthly Report (August 2020) | Drug Treatment Program | DTP Status Report | Download | |||||||||||||||||||||||
| December, 2020 | BC-CfE Marks Record Achievements for World AIDS Day 2020 |
Started December 1, 1988, World AIDS Day annually raises awareness of the AIDS pandemic and is a day to mourn those who have died of the disease. The World Health Organization chose to focus on "Global solidarity, resilient HIV services" as its theme for this year. As of 2019 there were 38 million people living with HIV infection, 690,000 deaths from HIV-related causes, and 1.7 million people were newly infected. These numbers demonstrate that the global HIV epidemic is far from over, and there are fears that the spread of the disease may be accelerating during the COVID-19 pandemic. Tragically, the world will be missing the BC CfE-inspired, UNAIDS 90-90-90 target for 2020. That target was set to ensure that 90% of people living with HIV are aware of their status, and of that group of people diagnosed with HIV, 90% are receiving treatment, and then of all people receiving treatment 90% have achieved viral suppression. COVID-19's massive disruptions have made HIV services unaffordable or unobtainable for many, and the pandemic's interference with supply chains and service delivery meant that, as of July 2020, one third of people on HIV treatment around the world had experienced interruptions in drug supplies. A WHO and UNAIDS modeling study showed that a "six-month disruption in access to HIV medicines could lead to a doubling in AIDS-related deaths in sub-Saharan Africa in 2020 alone." However, in the midst of this bleakness, within a surging global pandemic and the opioid overdose epidemic, BC has been able to meet and surpass the UNAIDS target. In BC, as of this writing, at least 90% of people living with HIV are diagnosed, at least 90% of those diagnosed are receiving treatment with antiretroviral therapy, and at least 90% of those on treatment have a sustained undetectable HIV viral load. Furthermore, our province has seen a greater than 90% decrease in people living with and dying from AIDS. New HIV diagnoses in BC reached their lowest level yet in 2020, down by approximately 80% from the peak in 1987, when over 900 cases were diagnosed annually in BC. To announce and celebrate these achievements while observing COVID-19 restrictions, the BC Centre for Excellence in HIV/AIDS (BC-CfE) and the BC Ministry of Health held a virtual press conference on World AIDS Day hosted by Ms. Fiona Dalton with statements by Minister of Health Hon. Adrian Dix and Dr. Julio Montaner. Dr. Julio Montaner, the BC-CfE's Executive Director & Physician-in-Chief, said, "I am pleased to report BC has now surpassed the UNAIDS 90-90-90 target. Furthermore, this year BC has seen new HIV diagnoses decrease to the lowest level since the peak of the epidemic in the pre-HAART era. This is on top of this year's announcement of a record low number of AIDS diagnoses in BC. Our success remains strictly dependent on our ability to continue to support the existing programs and people living with HIV/AIDS. Failure to do so would be devastating and severely undermine the success of our strategy." Fiona Dalton, President and CEO of Providence Health Care said, "The 90-90-90 target for the management of HIV/AIDS is an incredibly powerful approach and we're proud it's been adopted by the UN for the worldwide control of HIV/AIDS. We're even prouder that the target has been surpassed in British Columbia, and as a result we are seeing a dramatic decrease in AIDS-related morbidity and mortality, as well as HIV transmission." The virtual press conference also showcased how the BC-CfE is applying Treatment as Prevention to therapeutic areas beyond HIV/AIDS, including viral hepatitis and addiction, promoting targeted disease elimination as a means to contribute to health-care sustainability. As part of this effort, Minister Dix and Dr. Montaner formally announced the opening of the Hope to Health Research and Innovation Centre in Vancouver's Downtown Eastside. The clinic supports people living with HIV, opioid addictions, mental health and other health issues, including hepatitis C. People can walk into the clinic without an appointment to see a nurse, social worker or a doctor, as needed. It provides support to people accessing medication for HIV and hepatitis C, as well as methadone and suboxone for opioid addictions. Take-home naloxone kits for treating overdoses from opioids such as fentanyl are also available. Additional services include referral for treatment, counselling and other health services. The Hope to Health Research and Innovation Centre is just one of the BC-CfE led and supported initiatives to further prevent the transmission of HIV in BC. Other examples include expanded public funding for pre-exposure prophylaxis (PrEP) and post-exposure prophylaxis (PEP). Provincial Health Officer Dr. Bonnie Henry said, "British Columbia has been at the forefront of response to the HIV/AIDS epidemic from the very beginning with the key collaborations between the health authorities and Dr. Julio Montaner and his team at the BC-CfE. This has led us to markedly reduce the impacts of what was once a death sentence not only here in BC, but also around the world." | BOOST, Laboratory | Treatment as Prevention® | Forecast Newsletter | Download | |||||||||||||||||||||
| December, 2020 | BC Centre for Excellence in HIV/AIDS CDET Committee Statement on the use of COVID-19 mRNA vaccines (Pfizer and Moderna) in Persons living with HIV | Download | |||||||||||||||||||||||||
| November, 2020 | New BC-CfE research seeks to improve COVID-19 nasal swab collection procedures |
New research that will help improve sample quality and patient experience in COVID-19 testing was recently published by BC-CfE research assistants Natalie Kinloch and Aniqa Shahid. Kinloch and Shahid are also PhD students in the Faculty of Health Sciences at Simon Fraser University under the supervision of SFU Professor and BC-CfE laboratory director Dr. Zabrina Brumme. Their findings were published in the scientific journal Open Forum Infectious Diseases. Nasopharyngeal swabs are critical to COVID-19 diagnostics, but collection techniques vary. The swabbing procedure is also notoriously uncomfortable. With the goal of improving sample collection quality and patient experience, Kinloch and Shahid teamed up with Dr. Victor Leung, Medical Director of Infection Prevention and Control at Providence Health Care, to evaluate two commonly used swab collection techniques. Specimen collection involves inserting a long flexible swab through the nostril all the way to the back of the throat to an area called the nasopharynx. This is a depth of about seven centimetres. The procedure must be performed by a trained healthcare professional familiar with the technique and nasal anatomy. There is, however, no consensus on what to do with the swab once it reaches the nasopharynx. In particular, many guidance documents recommend that the swab be rotated in place after contacting the nasopharynx, while others indicate that this is not necessary. The research team recruited adult volunteers to undergo a nasopharyngeal swab with or without rotation, and asked the volunteers to rate their discomfort during the swab procedure. Kinloch and Shahid also used a laboratory technique called droplet digital polymerase chain reaction (ddPCR) to assess nucleic acid recovery as a marker of swab collection quality. Their results revealed that swab rotation did not enhance sample quality. Furthermore, responses from the participants suggested that rotation made the procedure less tolerable. The team's first major conclusion was therefore that swabs do not need to be rotated during sample collection. Kinloch and Shahid's results additionally revealed that discomfort during the swab test varied widely: when participants were asked to rate their discomfort on a scale from zero to 10, their responses ranged from 1 to 10! On average, Asian participants reported higher levels of discomfort than those who self-identified as White, a finding that may be explained by differences in nasal anatomy among ethnic groups. The team's second major conclusion was that care providers need to be sensitive to such differences in people's experiences. The team is working with Dr. Leung to translate their findings into an improved COVID-19 diagnostic experience for people getting tested. Of the research, Kinloch said, "As a basic scientist, I often feel quite removed from the people my work will hopefully one day help. It has been very rewarding to contribute directly to the on-going COVID-19 pandemic response and be a part of research that has implications for clinical practice." As for her contribution to the published study, Shahid said, "This research was indeed a result of a dynamic and collaborative team effort at SFU, BC-CfE and PHC. I am excited to be a part of the scientific community that is actively working to accelerate our current understanding of the COVID-19 pandemic. This research, funded by Genome BC, was undertaken in partnership with Simon Fraser University and Providence Health Care. Ms. Kinloch is supported by a Vanier Canada Graduate Scholarship and Ms. Shahid by a CIHR Fredrick Banting and Charles Best Doctoral Award. | BOOST, Momentum | Forecast Newsletter | Download | ||||||||||||||||||||||
| November, 2020 | PrEP Quarterly Report for British Columbia - Second Quarter 2020 | PrEP | PrEP Quarterly Report | Download | |||||||||||||||||||||||
| November, 2020 | BC-CfE Drug Treatment Program Monthly Report (July 2020) | Drug Treatment Program | DTP Status Report | Download | |||||||||||||||||||||||
| November, 2020 | BC-CfE Drug Treatment Program Monthly Report (June 2020) | Drug Treatment Program | DTP Status Report | Download | |||||||||||||||||||||||
| September, 2020 | Dr. Julio Montaner Honoured as Groundbreaking Physician by Canada Post |
This September, the BC-CfE's Executive Director & Physician-in-Chief Dr. Julio Montaner was honoured by Canada Post as part of their Medical Groundbreakers stamp series. The new stamps honour groundbreaking contributions to medicine and include six Canadian physicians and researchers who revolutionized their fields of health care. Alongside Dr. Montaner, those chosen by Canada Post include Drs. Bruce Chown, Balfour Mount, M. Vera Peters, James Till and Ernest McCulloch. Dr. Montaner's work, for which he's dedicated four decades of his life, has helped transform HIV/AIDS into a manageable condition with a near-normal life expectancy and has also drastically reduced HIV transmission. He led the development of highly active antiretroviral therapy (HAART), now considered the global standard of care and also pioneered Treatment as Prevention (TasP), a strategy that has markedly reduced HIV transmission and has the potential to end the HIV/AIDS epidemic worldwide. Fiona Dalton, President and CEO, Providence Health Care, said, "I think there are real lessons we can learn now from how we managed a different virus, HIV, in the early '80s – a virus that was really scary that we didn't know anything about, which we had no treatment for, and we can see that again with COVID now." Dalton added, "We are really benefiting from that work in terms of HIV/AIDS and how we can apply that to our new pandemic." Eric Harris, the board chair at Providence Health Care, praised Dr. Montaner, and said, "He is brilliantly fearless, to the point of being breathtaking on occasion, but it's always backed up by organization, discipline, and clinical work." Those organizational skills were on full display as Dr. Montaner worked as a guiding force behind the 1996 International AIDS Society Conference, where he introduced HAART as a new global standard of care for HIV. The 1996 conference is widely seen as a turning point in HIV/AIDS history thanks to this revolutionary treatment. Within a year of implementing HAART in BC, AIDS deaths decreased by over 80%. As BC saw success in its HIV treatment approach, Dr. Montaner recognized gaps in care among those with socio-economic, cultural, or disease-related challenges, and his research informed harm reduction strategies in Vancouver including at InSite in the Downtown Eastside, North America's first supervised injection site. In 2006 Dr. Montaner demonstrated through models and a wealth of research findings from BC's experience that universal coverage with HAART could lead to the control and possible elimination of HIV within a generation. This, along with a landmark paper published in The Lancet in 2010, formed the basis for the BC-CfE's TasP strategy, which has since been formally adopted in many countries around the world and by the World Health Organization and Joint United Nations Programme on HIV/AIDS (UNAIDS). TasP then became the cornerstone of UNAIDS' 90-90-90 strategy in 2014, and recently helped inspire another game-changing initiative, U=U. The U=U campaign informs the public, healthcare professionals and policy-makers about the tenets of TasP, that those living with HIV who are successfully on HAART treatment and have an undetectable viral load are untransmittable. The continued success of TasP in reducing new diagnoses led St. Paul's Hospital to repurpose their AIDS Ward in 2014 and Dr. Montaner to declare the end of the AIDS epidemic in BC in 2019. The province, once the hardest hit by HIV/AIDS in Canada, now sees the disease as a chronic but manageable condition. Dr. Montaner continues to see patients, lead BC-CfE HIV treatment & research efforts, advocate for access to care, harm reduction & safe supply, and established the Hope to Health Centre in the DTES to ensure no one goes without the care they deserve. Having previously been invested in the Order of Canada and inducted into the Canadian Medical Hall of Fame, Dr. Montaner said, "This particular honour has unique significance because I view it as the recognition from the people of my adopted country, Canada." The image on Dr. Montaner's stamp was designed by Vancouver's Mike Savage and Dale Kilian at Signals including photography by BC-CfE Website and Digital Strategy Coordinator Fernando Prado. The PermanentTM domestic rate stamps are available in a booklet of 10 and can be purchased at canadapost.ca/shop. | Forecast Newsletter | Download | |||||||||||||||||||||||
| September, 2020 | HIV Monitoring Semi-Annual Reports, Second Quarter 2020 |
| STOP HIV/AIDS | ||||||||||||||||||||||||
| August, 2020 | BC-CfE work continues to evolve to help fight against and adjust to COVID-19 |
As of the last week of August the number of people with active COVID-19 infections in BC is at a record high, and we've now passed more than 200 deaths since the pandemic began. BC's total caseload is higher now than it was in March, when the province declared a state of emergency. TransLink and BC Ferries implemented mandatory mask policies also, requiring all passengers to wear masks while on board. Next month, all of BC's K-12 schools are set to reopen with a gradual, but full, return to in-class instruction for all students. Despite the discouraging news of rising case counts, and the sometimes uncomfortable and stressful adaptations we've all had to make during this pandemic, the staff at the BC Centre for Excellence in HIV/AIDS (BC-CfE) continue their vital work in treatment, research, outreach, and promotion of Treatment as Prevention. Per-SVR is a viral hepatitis study led by Dr. Kate Salters, a research scientist with the BC-CfE's Epidemiology and Population Health program. Researchers in this multi-year study are working to learn more about the experiences of people, particularly those from highly marginalized populations, who have been treated with the new direct acting antiretroviral hepatitis C medications. Recruiting and research work on this study were paused due to the pandemic, but now, after approval from provincial authorities, and safely operating from our Hope to Health Centre on Powell Street, Per-SVR has resumed. Thrive is a community-based research study focused on improving health outcomes among older adults living with HIV. Thrive researchers adapted to the pandemic and the project has received ethics approval to conduct phone interviews to accommodate physical distancing guidelines. The Momentum/Engage Studies look at the sexual health of gay, bisexual and other men who have sex with men in Greater Vancouver and has been active since 2012. The BC-CfE's Dr. David Moore leads this work and, after modifying workspaces and practices to ensure compliance with the latest safety directives, the studies are set to restart soon. COVID-19 has also changed aspects of the work done by the BC-CfE's Drug Treatment Program. As noted in media reports, there has been a drop of 30 per cent in pre-exposure prophylaxis (PrEP) prescriptions in BC between April and May and a 70 per cent drop in new initiations into the program. Lacking research to provide direct proof, it's believed the populations which would have been taking PrEP have been listening to health officials' orders to stay home and limit physical interactions. Dr. Junine Toy, senior manager for the Drug Treatment Program at the centre, didn't speculate as to the reason for the decline in PrEP prescriptions but did say the change in the volume aligned with the response to COVID-19. The accredited BC-CfE laboratories are another area where staff have had to make changes to accommodate COVID-19. In an update to doctors, prescribers, and people living with HIV, Laboratory Director Dr. Zabrina Brumme said increasing global demand for SARS-CoV-2 diagnostic testing has, for the second time during this pandemic, affected the availability of critical reagents required for HIV plasma viral load testing. Due to this, Dr. Brumme has requested a decrease in the frequency of HIV Plasma Viral Load Testing in stable patients on a stable antiretroviral therapy regimen. The BC-CfE's HIV and HCV Precision Medicine Testing Services has not been affected and the centre's medication dispensing services for its HIV Treatment and Prevention programs is continuing as usual. Dr. Jeff Joy, a BC-CfE senior research scientist specializing in evolutionary genetics, molecular epidemiology and bioinformatics, has been studying how COVID-19 spread around the globe, in particular how it arrived in North America and Europe. Furthermore, Dr. Joy and his research group have been using genomic analyses to quantify the effects of public health interventions and to study how the virus is evolving through time. Dr. Joy's as-yet-unpublished study suggests contact tracing efforts after the first cases of COVID-19 appeared in both the US and Germany were successful. Later introductions of the virus led to the outbreaks that are responsible for the epidemics in the US and Europe. In the US case these later introductions took place after travel bans were put in place. This kind of epidemiological research, so critical during a pandemic, will help in guiding policies to keep populations safe and fatalities down. | Epidemiology and Population Health | HIV Clinical Care | Forecast Newsletter | Download | |||||||||||||||||||||
| August, 2020 | BC-CfE Drug Treatment Program Monthly Report (May 2020) | Drug Treatment Program | DTP Status Report | Download | |||||||||||||||||||||||
| August, 2020 | BC-CfE Drug Treatment Program Monthly Report (April 2020) | Drug Treatment Program | DTP Status Report | Download | |||||||||||||||||||||||
| July, 2020 | BC-CfE contributes to vital dialogue at a virtual 23rd International AIDS Conference |
The fitting theme of AIDS 2020, the first fully-virtual International AIDS Conference, was Resilience. The theme reminded the global HIV community of its ability to come together despite a global pandemic to share our commitment to HIV prevention, treatment and cure research. More than 180 countries participated in this year's conference, held during the second week of July, and it featured more than 600 sessions and activities. Among the major findings revealed during the conference was a pilot proof-of-concept study of what could be the first case of an adult with HIV to achieve long-term remission without a bone marrow transplant. On the topic of Treatment as Prevention, a study presented at the conference found cabotegravir for long-acting injectable PrEP is not only just as effective, but superior, to daily oral Truvada for HIV PrEP. Meanwhile, UNAIDS Executive Director, Winnie Byanyima, and WHO Director-General, Dr Tedros Adhanom Ghebreyesus, presented virtually with both examining the link between the HIV and COVID-19 pandemics. Thanks to research from the US and the UK, we know HIV does not increase the risk of getting COVID-19 nor does living with HIV increase chances of a COVID-19 death. In fact, a London study found COVID-19 patients living with HIV improved faster than HIV negative patients. However, other research presented at AIDS2020 found COVID-19 lockdown measures affected PrEP access, led to a sudden shift to rapid self-testing, and in some areas, interrupted or restricted access to antiretroviral treatment. Furthermore, we now know, thanks to a Spring survey of more than 13,000 people in 138 countries, how COVID-19 is negatively impacting the global LGBTQ2+ community. Nearly half of those surveyed faced economic difficulty, with many unable to meet basic needs, skipping meals, or fearful of losing employment. 13% had already lost their jobs. Respondents also reported reduced access to safe injection equipment and opioid substitution therapy, something that threatens to undo global progress toward HIV prevention and treatment goals. The BC-CfE was represented by five researchers at AIDS 2020. Our epidemiologist Martin St-Jean and his team's presentation looked at the impact of drug overdoses on life expectancy among people living with HIV in BC and identified risk factors associated with increased overdose mortality. St-Jean's team found survival gains from effective antiretroviral therapy being threatened by drug overdose deaths among people living with HIV. The BC-CfE analysis included 10,362 HIV-positive people aged 20 or older in our province's HIV/AIDS Drug Treatment Program clinical registry. About a quarter of these people injected drugs. With their findings, St-Jean's team concluded that overdose prevention and substance use treatment are necessary components of quality HIV care programs. This vital study comes at a time when BC's opioid crisis is worse than it has ever been. May saw a record 171 people die from drug overdoses. That record was tragically broken in June, which saw 175 people die of illicit drug toxicity. In the first six months of this year, 728 British Columbians died from drug overdoses. As of this writing, COVID-19 has killed 194 in BC. Other BC-CfE attendees to AIDS2020 were able to afford the virtual conference thanks to the Bonnie Devlin Memorial Bursary Endowment Fund for Education. This fund was set up to honour Devlin (1957-2008), who worked at St. Paul's Hospital as the Program/Research Coordinator for Vancouver Lymphadenopathy AIDS Study (VLAS) between 1986 and 1992, and later for BC-CfE between 1992 and 2007. Bonnie was considered a mother-figure at BC-CfE who everyone loved and cherished. Julia Yinxin Zhu, a data analyst with the BC-CfE's Division of Epidemiology and Population Health, was able to virtually attend and take full advantage of the global platform to connect with scientists, researchers, and people living with HIV from across the globe. Raquel Maria Espinoza, a data entry clerk with the BC-CfE's Drug Treatment Program was also a beneficiary of the Bonnie Devlin Fund. Espinoza says, "As a health professional new to the research field, I knew I would greatly benefit from being able to engage with HIV research experts to not only learn about best research practices but also in an effort to contribute to discussions that will help shape future health policies and improve patient health." Attendees to AIDS 2020 saw the global virtual conference end with an urgent plea. Peter Sands, Executive Director of The Global Fund to Fight AIDS, Tuberculosis and Malaria, talked about the pandemic's drastic impact on both treatment and prevention of HIV, with lockdowns isolating people from their communities, disrupting global supply chains, and changes to local distribution of antiretroviral drugs and other vital medicines. Sands urged everyone involved in AIDS2020 to work together to fight against the COVID-19 pandemic and the potential backslide it could bring to the progress made against HIV/AIDS, and continue to work to further reduce new infections and to reduce deaths. | CHIWOS, Viral Hepatitis Research Program (VHRP) | Treatment as Prevention® | Forecast Newsletter | Download | |||||||||||||||||||||
| July, 2020 | 5-day PEP starter kit information for healthcare providers | PEP | Download | ||||||||||||||||||||||||
| July, 2020 | 5-day PEP starter kit information for patients | PEP | Download | ||||||||||||||||||||||||
| July, 2020 | Risk assessment: Estimated probability of HIV following a single exposure in British Columbia | PEP | Download | ||||||||||||||||||||||||
| July, 2020 | WorkSafeBC Physician’s Report (form 8/11) | PEP | Download | ||||||||||||||||||||||||
| July, 2020 | Counselling guidelines: Cautions to prevent potential HIV transmission to others, for persons who have experienced a significant exposure | PEP | Download | ||||||||||||||||||||||||
| July, 2020 | 23-day PEP continuation information for patients | PEP | Download | ||||||||||||||||||||||||
| July, 2020 | Dispensing Prophylactic Medications Post-Sexual Assault, BC CDC Practice Support Decision Tool | PEP | Download | ||||||||||||||||||||||||
| July, 2020 | Estimated risk of HIV transmission by exposure type from known HIV positive source person with detectable viral load | PEP | Download | ||||||||||||||||||||||||
| July, 2020 | Management of Percutaneous or Permucosal Exposure to Blood and Body Fluid/Laboratory Requisition form, HLTH 2339 (BC Ministry of Health) | PEP | Download | ||||||||||||||||||||||||
| July, 2020 | Management of Percutaneous or Permucosal Exposure to Blood or Body Fluid Letter for Follow- up Physician form, HLTH 2340 (BC Ministry of Health) | PEP | Download | ||||||||||||||||||||||||
| July, 2020 | Repeat Fill Authorization Permitted on BC-CfE Antiretroviral Prescriptions for the Treatment of HIV Infection | Notice to Prescribers | Dear Doctor Letter | Download | |||||||||||||||||||||||
| July, 2020 | Updates to BC-CfE HIV Drug Treatment and Prevention Programs |
| Notice to Prescribers | Dear Doctor Letter | Download | ||||||||||||||||||||||
| July, 2020 | BC-CfE Drug Treatment Program Monthly Report (March 2020) | Drug Treatment Program | DTP Status Report | Download | |||||||||||||||||||||||
| June, 2020 | BC-CfE launches BOOST Quality Improvement Network building on previous BOOST Collaboratives |
With BC in the midst of two public health emergencies, one for COVID-19 and one for drug overdose deaths, the BC Centre for Excellence in HIV/AIDS (BC-CfE) has just launched a new Quality Improvement Network for its BOOST Collaborative (Best-Practices in Oral Opioid agoniSt Therapy). Led by Dr. Rolando Barrios, the BC-CfE's Senior Medical Director, the Vancouver and Provincial BOOST Collaboratives brought together more than 40 teams to deliver services through mental health and substance use programs, and stabilization and primary care clinics, both in health authority and private practice settings. The new Quality Improvement (QI) Network, launched on June 25th, will build on this work and continue with the common purpose of improving care for clients living with opioid use disorder (OUD) by systematically implementing, measuring and sharing best practices in Opioid Agonist Therapy (OAT). The arrival of the new BOOST QI Network comes at a crucial time for this province as last month was the deadliest in BC history for illicit drug overdoses. In May 170 people died, with first responders attending to close to 2,300 overdose calls. Since the declaration of the public health emergency in early 2016, there have been more than 5,000 confirmed opioid-related overdose deaths in BC alone. Hon. Judy Darcy, BC Minister of Mental Health and Addictions, summed up the lead-up to the tragic month by saying, "Before COVID-19, there was so much more to do, but we were heading in the right direction. The overdose death rate was coming down in BC, and the evidence told us that our collective efforts were making a difference. The rapid scale up and distribution of naloxone and increased access to overdose prevention services (OPS) and treatment showed, through the BC Centre for Disease Control, that we had averted more than 6,000 deaths since the crisis began. Indeed, since the global COVID-19 pandemic began, BOOST Collaborative partners have seen first-hand its early effects and impacts on the ongoing opioid crisis. With our borders closed, the usual illegal drug supply chains are disrupted leading to an increasingly toxic drug supply on the streets. COVID-19 has also increased unemployment, social isolation, and has exacerbated mental health and addiction issues. The BOOST QI Network, however, has partners and leaders who have the benefit of experience and accomplishments from working within the BC-CfE's Treatment as Prevention mandate. Dr. Barrios says, "The QI Network is rooted in the experiences and accomplishments of the Treatment as Prevention and the STOP HIV/AIDS Collaboratives." BOOST collaborators stress the importance of using established improvement tools and methods to implement system changes. Doing so is critical in ensuring the maintenance of the gains made over the last couple of years in improving overall care for clients living with OUD. Evidence shows that a significant proportion of individuals with OUD will reduce illicit opioid use and remain in treatment longer with appropriate doses of opioid agonist therapy such as methadone, buprenorphine/naloxone or slow release oral morphine. Furthermore, the BOOST QI Network aims to provide equitable access to integrated, evidence-based care to help clients with OUD. The Collaborative's goals are to see 95% of clients with an active OAT prescription, 95% of those clients with an active OAT prescription retained on therapy for greater than 3 months, and 100% of teams with a process to monitor and incorporate the patient voice in their quality improvement work. QI teams will be supported in their mission to achieve these goals by continued quality improvement coaching, educational webinars, quarterly feedback reports, access to expert faculty, and half-day Learning Sessions. Another invaluable resource for the BOOST QI Network and its clients is the BC-CfE's Hope to Health Research & Innovation Centre in the heart of Vancouver's Downtown Eastside. The Research & Innovation Centre provides integrated and accessible healthcare to clients in the inner city with complex healthcare needs. Many of these clients have multiple conditions that can include HIV, hepatitis C, and mental health issues. Staffed by an interdisciplinary team of physicians, nurses, counsellors, and peer navigators, the Research & Innovation Centre provide ‘wrap-around' healthcare to clients, ensuring they receive the full continuum of care under one roof. The BOOST QI Network project team say the early effects of COVID-19, and its impact on the ongoing opioid crisis, demonstrates the importance of using established improvement tools and methods to implement system changes. Doing so is critical in ensuring the maintenance of the gains made over the last couple of years in improving overall care for clients living with OUD. | BOOST, Clinical Education & Training, Laboratory | Harm Reduction | Forecast Newsletter | Download | |||||||||||||||||||||
| June, 2020 | PrEP Quarterly Report for British Columbia - Second Quarter 2019 | PrEP | PrEP Quarterly Report | Download | |||||||||||||||||||||||
| June, 2020 | Guideline for Antiretroviral Therapy (ART) Regimens for Initial Therapy and for Switching ART in Virologically Stable Suppressed Adults | Guidance document | Dear Doctor Letter | Download | |||||||||||||||||||||||
| May, 2020 | BC-CfE provides update on response to COVID-19, while teams lead new research into the virus |
With BC currently in its longest-ever state of emergency, the BC-CfE continues to perform its critical work of promoting testing, treating and learning from people living with HIV (PLHIV), while carrying out epidemiological and infectious disease research and the mandate of Treatment as Prevention. In a recent webinar, BC-CfE's senior leadership outlined how the Centre's work has changed and what has stayed the same during this global COVID-19 pandemic. Moderated by Dr. Silvia Guillemi, Director of BC-CfE's Clinical Education and Training program, the webinar had several goals, including a review of the current epidemiology, containment, and clinical management of COVID-19 in BC. Dr. Peter Phillips, Clinical Professor in the Division of Infectious Diseases at the University of British Columbia, provided an overview of the epidemiology for the five largest Canadian COVID-19 epidemics. Dr. Phillips' presentation discussed COVID-19 issues such as demographics, testing frequencies, and statistical information such as case fatality ratios. Other presenters included the BC-CfE's Laboratory Director Dr. Zabrina Brumme, Research Scientist Dr. Jeffrey Joy, Senior Medical Director Dr. Rolando Barrios, and Executive Director and Physician-in-Chief Dr. Julio Montaner. The webinar also provided updates on COVID 19 molecular virology and bioinformatics support BC-CfE laboratories are providing to the local and international community, and provided background on the virus and understanding of its evolution and molecular epidemiology in BC, Canada and beyond. While this may sound complicated and daunting for someone without an extensive background in epidemiology or infectious diseases, anyone interested can check out the webinar at bit.ly/BCCfE_COVIDupdate and see for themselves that the knowledge is presented in an easy-to-understand format. Meanwhile, the BC-CfE's HIV Precision Medicine testing services, which had been temporarily suspended during this pandemic, have now resumed. The same BC-CfE laboratories that provide this invaluable testing, are also working to research and learn as much as possible about COVID-19. Two teams led by BC-CfE scientists have qualified for the Rapid Response Funding for COVID-19 Research Projects overseen by Genome BC. The first team is led by Dr. Chanson Brumme, the BC-CfE's Assistant Laboratory Director. Working with Don Kirkby, the BC-CfE laboratory's lead software developer, C. Brumme's team's project is called "Rapid release of an easily accessible SARS-CoV-2 genome analysis pipeline". This project will adapt an open-source software package, co-created by Kirkby and former BC-CfE scientist Dr. Art Poon, to analyze genetic data from SARS-CoV-2, the virus that has caused the COVID-19 pandemic. The original software package, also funded by Genome BC, was successful in identifying drug resistance in other viral diseases including HIV and Hepatitis C. A beta version, already in use, has so far successfully assembled SARS-CoV-2 genomes from various publicly-available data sources. This vital work will increase local and global capacity to sequence circulating SARS-CoV-2 genomes, which will in turn advance understanding of the molecular epidemiology and virology of this infection. The BC-CfE hopes to see this new tool rapidly adopted by the global scientific community. The BC-CfE estimates that the software will be publicly available within one week, which will enable users to contribute COVID-19 genomic data to public repositories. This public sharing of data will further enable researchers to track the virus's origins, spread, and evolution in real time. Furthermore, the data will help develop much-needed medications and vaccines against COVID-19. The second BC-CfE team fighting COVID-19 is co-led by Dr. Z. Brumme and Dr. Christopher Lowe, Medical Microbiologist and Virologist, who leads the Virology Laboratory at St. Paul's Hospital. Z. Brumme and Lowe's team has two aims: the first is to use sophisticated molecular technology to better understand the performance characteristics of the current COVID-19 testing process, and the second is to develop a quantitative SARS-CoV-2 viral load assay. The development of a quantitative viral load assay will be critical in helping to determine which therapeutic interventions are most effective. Together, these efforts will advance our understanding of COVID-19 and lead the way towards controlling this pandemic. | Clinical Education & Training, Epidemiology and Population Health, Hope to Health Primary Care Clinic, Laboratory | Forecast Newsletter | Download | ||||||||||||||||||||||
| May, 2020 | BC-CfE Drug Treatment Program Monthly Report (February 2020) | Drug Treatment Program | DTP Status Report | Download | |||||||||||||||||||||||
| May, 2020 | BC-CfE Drug Treatment Program Monthly Report (January 2020) | Drug Treatment Program | DTP Status Report | Download | |||||||||||||||||||||||
| May, 2020 | Antiretroviral Treatment (ART) Pick-up in Community Pharmacy | Resources for Community Pharmacists | Download | ||||||||||||||||||||||||
| May, 2020 | Antiretroviral Medication Pick-up Flow Sheet | Resources for Community Pharmacists | Download | ||||||||||||||||||||||||
| May, 2020 | Antiretroviral Medication Return Form | Resources for Community Pharmacists | Download | ||||||||||||||||||||||||
| May, 2020 | Antiretroviral Medication Reorder Form | Resources for Community Pharmacists | Download | ||||||||||||||||||||||||
| May, 2020 | Sample Antiretroviral Medication Inventory Form | Resources for Community Pharmacists | Download | ||||||||||||||||||||||||
| May, 2020 | Quick Reference HIV Guidelines for Community Pharmacists | Resources for Community Pharmacists | Download | ||||||||||||||||||||||||
| April, 2020 | BC Ministry of Health Directive to Include Antiretrovirals on PharmaNet | Notice | Dear Doctor Letter | Download | |||||||||||||||||||||||
| April, 2020 | BC-CfE Response to COVID-19 |
During these uncertain and unprecedented times, the senior leadership of the BC Centre for Excellence in HIV/AIDS (BC-CfE) presented a webinar to inform and reassure its clients, staff, and stakeholders, their critical work, with only a few minor modifications, will continue during the global COVID-19 pandemic. Presented on March 25th, the webinar titled, "COVID-19, the BC-CfE Response", was organized and led by BC-CfE Director of Clinical Education and Training Dr. Silvia Guillemi. Touching on key areas of service delivery, the panel included: BC-CfE Executive Director and Physician-in-Chief Dr. Julio Montaner, Clinical Professor with UBC's Division of Infectious Diseases Dr. Peter Phillips, BC-CfE Laboratory Director, Dr. Zabrina Brumme, and BC-CfE Drug Treatment Program (DTP) Senior Manager Dr. Junine Toy. Dr. Julio Montaner opened the webinar, giving a high-level overview of what clients, healthcare providers, and prescribers can expect to see change during this global health emergency. Despite limited data, he said international research on COVID-19 indicates there appears to be no increased risk of the disease for people living with HIV provided they are being effectively treated with, and adhering to, antiretroviral therapy and have a consistently undetectable viral load. He did however stress the need for everybody, regardless of whether or not they're living with HIV, to adhere to all of the recommendations from health officials such as hand washing, social distancing, and staying at home as much as possible. Dr. Peter Phillips followed by comparing and contrasting the current COVID-19 pandemic with other respiratory viral epidemics and pandemics. For those not closely following news of the COVID-19 pandemic, Dr. Phillips showed how the most recent similar pandemic that the world has been through, the so-called "Spanish flu" of 1918 compares to COVID-19. More accurately labelled an H1N1 virus, this pandemic infected about 500 million people, about a third of the world's population, and killed at least 50 million worldwide. Thankfully, the death toll from COVID-19 is currently nowhere near that high. But Dr. Phillips was clear and unequivocal in saying our current pandemic has the potential to be that deadly if we don't heed the warnings of health experts. In fact, data presented by Dr. Phillips showed that COVID-19 could be even deadlier than the Spanish flu, due to having a higher fatality and infectivity rate, and the degree of interconnectedness of the world today compared to 1918. It wasn't all a message of doom, Dr. Phillips said there are measures which can be taken by individuals, groups, and governments to stop the spread of COVID-19 including widespread adherence to the advice given by medical health officials to social distance. Up next, Dr. Zabrina Brumme stressed the BC-CfE Laboratory's precision medicine testing remains operational, but asked healthcare providers to restrict the number of tests requested and warned some results will be delayed up to a week due to processing delays of samples in the system. The lab will temporarily reduce the availability of non-essential precision medicine testing in order to ensure capacity for essential HIV testing urgently needed in clinical care. If non-essential testing is urgently required, the Lab will perform them but asks providers first contact the BC-CfE directly. Dr. Junine Toy closed out the webinar assuring prescribers and clients the DTP and BC-CfE management have been proactively working to ensure an adequate supply of medication in the province. She provided an update on how the DTP is working with prescribers and clients to streamline the process from prescription to medication delivery. The main goal of these changes is to ensure continuity of therapy while limiting time and exposure for those accessing medications and related healthcare appointments. This includes temporary adjustments to dispensing of longer supplies of medication and reduced non-essential routine viral load testing in virologically-suppressed clients on stable therapy. Dr. Toy highlighted the desire for prescribers and clients to simplify medication prescription, preparation and pick-up. Wherever possible and if able, the DTP asks prescribers to direct prescriptions directly to the pharmacy in advance, clients to specify medication pick-up dates, and if sending a delegate (e.g. friend or family member), to provide their full name. The full webinar can be reviewed at bit.ly/COVIDresponsewebinar, however as the situation and response to COVID-19 is constantly evolving, please refer to the BC-CfE website for the most up-to-date information: www.cfenet.ubc.ca. | Clinical Programs, Clinical Research, Drug Treatment Program, Laboratory, Operations, Quality and Safety | Forecast Newsletter | Download | ||||||||||||||||||||||
| March, 2020 | HIV Post-Exposure Prophylaxis (PEP) Guidelines | Therapeutic Guidelines MenuFor information on how to obtain medication for prevention of HIV infection following a high risk occupational or non-occupational exposure, please call the St Paul's Hospital Ambulatory Pharmacy 1-888-511-6222
| PEP | Therapeutic Guidelines | Download | ||||||||||||||||||||||
| March, 2020 | BC-CfE AND COVID-19: HIV Treatment and Prevention Programs Update | Notice to Prescribers | Dear Doctor Letter | Download | |||||||||||||||||||||||
| March, 2020 | BC-CfE Drug Treatment Program Monthly Report (December 2019) | Drug Treatment Program | DTP Status Report | Download | |||||||||||||||||||||||
| March, 2020 | COVID-19 and how it will affect Precision Medicine testing | BC-CfE Lab Notice to Prescribers | Dear Doctor Letter | Download | |||||||||||||||||||||||
| February, 2020 | The enigma of HIV's effects on aging |
We are in a new era of HIV research and care. We have never known more about the virology of HIV. We also have an array of highly effective antiretroviral therapies which suppress HIV to undetectable levels, while extending the life expectancy of individuals with HIV to close to that of the general population. These are all significant signs of progress; however, the legacy from the height of the HIV epidemic remains today through another complex and multifaceted healthcare challenge. The average age of a person living with HIV in Canada is now over 50 years old and this is projected to rise above 65 in the next 10 years. While this is a positive indication of the impact of highly active antiretroviral therapy (HAART) and Treatment as Prevention® in significantly reducing new cases of HIV, this aging population presents with age-related diseases sooner and more frequently than the general population. This includes cardiovascular and metabolic conditions, as well as cognitive impairment and frailty, among others. Little is understood about why this is the case. The BC Centre for Excellence in HIV/AIDS (BC-CfE) is playing an active role in research to better understand this population's distinct physiological and psychosocial challenges. Over the last 10 years, BC-CfE researchers have participated in a series of long-term investigations to look more closely at the lifestyle and health factors associated with aging with HIV. Positive Brain Health Now is one such study. Since 2013, the BC-CfE has participated in this long-term investigation funded by the Canadian Institutes of Health Research (CIHR) with the support of the Canadian HIV Trials Network (CTN). Led by investigators at McGill University, Positive Brain Health Now researchers are focused on better understanding HIV-related ‘brain health' factors and how these impact patient outcomes. This includes general cognitive processes such as concentration and memory, mental health and quality of life. By carefully tracking 856 adults living with HIV over time, researchers hope to understand the risk factors associated with declining brain health. While those living with HIV may experience higher rates of cognitive impairment, they are also more likely to show physical signs of aging sooner than the general population. In the fall of 2019, the BC-CfE joined the CIHR-CTN CHANGE HIV study which investigates frailty and other aging-related conditions in Canadians over the age of 65 living with HIV. The term frailty is commonplace in geriatric medicine and is used as a marker of physical wellbeing. Speaking about this study, Dr. Silvia Guillemi, Director of Clinical Education at BC-CfE said, "Many studies look at aging, however typically they follow younger populations as they age. With the CHANGE study, we are looking at an older population from the start and charting their progress over five years looking at various aspects of their lives, including physical activity levels, trauma, among others." The care and support received at home among older adults with HIV can also impact their overall health outcomes. THRIVE, a study based at the BC-CfE, is exploring experiences accessing home and community supports in BC for those aged 50 years and older. Through qualitative interviews, researchers aim to understand how this population navigates the home and community care system and using novel "service access mapping" interviews, this study will also document the day-to-day experiences of this population - from where they fill prescriptions to where they access food. Participants' narratives will help researchers understand how shifts in funding priorities have impacted the accessibility and nature of this care. Dr. Marianne Harris is a clinical research physician with the BC-CfE. Speaking about the importance of aging studies in HIV research, she said, "People living with HIV are now living into their 50s, 60s, 70s and beyond thanks to the success of modern antiretroviral therapy. Now they're facing a new set of issues that affect their quality of life including loss of memory, muscle weakness, breathing problems and so on. They're asking, ‘Is this an HIV outcome or is it natural aging, and what can I do about it?' "The best way to answer these questions is to study a large and diverse group of people living with HIV over time and look at how the effects of aging can be impacted by different interventions and lifestyle changes. It's important that people living with HIV are actively involved in this research to share their lived experiences and to help us better understand what's most important to them," Dr. Harris explained. According to the World Health Organization 37.9 million people were living with HIV/AIDS globally in 2018. As cure research continues to evolve, we need to ensure that people who are living with HIV, regardless of their age, are empowered and equipped with the knowledge of how to maintain good health and wellbeing. | Clinical Education & Training, Clinical Programs, Clinical Research, Laboratory, THRIVE | HIV Clinical Care | Forecast Newsletter | Download | |||||||||||||||||||||
| February, 2020 | HIV Monitoring Quarterly Reports, Fourth Quarter 2019 |
| STOP HIV/AIDS | ||||||||||||||||||||||||
| February, 2020 | BC-CfE Drug Treatment Program Monthly Report (November 2019) | Drug Treatment Program | DTP Status Report | Download | |||||||||||||||||||||||
| January, 2020 | How the Power of T-Cells May Lead to an HIV Cure |
Dr. Mark Brockman, a BC Centre for Excellence in HIV/AIDS (BC-CfE) Scientific Associate, recently presented at St. Paul's Hospital as part of the BC-CfE's Forefront Lecture series on the potential of using host T cells to eliminate the HIV viral reservoir. One of the principal challenges in achieving long-term ART-free HIV remission or a cure is the existence of a viral reservoir which resides within host cells as little as a day or two following infection. This resilient array of proviruses evolves and diversifies over time in the absence of antiretroviral therapy equipping them to evade host immune response. If an individual achieves viral suppression and is taken off antiretroviral therapy, the virus is thus capable of ‘rebounding' using this viral reservoir to propagate and recirculate in an individual's blood. Current HIV cure research is focused on ‘blunting' this viral rebound or finding a sterilization cure, where the reservoir would be completely eliminated. One approach Brockman discussed, referred to as ‘Kick and Kill', is being investigated by HIV researchers. These compounds trigger and shock proviruses, which make up the reservoir, to appear in plasma where they can be targeted and eliminated by host immune cells and antiretroviral therapy. However, latency reversal agents (LRAs) alone do not seem to reduce the size of this reservoir; another arm of therapeutics is required to complement their effects. Brockman explained a huge focus of his laboratory's research is the use of host immune response to eliminate viral reservoirs following the use of LRAs - specifically, by exploiting CD8 killer T cells. CD8 T cells play an important role in control of HIV in the acute phase of the infection, where they can suppress viral levels in the blood. However, after a month or so, HIV has adapted sufficiently to overcome host immune responses where the infection reaches a steady state and the virus cannot be eliminated. As a component of the adaptive immune system, CD8 T cells recognize pathogen-derived peptides presented by human leukocyte antigens (HLA) on the surface of infected cells. They then mount a tailored immune response that attempts to eliminate the infection. Research shows there are thousands of genetic variants (or alleles) of HLA among the population. The HLA alleles expressed by an individual determine which HIV peptides are presented to CD8 T cells, with some HLA alleles being better equipped to mount a strong CD8 T cell response to infection. Brockman explained that in addition to the scale of HLA variation among the population, there is also genetic variability in the HIV peptides presented to T cells. The virus rapidly mutates these sequences to further mask itself from T cells and their response. HIV peptides bound to HLA are recognized by specific T cell receptors expressed on the immune cells. Millions of T cell receptor variations are present within an individual, reflecting the enormous genetic diversity present within the immune system. Only a small number of T cell receptors respond to a particular peptide/HLA combination, and the exact contribution of T cell receptor variation to the immune response to HIV is still not well understood by researchers. Brockman and his research team are attempting to deconstruct this highly diverse process in an effort to exploit it for development of an effective HIV cure. Collaborating with researchers in South Africa, they are investigating the impact of HLA and T cell receptor variation on an individual's response to HIV infection. In collaboration with researchers at the CDC in China, they are using advanced crystallography techniques to better understand the structure and dynamics of HLA-peptide-receptor interactions. By getting a better understanding of the mechanisms used by T cell receptors to recognize HIV infection, we can improve our ability to develop vaccines and therapies that overcome the challenge of HIV diversity. In addition to his studies, Brockman discussed a number of strategies that are being investigated by others to enhance host immune responses to HIV. These include selectively expanding antiviral T cells outside the body and re-administering them to patients; and gene therapy, where T cell receptors are engineered in the laboratory and the altered receptors are then inserted into an individual's T cells. A less invasive approach using soluble bi-specific molecules, such as HIV-specific antibodies or T cell receptors, could also be used to re-direct CD8 T cells to sites of viral infection. In many respects, this approach could be the safest as it doesn't require manipulation of an individual's immune system. Investigating potential cures for HIV is a significant focus of the BC-CfE's laboratory program. While Treatment as Prevention strategies are being applied widely in BC to ensure early and efficient diagnosis of HIV, cure research is also essential to explore in tandem with clinical efforts if we are to fully eliminate HIV as a public health threat. | Clinical Education & Training, Laboratory | Forecast Newsletter | Download | ||||||||||||||||||||||
| January, 2020 | Updated BC-CfE Reference Documents Available for Use | Notice to Prescribers | Dear Doctor Letter | Download | |||||||||||||||||||||||
| December, 2019 | BC-CfE Drug Treatment Program Monthly Report (October 2019) | Drug Treatment Program | DTP Status Report | Download | |||||||||||||||||||||||
| December, 2019 | BC-CfE Drug Treatment Program Monthly Report (September 2019) | Drug Treatment Program | DTP Status Report | Download | |||||||||||||||||||||||
| December, 2019 | BC first province to declare the End of AIDS as an Epidemic |
On Sunday December 1, 2019, World AIDS Day, the Minister of Health Adrian Dix and the BC Centre for Excellence in HIV/AIDS (BC-CfE) announced the end of AIDS as an epidemic in British Columbia (BC). The announcement was made along with the opening of the BC-CfE's new laboratory on Powell Street. The new BC-CfE Research Laboratory is expanding its clinical and research services, including HIV cure research, further drug resistance testing and phylogenetics monitoring. Since 1992, the BC-CfE has closely monitored and evaluated HIV and AIDS rates in BC including recording new cases of HIV, testing rates, the number of people on treatment and new cases of AIDS. The BC-CfE revealed that AIDS cases have declined by over 90% since 1994, while new HIV cases have declined by over 75%. Both rates are at their lowest since the HIV crisis first arrived on the doorsteps of BC. The rate of new AIDS cases in BC now meet the UNAIDS working definition of ending AIDS as an epidemic as outlined by the organization's 90-90-90 Targets. In BC, AIDS has now transitioned from an epidemic to an endemic concern. This announcement adds to the BC-CfE's legacy of leading the way in innovative research and care for HIV and AIDS. In 1996, the BC-CfE pioneered highly active antiretroviral therapy (HAART) which significantly reduced a patient's viral load, decreasing morbidity and mortality. This led to the BC-CfE's Treatment as Prevention (TasP ) strategy - introducing earlier, sustained access to care and treatment to reduce patients' viral load to undetectable levels. This made-in-BC, strategy decreased HIV-related morbidity and mortality as well as HIV transmission in BC. TasP is the foundation of the global UNAIDS 90-90-90 Targets to end the AIDS epidemic worldwide by 2030. "Since the first AIDS patients presented to St. Paul's Hospital in downtown Vancouver, struggling against stigma and marginalization, community, researchers and clinicians worked tirelessly to advance evidence-based research to inform BC's HIV treatment policies," said Dr. Julio Montaner, BC-CfE Executive Director and Physician-in-Chief. "This included pioneering effective treatment, supporting widespread availability of antiretroviral therapy and making PrEP (pre-exposure prophylaxis) available to those deemed most at risk of contracting HIV. We are now reaping the rewards of this province's continued commitment to provide the best possible care for HIV as we set a standard for the rest of the world." In January 2018, the BC Minister of Health announced the availability of PrEP to all British Columbians deemed clinically at risk of contracting HIV, adding another prevention tool to BC's TasP approach. To date, over 5,000 people have initiated treatment as part of this program. Preliminary data indicates that PrEP is working in tandem with early treatment of HIV to further reduce new infection rates in the province. "British Columbia is known around the world as the catalyst for pioneering HIV treatment, research and innovative strategies," said Dr. Montaner. "We will advance our phylogenetics research and grow our Laboratory Program here at 647 Powell Street to better address HIV and continue our investigations into finding an HIV cure, with the support of the BC government." While HIV and AIDS infection rates have significantly declined across the province, neither will be eradicated without the development of a safe, effective and scalable cure or vaccine. BC-CfE researchers use advanced phylogenetics to not only investigate potential HIV cures, but also to monitor HIV ‘clusters'. This information provides insights into HIV transmission patterns, allowing healthcare resources to be targeted to regions most in need of additional follow-up and treatment. The BC-CfE's new laboratory space will also allow its Research program to further contribute to World Health Organization-sponsored HIV drug resistance surveys. These international efforts serve to better understand the spread of drug-resistant HIV in developing nations and inform programmatic changes to treatment strategies in these countries. | Laboratory | Treatment as Prevention® | Forecast Newsletter | Download | |||||||||||||||||||||
| December, 2019 | PrEP Patient Information Sheet | PrEP | PrEP Documents and Forms | Download | |||||||||||||||||||||||
| December, 2019 | BC-CfE Drug Treatment Program Monthly Report (August 2019) | Drug Treatment Program | DTP Status Report | Download | |||||||||||||||||||||||
| December, 2019 | BC-CfE Drug Treatment Program Monthly Report (July 2019) | Drug Treatment Program | DTP Status Report | Download | |||||||||||||||||||||||
| December, 2019 | HIV Monitoring Quarterly Reports, Third Quarter 2019 |
| STOP HIV/AIDS | ||||||||||||||||||||||||
| November, 2019 | BC-CfE Eligibility Criteria for emtricitabine/tenofovir alafenamide (FTC/TAF; Descovy®) | Guidance document | Dear Doctor Letter | Download | |||||||||||||||||||||||
| November, 2019 | Bictegravir-emtricitabine-tenofovir alafenamide (Biktarvy®) | Formulary Addition | Dear Doctor Letter | Download | |||||||||||||||||||||||
| October, 2019 | BC Centre for Excellence in HIV/AIDS invites the "Berlin Patient", the first person to be cured of HIV, to Vancouver |
"It's extraordinary story," begins Dr. Zabrina Brumme, Laboratory Director at the BC Centre for Excellence in HIV/AIDS (BC-CfE) and Professor of Health Sciences at SFU. Timothy Brown, known worldwide as the "Berlin patient" and the first person to be cured of HIV, was introduced by Dr. Brumme to a conference room in Vancouver. Attendees included community members, researchers, scientists, healthcare workers, post-doctoral fellows, and media. Dr. Brumme kickstarted Brown's talk with an overview of the science and the possibilities for an HIV cure. She emphasized while Brown's cure is inspiring, it is not a safe, scalable solution for people living with HIV around the world. However, Dr. Brumme pointed out, hearing the personal stories of people impacted by HIV, create opportunities for scientists and those with lived experience to come together in dialogue to move closer to an HIV cure. Timothy Brown was born and raised in Seattle and moved to Europe in 1991 when he was 25 years old. He settled in Barcelona and decided to study in Europe, where he found getting an education was affordable. Timothy quickly adapted to his new home and developed an active social life, meeting and working with people from all over the world. At this stage of his life, Brown says his idea of safe sex "was not safe at all". One of his partners, who was living with HIV, recommended Timothy get tested – he tested positive. Brown says the news stunned and upset him and he struggled to share his new status, especially with his family. Doctors put him on anti-retroviral medication, AZT (azidothymidine) as treatment, initially starting him on a low dose. "Basically, I forgot I was HIV positive," he says. He went for a checkup once a month and took his medication regularly but went on to resume his work and social life. Brown met someone who was also living with HIV and entered a long-term relationship. In 2006, Brown's health took a turn when he was in New York for a wedding and realized he was exceptionally tired. He didn't think much of it, but once he was back in Berlin, he noticed it took him longer than usual to ride to work. Shortly thereafter, as he rode his bike to a restaurant, he was only able to get halfway through his journey. After seeing a doctor, he found out he had anemia – and a very low blood cell count. He proceeded to get a transfusion but was eventually referred to an oncologist. After living with HIV for about 10 years, Brown received a diagnosis of acute myeloma leukemia, unrelated to his HIV. "It was like my second death sentence," he says. When Brown was diagnosed, he was told he had two years to live. Doctors suggested chemotherapy. The usual chemotherapy approaches to treat the leukemia were unsuccessful – leaving doctors with one last option – a bone marrow transplant which came with its own set of risks. Brown was introduced to pioneering hematologist, Dr. Gero Hütter, who was aware of a natural human genetic variant carried by a rare group of human beings, making them resistant to most strains of HIV. He thought it may be possible to find a bone marrow match which had this resistance. Only one per cent of Northern Europeans have two copies of this mutated gene, but Dr. Hütter found a donor in the registry without too much difficulty. Dr. Hütter suggested a bone marrow transplant from such a rare donor could cure both his HIV and leukemia. "I thought he was crazy", Brown laughs. Dr. Hütter was right – the transplant cured the HIV by 2009. The rest is medical history. A paper published in 2009 by Dr. Hütter and his colleagues did not mention the word "cure", but by 2011 the word was finally used in a paper titled: Evidence for the cure of HIV infection by CCR532/32 stem cell transplantation. Two years after the last bone marrow transplant, Timothy made a petition to get to know his anonymous donor. "I don't know if he knows he made history," Brown says. "I know nothing about him, except that he was studying in New York and he was German." "Mr. Brown's case shows us it is possible to cure HIV, but we need to do it safely," says Dr. Brumme. She spoke at the event about HIV cure research globally, including how Mr. Brown's cure has inspired research into gene therapies as part of the strategy to cure HIV. The cure for HIV will not be found in one place, by one person, Dr. Brumme insists. "The global community is in this fight together." | Harm Reduction, Treatment as Prevention® | Forecast Newsletter | Download | ||||||||||||||||||||||
| September, 2019 | BC-CfE Drug Treatment Program Monthly Report (June 2019) | Drug Treatment Program | DTP Status Report | Download | |||||||||||||||||||||||
| September, 2019 | BC-CfE Drug Treatment Program Monthly Report (May 2019) | Drug Treatment Program | DTP Status Report | Download | |||||||||||||||||||||||
| August, 2019 | HIV Monitoring Quarterly Reports, Second Quarter 2019 |
| STOP HIV/AIDS | ||||||||||||||||||||||||
| August, 2019 | BC-CfE Drug Treatment Program Monthly Report (April 2019) | Drug Treatment Program | DTP Status Report | Download | |||||||||||||||||||||||
| July, 2019 | Generational Differences in Sexual Behaviour and Partnering Among Gay, Bisexual and Other Men who have Sex with Men | Do the social and cultural conditions experienced by different generations of men who have sex with men affect their sexual behaviours and partnering? | Epidemiology and Population Health, Momentum | Research Summary | Download | ||||||||||||||||||||||
| July, 2019 | BC-CfE Drug Treatment Program Monthly Report (March 2019) | Drug Treatment Program | DTP Status Report | Download | |||||||||||||||||||||||
| July, 2019 | Comparative Outcomes And Service Utilization Trends (COAST) Fact Sheet | The Comparative Outcomes And Service Utilization Trends (COAST) study is a population-based cohort study that aims to examine the health outcomes and health service use of people living with HIV (PLHIV), including both those who are accessing and not accessing antiretroviral therapy, as compared to the general population of British Columbia. The study comprises two defined cohorts of adults: a cohort including PLHIV and a comparison group consisting of a 10% random sample of adults from the general population of BC followed from 1996 to 2013. COAST contains de-identifed health-related data on antiretroviral and health service use from the BC Centre for Excellence in HIV/AIDS (BC-CfE) and other health administrative data holdings within Population Data BC. The study currently has linked data from 1996 to 2013, with future data linkages planned for additional years. Learn more about the COAST study's aims, objectives and key findings in this fact sheet. | COAST, Epidemiology and Population Health | Treatment as Prevention¨ | Fact Sheet | Download | |||||||||||||||||||||
| June, 2019 | BC-CfE Pharmacovigilance 2018 Annual Report | Pharmacovigilance Initiative, Quality and Safety | Download | ||||||||||||||||||||||||
| June, 2019 | CANOC (Canadian HIV Observational Cohort Collaborative Research Centre) Fact Sheet | CANOC is an initiative of the BC-CfE’sEpidemiology and Population Health Program. It is an integrated network of all registered treatment information from eleven cohort databases across British Columbia, Ontario, Quebec, Saskatchewan and Newfoundland. This collaboration of national researchers and select databases establishes policy-relevant studies in HIV therapeutics, population and public health. Learn more about the CANOC study's aims, objectives and key findings in this fact sheet. | CANOC | Treatment as Prevention¨ | |||||||||||||||||||||||
| June, 2019 | Spring HIV/ARV Update brings latest in HIV research to Vancouver from local and international speakers |
The spring HIV/ARV Update brought expert presentations about scientific findings on hepatitis B and HIV co-infection, breastfeeding policies, HIV cure strategies, and more. China's chief epidemiologist addresses the country's HIV epidemic Dr. Zunyou Wu—Chief Epidemiologist, China Centre for Disease Control and Prevention (China CDC), and Director of Division of HIV Prevention, the National Centre for AIDS/STD Control/China CDC—was a featured speaker at the BC-CfE Spring HIV/ARV Update. He shared China's unique experiences in addressing the HIV and AIDS epidemic, presenting that an estimated 30% of people living with HIV in the country remain undiagnosed today despite a boost in testing efforts. China has ramped up testing efforts: over 240 million HIV tests were completed last year alone. "While the seek and treat approach does work, the population size of China makes it more challenging to control the epidemic," said Dr. Wu. "China needs to do everything possible: education, condom promotion, destigmatizing those infected, among other measures." China began collaborating with BC in 2009 to tackle its rising rates of HIV and was the first nation to formally announce its adoption of the BC-CfE-pioneered Treatment as Prevention (TasP) strategy in 2011. Importance of addressing syndemics of HIV and hepatitis B Recent studies show that 35% of patients are not receiving curative hepatitis B treatment in cases where they are co-infected with HIV. Dr. Mark Hull, a researcher at the AIDS Research Program (a collaboration between St Paul's Hospital and University of British Columbia) spoke of his experience treating an estimated 7–10% of HIV patients who are co-infected with HIV and hepatitis B. Dr. Hull stressed the importance of addressing these syndemic infectious diseases, particularly as HIV has the effect of increased risk of cirrhosis among individuals co-infected with hepatitis B. HIV and hepatitis B both require treatment over a patient's lifetime. Dr. Hull said we need "a system in place to ensure individuals are being appropriately treated for both viral infections, particularly as co-infection increases the risk of progressive liver disease and liver-related mortality." Providing infant feeding support for pregnant women living with HIV Dr. Chelsea Elwood, Clinical Assistant Professor in the Department of Obstetrics and Gynecology at UBC, and health care provider at Oak Tree Clinic, spoke about the challenges faced by her pregnant patients living with HIV when deciding whether to breastfeed their infants. While HIV treatment can make the viral load undetectable and, therefore, untransmittable in blood and sexual fluids, breast milk can remain a vehicle for HIV transmission. Breastfeeding results in about 50% of new HIV perinatal transmissions worldwide, but little research is done in high-income countries where antiretroviral therapy is more accessible. In high-income countries where access to clean water and formula is available, Dr. Elwood recommends formula feeding to eliminate the risk of breastfeeding transmission, with close prenatal and postnatal support to the mother and the family. "What we have found is that every woman really wants the best outcome for her baby," said Dr. Elwood. "We believe that the risk of perinatal transmission of HIV should be zero in the province of BC," continued Dr. Elwood. "We believe that hep B should be the same and we are working really hard to make HCV (hepatitis C virus) the same." Target is now long-term HIV remission Currently, an individual who is on sustained HIV treatment can achieve an undetectable viral load allowing their health and longevity to improve. However, when treatment is interrupted the virus can rebound—which is a barrier to an HIV cure or remission. Dr. Mark Brockman, BC-CfE Associate Researcher and Associate Professor in the SFU Faculty of Health Sciences explained scientists now know that HIV develops a latent (or dormant) viral reservoir. Research continues to build on our knowledge of how the virus diversifies in the body and persists within this reservoir. The question remaining for achieving HIV cure or long-term remission is: "How can we disrupt this latent reservoir?" Dr. Brockman provided an update on potential therapies that could target and eliminate the viral reservoir, saying in vivo and in vitro studies have been promising. Dr. Zabrina Brumme, Director of the BC-CfE Laboratory, spoke to the use of the CRISPR-Cas9 targeted genome editing system as a tool in HIV research, including research towards an HIV cure. Research into the use of gene editing technologies in HIV eradication is supported by a historic case of an HIV cure. A second and more recent possible case of HIV cure achieved through a bone marrow transplant from a donor with a naturally occurring mutation in the human CCR5 gene, rendered the resulting protein non-functional. CCR5 is necessary for HIV to enter cells in the body. The HIV virus uses human proteins at every stage of its life cycle. Dr. Brumme explained how CRISPR-Cas9's research use, knocking out certain proteins, could help identify which ones may be essential to the replication of HIV. Equipped with this knowledge, potential therapies and strategies could be developed to enhance host proteins, knock them out, or even excise the viral genome. "There are many challenges to the CRISPR-Cas9 technology", said Dr. Brumme, "However, it is a powerful technology and easy to use…It is possible, one day in the future, we may see these technologies in the clinic. But we need to be careful, as it raises important ethical questions that will need to be addressed." Watch the HIV/ARV update videos online: http://bit.ly/ARVvideo | Forecast Newsletter | Download | |||||||||||||||||||||||
| June, 2019 | Nevirapine XR (ViramuneTM XR) tablet substitution with Nevirapine 200mg tablets | Notice to Prescribers | Dear Doctor Letter | Download | |||||||||||||||||||||||
| May, 2019 | HIV Monitoring Quarterly Reports, First Quarter 2019 |
| STOP HIV/AIDS | ||||||||||||||||||||||||
| May, 2019 | BC-CfE Drug Treatment Program Monthly Report (February 2019) | Drug Treatment Program | DTP Status Report | Download | |||||||||||||||||||||||
| May, 2019 | BC-CfE Drug Treatment Program Monthly Report (January 2019) | Drug Treatment Program | DTP Status Report | Download | |||||||||||||||||||||||
| May, 2019 | Made-in-BC Treatment as Prevention strategy recognized locally, nationally and globally |
On April 24th, Federal Health Minister Hon. Ginette Petitpas Taylor visited the BC Centre for Excellence in HIV/AIDS (BC-CfE) to speak to Executive Director & Physician-in-Chief Dr. Julio Montaner about BC's leadership in HIV, hepatitis C (HCV) and opioid use disorder (OUD). The BC-CfE has long played an essential role in the testing, diagnosis, treatment and ongoing monitoring of people living with HIV in British Columbia, and is transferring that knowledge to HCV and OUD. Dr. Montaner discussed how the made-in-BC Treatment as Prevention (TasP) strategy and Targeted Disease Elimination (TDE®) platform are providing a framework for the treatment and prevention of other communicable diseases and diseases with a social contagion factor, such as hepatitis C. The TDE® strategy can also be applied to the opioid crisis. For example the BOOST (Best practices in Oral Opioid agoniSt Therapy) Provincial Collaborative, based on the BC-CfE's success from the STOP HIV/AIDS Structured Learning Collaborative, was highlighted as a novel tool in bringing down the number of opioid-related deaths in BC through improved engagement in opioid agonist treatment. In early April, Dr. Montaner, met with City of Vancouver Mayor Kennedy Stewart to discuss the BC-CfE's research and work in the area of public policy with a focus on TasP and TDE®. Recent findings confirm made-in-BC TasP strategy is the path toward ending AIDS. These key meetings preceded a global scientific advance in TasP. The latest findings from a major international study support the already strong case that consistent and sustained HIV antiretroviral treatment prevents new HIV infections. In findings released in The Lancet, the PARTNER study found no cases of HIV transmission through condomless sex among gay couples in which one partner was living with HIV on treatment and the other was HIV-negative. These results follow previous PARTNER study findings showing no cases of HIV transmission in more than 58,000 instances of condomless sex among serodiscordant homosexual and heterosexual couples. "The PARTNER study is bolstered by over a decade-long history of scientific research by the BC-CfE supporting access to HIV treatment as a means to control the epidemic," says Dr. Montaner. "These results show consistent and sustained HIV treatment absolutely eliminates the risk of HIV transmission to sexual partners, equally among heterosexual and homosexual couples." The made-in-BC TasP strategy, pioneered 13 years ago by the BC-CfE—providing earlier and free access to HIV testing and immediate, supported and sustained access to HIV treatment—is key to curbing HIV and ending AIDS. TasP forms the basis of the UNAIDS plan to end AIDS as a pandemic by 2030 by hitting ambitious—but reachable—targets for expanding access to HIV testing and sustained HIV treatment. Through the implementation of TasP with support from the BC Government, BC has successfully reduced HIV transmission—from a peak of more than 850 new cases per year to less than 200 per year in 2018. BC is the only Canadian province to implement TasP and, as a result, has seen the largest decline in new HIV cases in Canada. The study confirms the BC-CfE position, based on 13 years of successful implementation of the TasP strategy in BC, and further bolsters Canada's continuing support for the Undectable equals Untransmittable (U=U) campaign. TasP laid the foundation for U=U and the BC-CfE was an early signatory to the U=U statement. In order to reduce stigma for those living with HIV, it is critical for this message to reach a broad audience that includes the general public and leaders in government. "One of the major hurdles we face in achieving the global goal of ending AIDS is ensuring international funding continues to address the ongoing HIV epidemic," says Dr. Montaner. Globally, there are about 5,000 new HIV cases per day. The arrival of the latest results of the PARTNER study comes ahead of the next round of financing for the Global Fund. The BC-CfE encourages countries around the world to strengthen their financial contributions to the Global Fund, to deliver on the promise of the made-in-BC TasP strategy. | Epidemiology and Population Health | Treatment as Prevention® | Forecast Newsletter | Download | |||||||||||||||||||||
| May, 2019 | Overview: PrEP Prescription Process | PrEP | PrEP Documents and Forms | Download | |||||||||||||||||||||||
| May, 2019 | The BC Home and Community Care System and Older Adults Living with HIV. | THRIVE | Download | ||||||||||||||||||||||||
| April, 2019 | Countering complacency on path to an HIV cure |
The BC-CfE applauds the news that emerged from CROI (Conference on Retroviruses and Opportunistic Infections) and captured global news headlines: an individual living with HIV has been in remission and off treatment for 18 months after receiving a bone-marrow transplant. The "London patient" is now the second individual to achieve HIV remission. To briefly explain, as in the first case, this milestone was achieved through a bone-marrow transplant from a donor harbouring a rare mutation in the human CCR5 gene. Acting as a receptor, the CCR5 is necessary for HIV to enter cells in the human body. It is important to note that HIV cure by bone-marrow transplantation is neither safe nor capable of being easily expanded. The reality is that we still don't know when an HIV cure will be achieved. There is currently no available solution for achieving a broadly applicable cure that could help those living with HIV worldwide. News of the London patient does demonstrate the potential for eradicating HIV from the body, underlining the importance of continuing HIV cure and vaccine research. Under the leadership of BC-CfE Laboratory Director Dr. Zabrina Brumme, the BC-CfE continues to seek to better understand dormant HIV cells that accumulate and persist in the body. While on sustained treatment, an individual can achieve a viral load that is undetectable by standard blood tests, at which point they cannot transmit to others. However, if treatment is stopped or interrupted, viral levels can rebound. Grasping the diversity of HIV residing within an individual (known as the viral reservoir) is a key stepping stone to identifying a cure. Unfortunately, good news of slow progress towards an HIV cure could contribute to misconceptions. Combined with impressive advances in HIV treatment, it could lead some to believe HIV is a resolved issue.Dr. Anthony Fauci, Director of the US National Institutes of Health, told attendees of CROI we have reached a point of "understandable but unacceptable complacency." The bottom line is the HIV epidemic remains a public health concern. There are nearly 37 million people living with HIV in the world, including an estimated 13,000 in British Columbia and over 63,000 people in Canada. More than ever, health care providers, policymakers and the public must be on high alert for complacency. It is equally critical that we take every chance to implement the tools at our disposal to curb HIV and achieve an end to AIDS. In the absence of a vaccine or a cure for HIV, providing early, widespread access to testing and sustained, universal treatment is the most effective means to stop HIV new infections. This is the concept supporting the proven successful, made-in-BC Treatment as Prevention (TasP) strategy that forms the foundation of the UNAIDS 90-90-90 Target to end AIDS by 2030. To meet this goal, by 2020, 90% of individuals living with HIV must be diagnosed, 90% of those diagnosed must be on treatment, and 90% of those on treatment must be virally suppressed. In BC through the implementation of TasP, we have seen a steady increase in individuals accessing HIV testing and antiretroviral treatment, leading to a consistent decline in new HIV cases. HIV treatment today improves longevity and quality of life. However, there is still more we can do. For example, a recent BC-CfE study published in PLOS-ONE uncovered new opportunities in the health care system to diagnose individuals living with HIV. Our study found one in seven individuals living with HIV in BC could have been diagnosed earlier—if health care providers had recognized certain key clinical conditions as triggers for HIV screening. Individuals aged 40 years or older, heterosexuals, people living in remote areas and people who had ever injected drugs were more likely to have had a missed opportunity for an earlier HIV diagnosis. This data provides critical clues on how we can close gaps in access to HIV testing and treatment. It is also a useful reminder HIV does not discriminate. In BC, all individuals are recommended to ask their health care providers for regular HIV tests. We can all get tested for HIV. While scientists and researchers worldwide continue to make remarkable advances in our understanding of HIV, it is too early to celebrate. As we approach the 2020 milestone towards ending AIDS by 2030, we need to accelerate investments and efforts. There is still much more to be done to support the needs of those living with HIV today and to reach our goal of ending AIDS. Dr. Julio Montaner is the Executive Director and Physician-in-Chief of the BC-CfE | SHAPE Study, STOP HIV/AIDS | Treatment as Prevention® | Forecast Newsletter | Download | |||||||||||||||||||||
| March, 2019 | “Condoms are…like public transit. It's something you want everyone else to take.” | Perceptions and use of condoms among HIV negative gay men in Vancouver, Canada, in the era of biomedical and sero-adaptive prevention | Epidemiology and Population Health, Momentum | Research Summary | Download | ||||||||||||||||||||||
| March, 2019 | Celebrated BC-CfE researcher Dr. Robert Hogg named to Order of Canada |
Dr. Robert ("Bob") Hogg was officially inducted into the Order of Canada on February 1st, an accomplishment he doesn't just see as an award but as a national responsibility. "It's very humbling, especially when you start to meet other people who have been inducted, to be a part of that group," he said. Dr. Hogg's work has strongly influenced our understanding of barriers to accessing HIV testing, treatment and care in Canada and the world. "[The BC-CfE] has always had a role of providing research not just for research's sake, but research that will have an impact. I want to make sure that the research I do will have an impact for those living with HIV in BC and even across Canada," said Dr. Hogg, during a small break between meetings at his downtown BC-CfE office. In some ways, the hardworking Dr. Hogg is unexpectedly following his father, Dr. James Hogg, who received the Order of Canada for influencing medical understanding of the lung condition COPD. Ever humble and modest, Dr. Bob Hogg says filling in his father's footsteps was never part of the plan. Nonetheless, from his start as a postdoctoral fellow, Dr. Hogg has had a profound influence on the infrastructure supporting people living with HIV in BC. In 1992, as a demographer with an interest in the population aspects of HIV, Dr. Hogg helped establish the database for the BC-CfE's Drug Treatment Program (DTP). At first, this was simply a filing cabinet to house clinical trial records. Dr. Hogg helped guide the DTP's transformation into a secure database of individuals from across the province who are accessing HIV treatment, which still informs a wealth of studies. Dr. Hogg, who also serves as a professor in the Simon Fraser University Faculty of Health Sciences, is a prolific researcher and a well-respected mentor. Throughout his career, he has taught over 3,000 students and supervised more than 50 graduate students and postdoctoral fellows. As Director of BC-CfE's Population Health and Epidemiology program from 1992 to 2014 and Senior Scientist since 2015, Dr. Hogg has been awarded more than $50 million in grants for province- and Canada-wide studies. In over 500 articles, his published research has laid the groundwork for transforming how we perceive, research and treat HIV. Trained in anthropology, demography and epidemiology, Dr. Hogg has investigated barriers to HIV treatment, health and mental health challenges faced by marginalized people living with HIV, the unique needs and challenges of women living with HIV, and the increasingly emerging issue of people aging with HIV. Dr. Hogg's study in the leading medical journal The Lancet was among the first to demonstrate that lower socioeconomic status decreased length of survival among men living with HIV. Even in his earliest research, Dr. Hogg was crafting questionnaires and surveys "to see [HIV] as more than just a clinical condition, but to see it from a broader social, cultural point of view." "Dr. Robert Hogg is a world-leading scientist and his contributions are among those that helped to create and refine new approaches to HIV treatment and care," said Dr. Julio Montaner, Executive Director and Physician-in-Chief of the BC-CfE. Dr. Hogg's research provides important support to the case for expanding access to HIV treatment, supporting the made-in-BC Treatment as Prevention (TasP) strategy as the most effective means of curbing the global HIV epidemic. Strategies inspired by TasP can now be applied to other contagious or socially contagious diseases, such as hepatitis C and substance use, to achieve Targeted Disease Elimination (TDE®). For example, the BC-CfE's BOOST initiative is looking to apply similar methods to increasing engagement in lifesaving opioid agonist treatment. Dr. Hogg says the most significant progress since he started researching HIV at the epidemic's peak in the 1990s is that people with HIV are living longer due to modern antiretroviral treatment. "Often, you would meet [people living with HIV] at one meeting, and then the next meeting they would be in hospital, and the next they would be dead," he said. Even in light of such important progress, it's crucial scientists are dedicated to dispelling myths and misconceptions. "When you talk to people that are in the general community, they just assume that people [living with HIV] are being treated and cured," said Dr. Hogg. "HIV is not going away, and the TasP approach, pioneered by the BC-CfE, ensures that we have an opportunity to significantly reduce the burden for future generations, said Dr. Hogg. "In an exciting advance, the lessons we have acquired through TasP can now be applied to TDE®." | BOOST, STOP HIV/AIDS | Forecast Newsletter | Download | ||||||||||||||||||||||
| February, 2019 | HIV Monitoring Quarterly Reports, Fourth Quarter 2018 |
| STOP HIV/AIDS | ||||||||||||||||||||||||
| February, 2019 | Repeated Measures Analysis of Alcohol Patterns among Gay and Bisexual Men in the Momentum Health Study | What are the patterns of alcohol consumption among gay, bisexual and other men who have sex with men in Metro Vancouver, Canada? | Epidemiology and Population Health, Momentum | Research Summary | Download | ||||||||||||||||||||||
| February, 2019 | The Additive Effects of Depressive Symptoms and Polysubstance Use on HIV Risk Among Gay, Bisexual and other Men who have Sex with Men | How does the combination of depressive symptoms and polysubstance use relate toHIV risk among gay, bisexual, and other men who have sex with men in Metro Vancouver, Canada? | Epidemiology and Population Health, Momentum | Research Summary | Download | ||||||||||||||||||||||
| February, 2019 | Trends in Awareness and Use of HIV PrEP among Gay, Bisexual and other Men who have Sex with Men in Vancouver, Canada 2012–2016 | In this study conducted before the start of the provincial PrEP program, low rates of PrEP usage were observed. | Epidemiology and Population Health | Research Summary | Download | ||||||||||||||||||||||
| February, 2019 | A Longitudinal Analysis of Cannabis Use and Mental Health Symptoms among Gay, Bisexual and Other Men who have Sex with Men (gbMSM) in Vancouver, Canada | Is cannabis use related to mental health symptoms among gbMSM diagnosed with anxiety or depression? | Epidemiology and Population Health, Momentum | Research Summary | Download | ||||||||||||||||||||||
| February, 2019 | Belief in Treatment as Prevention and its Relationship to HIV Status and Behavioural Risk | How have attitudes towards Treatment as Prevention (TasP) among gay, bisexual and other men who have sex with men changed over time? | Epidemiology and Population Health, Momentum | Research Summary | Download | ||||||||||||||||||||||
| February, 2019 | BC-CfE Drug Treatment Program Monthly Report (December 2018) | Drug Treatment Program | DTP Status Report | Download | |||||||||||||||||||||||
| February, 2019 | BC-CfE Drug Treatment Program Monthly Report (November 2018) | Drug Treatment Program | DTP Status Report | Download | |||||||||||||||||||||||
| February, 2019 | BC-CfE announces provincewide initiative to increase access to lifesaving treatment for opioid use disorder |
On January 17th, the BC-CfE announced the launch of a provincewide initiative, supported by a funding grant from Health Canada's Substance Use and Addiction Program. The first-of-its-kind initiative based on the BC-CfE's world-renowned Treatment as Prevention (TasP) strategy to curb HIV and AIDS—will roll out across all BC regional health authorities in early 2019. This initiative is building upon the successful foundation of a pilot project between the BC-CfE and Vancouver Coastal Health (VCH). The BOOST (Best Practices in Oral Opioid AgoniSt Therapy) Collaborative introduced a proactive model of treatment for opioid use disorder (OUD) to VCH clients at risk of overdose. Health care teams across Vancouver worked to implement system changes to effectively identify, diagnose and engage over 1,100 people in care for OUD—doubling those kept on lifesaving treatment at three months. Through the Collaborative, health care teams created and implemented processes to better reach out to clients (for example, increasing follow-up calls and streamlining client intakes). These incremental changes are providing a path forward to help address the needs of those living with opioid use disorder. The initiative launches in the midst of the ongoing opioid drug overdose crisis, which the Government of BC declared a public emergency in 2016. There have been more than 3,800 confirmed deaths to illicit drug overdose in B.C. since January 1, 2016. "The BC-CfE applied lessons from its proven effective HIV strategy, which drove a steady and consistent decline in HIV and AIDS, to address the urgent opioid overdose crisis affecting individuals and families provincewide," said Dr. Rolando Barrios, Senior Medical Director, BC-CfE. "Small-scale improvements in care, implemented through the work of VCH health care teams, created major, positive impacts on the lives of those affected by opioid use disorder. We can now apply these concepts to every region in BC." Among VCH clinics participating in the BOOST Collaborative, the number of individuals retained in opioid agonist treatment (OAT) at the 90-day mark increased from three out of ten to seven out of ten—a very significant leap in improving access to regular, long-term care for opioid use disorder. "I am extremely proud of the work of the VCH health care teams in successfully engaging with clients to improve their access to lifesaving opioid agonist therapy," said Dr. Patricia Daly, Chief Medical Health Officer and Vice President, Public Health, VCH. Dr. Daly is the Former Executive Lead of the Overdose Emergency Response Centre, established by the B.C. Government in 2017. The BOOST Collaborative is based on an evidence-informed approach. Research shows that the biggest barriers to effective treatment for opioid use disorder are treatment access, dosage and retention. A significant proportion of individuals struggling with opioid use disorder will reduce illicit opioid use and remain on treatment longer with appropriate doses of methadone, buprenorphine/naloxone or slow-release oral morphine (all categorized as OAT). The risk of morbidity and mortality decreases by 80% for individuals on effective OAT. Recent data from the BC Coroner's office found that, of the 1,800 deaths reviewed over a 19-month period (January 2016 to July 2017), none had buprenorphine present in their system. Despite the known benefits of OAT, at baseline and before the launch of the Vancouver BOOST Collaborative, only 30-40% of individuals in Vancouver who started OAT remained on treatment at three months. "Programs that help to meet clients where they are and address their needs effectively are fundamental to our progress against HIV with the Treatment as Prevention strategy," said Dr. Julio Montaner, Executive Director and Physician-in-Chief, BC-CfE. "The achievements of the BOOST Collaborative show the benefits in applying these principles to improving care and quality of life for individuals with opioid use disorder." The provincial BOOST Collaborative aims to improve upon already impressive achievements of the VCH/BC-CfE pilot project, with the goals that 95% of clients on OAT will have an active OAT prescription and 95% of those clients with an active OAT prescription will be retained on therapy for longer than three months. The newly launched BOOST Collaborative will be holding regular meetings among health care teams located at clinics across the province to share best practices. The BC-CfE will provide support as the teams work on identifying and addressing gaps in reaching clients within their own clinical settings | Laboratory | Harm Reduction, Treatment as Prevention® | Forecast Newsletter | Download | |||||||||||||||||||||
| December, 2018 | BC-CfE Drug Treatment Program Monthly Report (October 2018) | Drug Treatment Program | DTP Status Report | Download | |||||||||||||||||||||||
| November, 2018 | China CDC and BC-CfE renewed partnership reaffirms commitment to fight HIV |
China is facing an HIV epidemic that is on the scale of its population of approximately 1.4 billion. The BC-CfE is providing valuable insights on successful tactics, programs and strategies implemented in British Columbia to curb HIV. Namely, the BC-CfE's Treatment as Prevention (TasP) strategy has transformed the province from the one with the highest number of new HIV diagnoses to one of the lowest (despite being one of the most populous provinces). On October 29th, delegates from the BC-CfE traveled to Beijing to meet with members of the National Centre for AIDS/STD Control/Prevention and Chinese Centre for Disease Control and Prevention (NCAIDS/China CDC) and renewed their partnership to address HIV and AIDS. The BC-CfE and NCAIDS/China CDC signed a memorandum of understanding to collaborate on health priorities affecting China and British Columbia in relation to HIV/AIDS and hepatitis C virus (HCV). "China will continue to use the best science and evidence from around the world and implement strategies that have a real impact on curbing the transmission of HIV and AIDS," said Dr. Zunyou Wu, Chief Epidemiologist China CDC and Director of Division of HIV Prevention, NCAIDS/China CDC. "For people to be able to participate fully in the labour force and to proactively participate in their communities, health is a very important thing," said Jim Nickel, Deputy Head of Mission, China, with Global Affairs Canada who spoke at the October MOU signing in Beijing. Mr. Nickel said the work by China and Canada is important for sustainable development. The collaboration between BC and China began in 2009 and China was the first nation to formally announce its adoption of the BC-CfE-pioneered TasP strategy in 2011. This was followed by the signing of the first MOU between the BC-CfE and China in 2013. Since then, the BC-CfE and China have collaborated in adapting the TasP strategy developed in British Columbia to be applicable in China—with promising results. China embedded the TasP strategy into their national HIV/AIDS policy, and has seen large-scale increases in HIV testing with 200 million HIV tests performed in 2017 alone. This effort has been accompanied by the immediate offer of antiretroviral treatment (ART) to people living with HIV, with 610,000 people living with HIV in China covered by ART in 2017. In 2017 alone, 131,000 people living with HIV in China were newly enrolled on ART. For several successive years, new HIV diagnoses have increased in China, attributable to increased access to testing. Prior to access to testing, individuals may have been unaware they were living with HIV for a number of years. China is committed to expanding the number of individuals accessing testing and treatment in order to attain the 90-90-90 Target of 90% of people living with HIV diagnosed, 90% of those diagnosed on treatment, and 90% of those on treatment virally suppressed. Joint research projects between the BC-CfE and China during their previous partnership showed increased access to testing and treatment initiation. In particular, a trial in the Guangxi region to eliminate wait times and extra steps in the testing and diagnosis process had positive results. The intervention helped avert new cases of HIV and save in costs due to avoided illness; the process of testing resulted in a 91% increase in ART initiation and a 62% drop in mortality. The China and BC-CfE MOU renews a three-year fellowship program bringing three of among China's top scientists to Vancouver to collaborate with researchers and clinicians at the BC-CfE. "Our partnership with Dr. Zunyou Wu and his colleagues is based on mutual trust and collaboration and a deep commitment to ending HIV/AIDS using evidence-based research and strategies known to be effective in the fight against HIV/AIDS, such as TasP," says Dr. Julio Montaner, Director of the BC-CfE. "We will continue to work jointly, as we have for several years now, to improve the health of British Columbians and Chinese citizens. We can collaborate to advance strategies like TasP—and the various initiatives that have evolved from this approach—in order to reduce new cases of HIV." Controlling HIV transmission remains a primary objective in reducing China's HIV epidemic. As part of the Canadian delegation to China, BC-CfE researchers and scientists Drs. Viviane Dias Lima and Jeffrey Joy provided specialized knowledge on how to address HIV. "Through our use of phylogenetics, we have been able to demonstrate a way to identify current hotspots of HIV transmission. In British Columbia, this has allowed us to target these emerging epidemics through early health interventions," said Dr. Jeffrey Joy, BC-CfE Research Scientist. "We hope that sharing our knowledge with our colleagues in China, will provide them yet another tool to efficiently and cost-effectively target hotspots of HIV and hepatitis C transmission." "Identifying those living with HIV through widespread and normalized testing approaches helps to expand treatment and to have a positive impact on the HIV epidemic," says Dr. Viviane Dias Lima, Research Scientist and Senior Statistician at the BC-CfE. "These core fundamentals of TasP are vitally important in controlling HIV in a population of China's size." As the Chinese government continues to make a serious domestic commitment to funding HIV treatment and prevention efforts, NCAIDS/China CDC is tasked with ensuring the scale up of these efforts are cost-effective and reach across demographic groups. Principles of TasP are also being applied to addressing reinfection in the hepatitis C epidemic, another bloodborne pathogen that can now be effectively cured with access to the latest generation of treatments or DAAs (direct acting antivirals). The BC-CfE has consistently developed programs to connect hard-to-reach populations to HIV care and treatment—and is applying the strategy to addressing hepatitis C reinfection as well as the spread of other communicable and socially communicable diseases. Investing in reducing the burden of new infections has enormous long-term benefits. The made-in-BC TasP strategy has been shown to be not only cost-effective, but also cost-saving. Through collaboration with colleagues in China, the BC-CfE will ensure the lessons learned in BC will help guide the NCAIDS/China CDC in curbing the spread of HIV and hepatitis C, including the use of some of the most cutting-edge science such as phylogenetics. | Clinical Education & Training, International Program | Treatment as Prevention® | Forecast Newsletter | Download | |||||||||||||||||||||
| November, 2018 | BC-CfE Drug Treatment Program Monthly Report (September 2018) | Drug Treatment Program | DTP Status Report | Download | |||||||||||||||||||||||
| November, 2018 | BC-CfE Drug Treatment Program Monthly Report (August 2018) | Drug Treatment Program | DTP Status Report | Download | |||||||||||||||||||||||
| November, 2018 | BC-CfE Drug Treatment Program Monthly Report (May 2018) | Drug Treatment Program | DTP Status Report | Download | |||||||||||||||||||||||
| November, 2018 | BC-CfE Drug Treatment Program Monthly Report (July 2018) | Drug Treatment Program | DTP Status Report | Download | |||||||||||||||||||||||
| November, 2018 | BC-CfE Drug Treatment Program Monthly Report (June 2018) | Drug Treatment Program | DTP Status Report | Download | |||||||||||||||||||||||
| November, 2018 | HIV Monitoring Quarterly Reports, Third Quarter 2018 |
| STOP HIV/AIDS | ||||||||||||||||||||||||
| November, 2018 | Recap on the Fall HIV/ARV Update |
For over a decade now, health care providers, researchers, scientists, service providers and members of the community have come together twice yearly at the BC Centre for Excellence in HIV/AIDS (BC-CfE) for a day-long conference on the status of HIV and related conditions in BC. On October 22nd, this year's Fall HIV/ARV Update focused on HIV and syndemic issues of substance use disorders, viral hepatitis and mental health. Advancing access to PrEP and ARTIn a relatively new BC-CfE initiative, pharmacist Junine Toy shared news on the continued rapid uptake of PrEP (pre-exposure prophylaxis) since becoming publicly available in BC in January. Close to 3,000 British Columbians have been prescribed the HIV prevention drug, with new prescribers coming on each month from across the province. PrEP is a new Government of BC supported initiative in the Treatment as Prevention (TasP) strategy. And, in combination with expanding access to HIV testing and treatment through TasP, will play a role in curbing the HIV epidemic. As part of the update, the BC-CfE Education and Training Team invited nurse practitioners to access training in order to prescribe PrEP and antiretroviral treatment (ART). This new BC-CfE program, launched this fall in partnership with the College of Registered Nurses of BC (now the British Columbia College of Nursing Professionals), is aiming to increase PrEP and ART prescribers. The goal is to reach individuals living with HIV or at-risk of HIV in underserved areas. Addressing syndemic issues and BC's opioid crisisBC-CfE Director Dr. Julio Montaner highlighted the encouraging pace of progress in BC and in Canada towards reaching the UNAIDS 90-90-90 goals to end AIDS by 2030. "AIDS-related deaths are at an all-time low in BC. The challenge is we are seeing increased non-AIDS-related conditions as drivers of mortality," said Dr. Montaner. "There is an urgent need on our part to expand our strategy to be more attentive to the needs of the patients with mental health and substance use issues." These factors are pertinent to the BC-CfE's continued expansion into Vancouver's Downtown East Side. Two years since a public health emergency was declared, BC Provincial Health Officer Dr. Bonnie Henry reflected on the ongoing opioid overdose crisis in the province. The crisis is being driven by illicit drug use and overdose deaths are predominantly among young men. Indigenous populations are "overwhelmingly overrepresented". According to Dr. Henry, life-saving naloxone is key to reducing deaths in the short-term, but further engagement in substance use treatment and expansion of mental services are needed. "That we are not seeing increases in HIV and hepatitis C is testament to the success of harm reduction programs," said Dr. Henry BC-CfE's BOOST Initiative seeing success Aiming to optimize access to harm reduction through opioid agonist treatment, the BC-CfE-led BOOST Initiative is making headway. The initiative has helped clinics better retain individuals with substance use disorders through ground-up quality improvement. Incremental changes led by clinic staff, such as adding reminder calls for appointments or follow-up calls for patients, have made a difference. "Data drives change," said Dr. Rolando Barrios, Assistant Director of the BC-CfE. "In quality improvement, we are not in the quest of new knowledge but in the quest of applying existing knowledge." The goal is to have 95% of patient retained on opioid agonist therapy for three months or more. The program is now reaching almost 80% retention at three months, compared with a rate of approximately 30% at its start. Based on its success, BOOST will see further expansion throughout the province in the coming months. Applying principles of Treatment as Prevention to addressing hepatitis CBC-CfE researcher and clinician Dr. Mark Hull explained there has been strong uptake along the cascade of care for hepatitis C in BC; however, not everyone is benefitting equally. Women, people with substance use disorders and Indigenous people are not being offered care for hepatitis C at the same rates. "There is not universal access to DAAs [direct acting antivirals]," said Dr. Hull. "Hep C treatment should fall under the repertoire of experienced family care doctors." DAAs offer higher cure rates, shorter treatment times and fewer side effects than previous generations of hepatitis C treatments. Currently, the BC-CfE Per-SVR study is looking at the threshold of prevention and harm reduction interventions that will prevent reinfection. Expanding access to hepatitis C testing and treatment is another element of a Targeted Disease Elimination strategy, based on the principles of TasP. | Forecast Newsletter | Download | |||||||||||||||||||||||
| October, 2018 | Are we close to the end of AIDS? |
Just two years ago, UNAIDS announced a window of opportunity to end the AIDS epidemic by 2030 by fast-tracking towards meeting the 90-90-90 Target. There was tempered optimism this ambitious goal was within reach. Now, the international HIV community is experiencing a sense of urgency: complacency is moving us perilously close to an HIV rebound. This was a main focus when experts, advocates and community gathered for the most recent AIDS conference in Amsterdam this past summer. According to the World Health Organization, there are too many people not accessing care which will impede reaching the Target goals of 90% of all those living with HIV being diagnosed, 90% of all those diagnosed accessing treatment and 90% of those on treatment achieving viral suppression. Some leading governments have stalled funding towards helping to expand access to treatment for ending AIDS. After widening access to treatment in Africa from a baseline of 50,000 to 14 million, funding for PEPFAR, the United States President's Emergency Plan for AIDS Relief, has generally plateaued for the past decade. This, despite the fact that HIV treatment is still not accessible in many health care settings in low- and middle-income countries. At a time when we have reached consensus on the made-in-BC 90-90-90 Target as a means to end AIDS as a pandemic, the international community's investment is faltering. Canada needs to lead the charge in asking for the expansion of the funding envelope to provide universal coverage for effective HIV treatment and prevention drugs. At the last Global Fund Replenishment Conference in 2016, Canada boosted its international funding for fighting HIV by 20%. Canada must be a model in ending AIDS here at home and deliver on the promise of the Treatment as Prevention (TasP) strategy. The winning and cost-effective TasP strategy, implemented in BC, involves expanding access to testing and the immediate, universal provision of HIV antiretroviral treatment upon diagnosis. More recently, seven Canadian provinces, including BC, expanded coverage of the HIV prevention drug, PrEP (pre-exposure prophylaxis). The goal set to end AIDS by 2030 is not an arbitrary one. With a growing global population and strains to be imposed by climate change, we need to end AIDS before resources are shifted. Climate change will impact progress on global health in ways both expected and unexpected. Food insecurity and drought can make it difficult to use HIV antiretroviral medications, even when available, as many must be taken with food. Triggered by the effects of changes in weather and landscape, mass migration is anticipated to increase. Beyond the absence of action, discriminatory laws and policies in some world regions are targeting vulnerable groups such as people who use drugs and the LGBTQ community. Eastern Europe and Central Asia are seeing sharp increases in new HIV cases. By the end of 2017, official estimates from Russia showed around 1 million people living with HIV and only about one third receiving treatment, well below the 90-90-90 Target. Each year the country is seeing around 100,000 HIV cases, one of the highest rates of new infections in the world. North America is experiencing pockets of HIV growth, for example in regions of Western Canada and the Southern United States. Marginalization and a lack of access to testing, treatment, care and other supports creates an environment for the HIV virus to spread and thrive. BC can show the world what is possible by reducing our yearly number of new HIV cases to double digits. We have seen a steady decline from around 900 at the peak of the epidemic to around 200 cases in 2016. Mathematical modelling shows that TasP when combined with PrEP could catalyze our progress towards ending AIDS. Also, integral to stopping HIV are outreach programs to address the basic needs of the most hard-to-reach populations, including barriers to treatment such as lack of housing or poverty. This is not a drill. We know what will end AIDS is reducing stigma while expanding access to testing and treatment. Now, we need upfront investment in effective programs that could help locally, nationally and globally. Canada must lead by example by ensuring free access to TasP and PrEP nationwide to end AIDS and curb the spread of HIV. | Momentum, Pharmacovigilance Initiative, STOP HIV/AIDS | Treatment as Prevention® | Forecast Newsletter | Download | |||||||||||||||||||||
| October, 2018 | HIV Testing Among a Representative Community Sample of Gay, Bisexual, and Other Men Who Have Sex with Men in Vancouver, Canada | What are the driving factors behind gay and bisexual men's decision to test or not test for HIV? | Epidemiology and Population Health, Momentum | Research Summary | Download | ||||||||||||||||||||||
| October, 2018 | HIV Treatment Optimism and Crystal Methamphetamine Use and Initiation among HIV-Negative Men who have Sex with Men in Vancouver, Canada: A Longitudinal Analysis | Has increased HIV treatment optimism changed crystal methamphetamine use among men who have sex with men in Metro Vancouver? | Epidemiology and Population Health, Momentum | Research Summary | Download | ||||||||||||||||||||||
| October, 2018 | Dolutegravir-containing Products (Tivicay®, Triumeq®) in Pregnancy and Use in Women of Reproductive Age | For more information: click here to link to BC-CfE Drug Safety Alerts | Notice to Prescribers | Dear Doctor Letter | Download | ||||||||||||||||||||||
| October, 2018 | HIV Pre-Exposure Prophylaxis (PrEP) | Notice of Program Launch | Dear Doctor Letter | Download | |||||||||||||||||||||||
| October, 2018 | Associations between Sexual Partner Number and HIV Risk Behaviours: Implications for HIV Prevention Efforts in a Treatment as Prevention Environment | Is the number of sexual partners still an important measure of sexual risk among gay, bisexual and other men who have sex with men in Metro Vancouver, Canada? | Epidemiology and Population Health, Momentum | Research Summary | Download | ||||||||||||||||||||||
| September, 2018 | Dr. Zabrina Brumme to lead world-renowned BC-CfE Laboratory Program |
The first time Dr. Zabrina Brumme entered the BC Centre for Excellence in HIV/AIDS (BC-CfE), she had no idea she would one day be the director of its innovative Laboratory Program. She was only seventeen at the time and had not yet embarked on a career in HIV research that would introduce her to many international leaders in the field. She laughs about it now, convinced that as a wide-eyed teenager she likely didn't make much of an impression on one of the luminaries in HIV research, Dr. Julio Montaner. "I am pretty sure Julio doesn't remember that meeting," she said. "But he was gracious enough to meet with a young, ambitious student interested in interviewing an expert as part of a high school thesis project on HIV." Born and raised in Vancouver, Dr. Brumme's original goal was to teach biology and English literature. While completing a bachelor of science at the University of British Columbia (UBC), it was a co-op work placement at the BC-CfE that exposed her to a career in HIV/AIDS research, sparking a lifelong passion. After graduating from UBC, Dr. Brumme traveled and then eventually circled back to the BC-CfE to do research and help with the clinical genotyping program. Even then, her career focus remained on ultimately becoming a high school teacher. The BC-CfE's Founding Director at the time, Dr. Michael O'Shaughnessy, had a habit of checking in with students to talk to them about career and future ambitions. "He gave me advice that drove me toward a career in science," said Dr. Brumme. O'Shaughnessy told Dr. Brumme that a path to becoming a scientist could lead to teaching; while pursuing teaching may make the path back to science difficult. With a revised career plan, Dr. Brumme acquired a Ph.D. in experimental medicine from UBC and went on to complete a post-doctoral fellowship at the Ragon Institute of Massachusetts General Hospital (MGH), MIT and Harvard University, under the mentorship of the highly recognized HIV researcher Dr. Bruce Walker. Dr. Brumme says that experience keeps on giving – she still collaborates with many former colleagues met at Harvard and continues to cultivate those rich international networks. Under Dr. Walker's direction, Dr. Brumme had three years of exploration in science and mentorship, with access to a wealth in ideas and resources. Her former mentor sees her new role as BC-CfE Laboratory Program Director as a great fit: "Zabrina brings enormous scientific talent and creativity to this role, but equally important is her gift for stewarding effective scientific collaboration locally, nationally and internationally," said Dr. Walker, Director of the Ragon Institute. "She is a clear leader, committed to creating knowledge while invested in the success of others." During her time at Harvard, Dr. Brumme collaborated internationally with Dr. Thumbi Ndung'u, Scientific Director of the HIV Pathogenesis Programme at the University of KwaZulu Natal in South Africa. He echoes the theme of her strength as a collaborator, who holds both herself and her team to very high standards. "Zabrina is a fantastic teacher and a visionary with a generous spirit. She brings people together," said Dr. Ndung'u. "She is a great choice to lead the BC-CfE and I have no doubt that with this appointment, the Centre will grow in its scientific contributions and expand its collaborations and influence in fighting HIV/AIDS in Canada and globally." By 2009, Dr. Brumme was back at home – this time at SFU – where HIV researchers including Drs. Bob Hogg and Jamie Scott were helping establish a vibrant interdisciplinary HIV research team in SFU's new Faculty of Health Sciences. Brumme landed her assistant professorship there in 2009, where she is now an associate professor. In her new role at the BC-CfE, on secondment from SFU, Dr. Brumme looks to continue the BC-CfE's outstanding clinical work in HIV genotyping and personalized medicine, as well as cutting-edge research in HIV and hepatitis C drug resistance and viral genetic diversity. She hopes to uphold the BC-CfE tradition of producing highly respected, scientifically rigorous and newsworthy research. The BC-CfE persists as a global leader in HIV, in particular through its research and advocacy around Treatment and Prevention (TasP) and is applying the proven effective principles of TasP to its Targeted Disease Elimination strategy of other blood-borne and socially contagious illnesses, such as hepatitis C and type 2 diabetes. With the addition of Dr. Brumme, the BC-CfE is further expanding in the exciting direction of HIV cure and vaccine research. "The global reputation of the BC-CfE Laboratory Program is outstanding," said Dr. Brumme. "The vision and foresight of Drs. Michael O'Shaughnessy and Julio Montaner propelled the province of BC towards becoming one of the best places in the world for HIV research and treatment." Dr. Brumme and her colleagues recognize the message her appointment sends to young scientists, particularly girls and women. "Zabrina is a role model for young female scientists," said Dr. Mary Carrington of the US Frederick National Laboratory for Cancer Research. "She is an adept, approachable mentor, committed to her work and scientific progress." "I do not hesitate to share my challenges and personal and professional experiences as a researcher with emerging scientists, while still pushing forward rigorous work," says Dr. Brumme. "Although there have been gains for women in the STEM fields, I would like to see more. We need to continue to create opportunities for women to take leadership roles in the advancement of science." | Clinical Education & Training, Laboratory | Treatment as Prevention® | Forecast Newsletter | Download | |||||||||||||||||||||
| August, 2018 | Gay Men's Understanding and Education of New HIV Prevention Technologies in Vancouver, Canada | There are still a number of barriers to be addressed in the uptake of HIV prevention methods and technologies. | Epidemiology and Population Health, Momentum | Research Summary | Download | ||||||||||||||||||||||
| August, 2018 | Seroadaptive Strategies of Vancouver Gay and Bisexual Men in a Treatment as Prevention Environment | HIV risk reduction strategies are evolving with important implications for HIV research to be further investigated. | Epidemiology and Population Health, Momentum | Research Summary | Download | ||||||||||||||||||||||
| August, 2018 | A Latent Class analysis of Sexual and Romantic Relationships among HIV-Positive and HIV-Negative Gay and Bisexual Men in Vancouver | Relationships among gay, bisexual and other men who have sex with men are diverse, displaying a range of behaviours and preferences about sex and sexual pleasure that should be further explored in research. | Epidemiology and Population Health, Momentum | Research Summary | Download | ||||||||||||||||||||||
| August, 2018 | An Event-Level Analysis of the Interpersonal Factors Associated with Condomless Anal Sex among Gay, Bisexual and other Men who have Sex with Men with Online-Met Partners | Condomless anal sex among gbMSM with partners met online is associated with a variety of interpersonal factors to be considered in health interventions. | Epidemiology and Population Health, Momentum | Research Summary | Download | ||||||||||||||||||||||
| August, 2018 | Changes in Smoking Status among a Longitudinal Cohort of Gay, Bisexual, and other Men who Have Sex with Men in Vancouver, Canada | Cigarette smoking remains a serious public health concern and gbMSM are more likely to smoke than the general population. | Epidemiology and Population Health, Momentum | Research Summary | Download | ||||||||||||||||||||||
| August, 2018 | Estimating the Size of the gbMSM Population in Metro Vancouver, Canada, Using Multiple Methods and Diverse Data Sources | Evidence from British Columbia and elsewhere has demonstrated the expansion of access to antiretroviral HIV treatment (ART) can result in population-level reductions in HIV incidence. This is the concept behind the made-in-BC Treatment as Prevention strategy, or TasP, which aims to expand early HIV testing and treatment to improve patients' health and curb the spread of HIV. Gay, bisexual and other men who have sex with men (gbMSM) represent the most affected HIV risk group, both in BC and Canada. The BC-CfE Momentum Health Study is designed to measure changes in HIV risk behaviour, attitudes toward TasP® and the proportion of HIV-positive gbMSM with unsuppressed viral load over time in the Vancouver region. The study uses respondent-driven sampling (RDS) to obtain a more representative sample reflecting the diversity of the gbMSM community in Vancouver. | Epidemiology and Population Health, Momentum | Research Summary | Download | ||||||||||||||||||||||
| August, 2018 | HIV Monitoring Quarterly Reports, Second Quarter 2018 |
| STOP HIV/AIDS | ||||||||||||||||||||||||
| August, 2018 | BC-CfE Pharmacovigilance 2017 Annual Report | Pharmacovigilance Initiative, Quality and Safety | Download | ||||||||||||||||||||||||
| July, 2018 | BC Minister of Health announces swift progress on PrEP program |
On June 26th, BC Health Minister Adrian Dix joined BC-CfE Director Dr. Julio Montaner to mark very encouraging progress on the uptake of HIV pre-exposure prophylaxis (PrEP) and post-exposure prophylaxis (PEP) in BC, since the January 1st launch of the publicly funded program. At the press event, which took place at Jim Deva Plaza in Vancouver's West End, the Minister of Health announced that the province has seen strong uptake of PrEP as the program continues to grow. Currently there are about 100 new PrEP prescriptions filled each week, with new prescribers also joining at a steady rate across the province. More than 2,000 individuals have been prescribed PrEP in BC between January 1 and July 1. "With the expanded access to PrEP and PEP, we are making important investments to the publicly funded health system, not only because it is the right thing to do, but also because people depend on us to help them live their healthiest possible lives, and that is something we're committed to do," said BC Health Minister Adrian Dix. Since the introduction of highly active antiretroviral therapy (HAART), which Dr. Montaner played the key role in developing, the number of new cases of HIV seen annually in BC has dropped from nearly 900 to fewer than 200. The BC Government, under NDP leadership, supported efforts to make HAART available to individuals living with HIV when the BC-CfE introduced it in 1996. The provincial expansion of coverage for PrEP and PEP in BC, has added a new resource to the Treatment as Prevention® (TasP®) strategy. PrEP is a daily oral antiretroviral medication that is highly effective in reducing new cases of HIV, up to nearly 100% in some clinical trials. PEP is a course of antiretroviral treatment provided following a possible HIV exposure in order to prevent infection. "The coverage of PrEP and expanded coverage of PEP has been something that many people in this community have advocated for some time," said Spencer Chandra Herbert, MLA for Vancouver-West End. "I am proud that, earlier this year, our government was able to make this treatment more readily available." The inclusion of PrEP in the TasP® envelope is a winning tactic for achieving the end of AIDS. When the PrEP program reaches 5,000 individuals, mathematical modelling from the BC-CfE projects the province will achieve a greater than 83% reduction of new HIV cases by 2026. BC is the only Canadian province to implement TasP®, providing universal access to antiretroviral treatment immediately upon diagnosis, and the only one to see a consistent decline in new cases. Dr. Montaner emphasized the importance of not losing focus in the fight against HIV and AIDS, in spite of significant and encouraging gains. "We need to keep the pedal to the metal," he said. "The work we have done in HIV and AIDS proves the political will and expertise exists in BC to expand the principles of TasP® to other contagions," said Dr. Montaner. "If we can curb HIV, imagine the global leadership BC can show in tackling other communicable diseases, such as viral hepatitis, through expanding access to testing, treatment and prevention." PrEP has been available at no cost when requested through the BC-CfE for eligible British Columbians, including men who have sex with men, transgender women, people with ongoing relationships with HIV-positive sex partners and people who inject drugs with a known HIV-positive partner. "We are fortunate here in BC to now have access to many tools in HIV prevention—including TasP®, PrEP and PEP," said Hesham Ali, Peer Navigator with the Positive Living Society of BC who has been living with HIV since 1999. "This is thanks to the support of the provincial government and the work of organizations such as the BC-CfE and Providence Health Care. Just as TasP® has been a life-changer for people living with HIV, PrEP makes a huge difference in HIV prevention." According to data from the BC-CfE's Drug Treatment Program, of the individuals who have accessed PrEP, the median age is 34. In the program, 73% of the users are new, 70% reside in Greater Vancouver and 99% are male. | CHIWOS, Viral Hepatitis Research Program (VHRP) | Hepatitis, PrEP, Treatment as Prevention® | Forecast Newsletter | Download | |||||||||||||||||||||
| July, 2018 | PrEP Lab Requisition Forms | PrEP | PrEP Documents and Forms | Download | |||||||||||||||||||||||
| July, 2018 | Generic antiretroviral products on BC-CfE Formulary | Notice to Prescribers | Dear Doctor Letter | Download | |||||||||||||||||||||||
| June, 2018 | BC-CfE Drug Treatment Program Monthly Report (April 2018) | Drug Treatment Program | DTP Status Report | Download | |||||||||||||||||||||||
| June, 2018 | BC-CfE Drug Treatment Program Monthly Report (March 2018) | Drug Treatment Program | DTP Status Report | Download | |||||||||||||||||||||||
| June, 2018 | Spring ARV Update: Publicly-funded PrEP off to strong start in BC |
An HIV prevention program, available at no cost to people at high risk of HIV, is enrolling over 400 participants – primarily men who have sex with men (MSM) – every month right across BC. PrEP (pre-exposure prophylaxis) is a daily oral antiretroviral medication that prevents new HIV infection when taken consistently. "Treatment as Prevention® has worked remarkably well here at home and around the world to bring down the rate of new HIV infections; however, we see a persistent rate of ongoing transmissions among MSM," says Dr. Julio Montaner, Director of the BC Centre for Excellence in HIV/AIDS (BC-CfE). "Our research shows PrEP will drastically reduce new cases of HIV in BC." Since it's official rollout in January of 2018, over 1,500 people have enrolled in the publicly funded PrEP program across BC. The median age of enrollees is 34 and 99% of them are male. Approximately 30% have accessed PrEP before while a larger number (70%) are new to the program. Junine Toy, Senior Manager of the BC-CfE Drug Treatment Program (DTP), expected to see a small number of prescribers join the PrEP program initially and was surprised by the results. One of the foundational programs of the BC-CfE, the DTP is funded by the provincial government (PharmaCare) to distribute anti-HIV drugs based on guidelines generated by the Therapeutic Guidelines Committee. "We thought we would only get a small number of prescribers with a high number of patients, but we have seen over 300 prescribers across the province, many with only one or two PrEP clients," says Toy. "This is truly heartening because it tells us people in BC are having important conversations with their family doctors about their health, preventatively and proactively." Most eligible individuals fall into the following groups — MSM, transgender women, those who have used NPEP (non-occupational post-exposure prophylaxis) more than once, people with ongoing relationships with HIV positive sex partners without a suppressed viral load and people who inject drugs with a known HIV-positive partner without a suppressed viral load. Many PrEP clients are assessed and provided with a HIRI-MSM score (HIV Incidence Risk Index for men who have sex with men) to determine their eligibility. Enrollees must have MSP coverage, reside in BC, be HIV-negative and be able to withstand the effects of the medication. Once eligibility is established, the approval process is efficient, according to Toy. Once approved, clients should pick up their prescription promptly to prevent any delay in initiation and continue to be monitored regularly. After the initial screening, clients are checked after one month for HIV infection, renal function, tolerability, adherence, and ongoing risk, and then every three months thereafter. "Doctors in BC can submit a request and within a few days, get approved and navigate the process by accessing the BC-CfE website, RACE (Rapid Access to Consultative Access), REACH (Rapid Expert Advice and Consultation for HIV) and the St. Paul's Hospital Pharmacy PrEP phonelines for any additional information," says Toy. "Physicians should monitor PrEP clients every three months – tying together the follow-up and prescription refills, allowing doctor and patient to reconnect frequently." MSM community groups and HIV researchers alike see the program as a pivotal part of ending the HIV epidemic among the MSM population in BC. "Gay, bisexual and other men who have sex with men are disproportionally affected by the HIV epidemic in BC, with 46% of new cases occurring in this population," says Montaner. "We developed a mathematical transmission model and determined the combination of Treatment as Prevention® and PrEP could lead to HIV elimination in BC among MSM over the next ten years (or by 2026)." PrEP joins existing programs offered by the BC-CfE such as PEP (post-exposure prophylaxis) which has been developed and managed by the BC-CfE for twenty years. It provides HIV prevention medication in instances of sexual assault and occupational exposure. NPEP (non-occupational post-exposure prophylaxis) covers individuals who may have been exposed to HIV through consensual drug use or sexual encounters. NPEP started out as a pilot project and expanded provincially to coincide with the launch of PrEP. | Drug Treatment Program, RETAIN, STOP HIV/AIDS | Forecast Newsletter | Download | ||||||||||||||||||||||
| May, 2018 | HIV Monitoring Quarterly Reports, First Quarter 2018 |
| STOP HIV/AIDS | ||||||||||||||||||||||||
| May, 2018 | Guidelines for Management of Acute HIV Infections | Therapeutic Guidelines MenuThese guidelines were created by a group of experts at the BC Centre for Excellence in HIV/AIDS to provide evidence-based recommendations for the assessment, diagnosis and management of individuals newly diagnosed with acute HIV infection (symptomatic or non-symptomatic). | Download | ||||||||||||||||||||||||
| May, 2018 | BC-CfE Drug Treatment Program Monthly Report (February 2018) | Drug Treatment Program | DTP Status Report | Download | |||||||||||||||||||||||
| April, 2018 | Eye clinic provides life changing care in the Downtown East Side |
When an anonymous donor helped the BC Centre for Excellence in HIV/AIDS (BC-CfE) establish a space for marginalized populations in the Downtown Eastside to provide healthcare, the BC-CfE worked with Dr. David Maberley, a highly credentialed ophthalmologist, to include an eye clinic. The Downtown Eastside Eye Clinic (DEEC), located at 623 Powell Street (accessible through the alley of the main building), has since – on an almost daily basis – seen patients who haven't had their eyes checked in years, if ever. Dr. Maberley worked closely with the BC-CfE in planning and developing the eye clinic space, whom he cites as being excellent leaders in helping to provide services to marginalized populations. "We are grateful to the BC-CfE for allowing us to be here and we hope they want to work with us for many years to come," he says. Dr. Maberley has been providing outreach for most of his career, including at the former location of the DEEC at the Vancouver Native Health Society, VNHS (established in 2000). By offering eye care in an accessible setting, a basic health care service can result in life changing diagnoses and treatment for individuals who may be homeless, under housed or face other challenges. Tamara Loyer first heard about the clinic while she was living in supportive housing. She visited as a form of preventative care and found it to be "in no way intimidating" with very little wait time. At the time, it was discovered Loyer had a painless tear on her retina that was later corrected through laser eye surgery at St. Paul's Hospital. She was referred to the hospital's retina clinic on an urgent basis. "The referral [the DEEC staff] gave to St. Paul's Eye Clinic, which they arranged, was applauded," says Loyer. "The treating physician commended the DEEC on catching a few issues that could have – and would have – become serious." As part of her assessment, Loyer had optic nerve scan and visual field testing done onsite, and was also given a prescription for eyeglasses, which she received within 24 hours at a nearby optical store. Loyer's positive experience in accessing full-circle treatment solutions is exactly what Dr. Maberley envisioned when he helped set up the DEEC, with the support from the BC-CfE. At the original clinic at the VNHS, he sometimes saw patients in doorways and did vision testing in the hallway. Entering the new building via a grey door in the back alley, a visitor walks past the Vancouver Coastal Health Connections Clinic, turns right and down the hall to the eye clinic. The spacious DEEC waiting room has a children's play area and framed photos of street shots taken by Dr. Maberley in the surrounding neighbourhood. Clients are welcome anytime. Bookings are kept to a minimum, ensuring the clinic staff and ophthalmologists can take the time to understand their patients' needs. Since moving to the new space, the clinic has grown from one to three rooms and acquired state-of-the-art equipment (with the hope of adding equipment for refractive laser eye surgery). Patient volume has increased three to four times, says Dr. Maberley. "This is a fabulous space. Clients can get assessed, have their eyes imaged, get directed to the right subspecialist, and then they get the proper care with almost no barriers," says Dr. Maberley. The move has also attracted more volunteers. Currently around a dozen ophthalmologists and optometrists donate their time and funds coming to the clinic through the BC Medical Services Plan. This includes specialists for glaucoma, cornea, and retina; a pediatric ophthalmologist; and even a doctor who flies in monthly from Smithers, B.C., to help out. Dr. Maberley himself has a long history of health outreach, first in northern Canadian communities and then later in inner-city neighbourhoods in New York City. At Queen's University, he completed a Master's of Science in Community Health and Epidemiology after medical school at the University of British Columbia. When he was still in high school, he followed his father, also an ophthalmologist, on a trip abroad with Orbis International's Flying Eye Hospital. "My dad volunteered to assist those with vision loss in the developing world, and I always felt there was also a local need. While we see ourselves as being pretty well off here in Canada, we do have gaps – there is no question," he says. | Forecast Newsletter | Download | |||||||||||||||||||||||
| April, 2018 | BC-CfE Drug Treatment Program Monthly Report (January 2018) | Drug Treatment Program | DTP Status Report | Download | |||||||||||||||||||||||
| March, 2018 | Today, Panama cites TasP success in reducing HIV morbidity and mortality |
According to health officials, Panama's embrace of Treatment as Prevention® (TasP® ) since 2014 has resulted in quicker diagnosis, as well as accelerating the linkage of patients to antiretroviral therapy (ART) clinics. The country's HIV diagnoses curve has stabilized in recent years and officials expect it will decrease in the coming years. "We have achieved better adherence and there has been an increase in the percentage of patients with undetectable viral loads," says Dr. Aurelio Núñez Maitín, Head of the STI, HIV and Viral Hepatitis National Program in Panama. "The incorporation of the BC-CfE's TasP® strategy in Panama has permitted the decentralization of CD4 counts and pVL tests in the country and the incorporation of a new algorithm for diagnosing HIV. These helped facilitate the beginning of the 90-90-90 strategy in the country." In addition to widespread HIV testing and immediate access to highly active antiretroviral therapy (HAART) for people living with HIV, the Ministry of Health is initiating a program titled "RAPID". This will focus on initiating patients into treatment immediately after diagnosis and on decentralizing services for people living with HIV so that they can receive treatment from general physicians and family doctors. Panama is increasing support for vulnerable groups such as MSM (men who have sex with men), women and transgender populations to encourage treatment adherence. Panama, which has a population of 3.8 million, has an estimated 17,000 people living with HIV. Comparatively, there are approximately 12,000 people living with HIV in B.C., which has a population of 4.6 million. The BC-CfE and Panama's health authorities jointly developed research and HIV initiatives and created an HIV fellowship program allowing Panamanian HIV scientists to work with BC-CfE researchers and clinicians in Vancouver. During this time, the BC-CfE trained lab staff and students and provided science and support in the development and evaluation of Panama's TasP® strategy. The BC-CfE trained master's students and developed research on the cost-effectiveness of TasP® while also processing lab samples for HIV drug resistance. In order to further develop the partnership, Panamanian health officials are developing a business case to expand BC-CfE support. The objective is to establish a facility similar to the BC-CfE in Panama, with BC-CfE support in an advisory capacity. "Our most recent update from the Panama government shows that TasP® is working exactly as we hoped and expected, to bring down the existing morbidity and mortality rates in that country," says BC-CfE Assistant Director, Dr. Rolando Barrios. "Moving forward, existing TasP® infrastructure – and the investment made by the people of Panama - will also help the country grapple with HIV-related challenges as they deal with increased migration from neighboring countries." Barrios believes there is an opportunity for the BC-CfE to expand the partnership with Panama, especially in the area of the BC-CfE's phylogenetic "first-of-its-kind" system identifying HIV transmission outbreaks, or "clusters" (groups of recent, related, HIV infections). Adopting the BC-CfE mapping technology will allow Panama, especially during times of population growth, to proactively monitor and track HIV clusters to ensure people are getting the treatment they need while controlling the spread of HIV. Panama is also interested in the adoption of the BC-CfE's Targeted Disease Elimination™ (TDE™) approach that would help the country respond to infectious disease and other high burden diseases affecting the country. "In addition to developing the program going forward, Panama will also need to address the supply of higher quality HIV drugs," says Dr. Rolando Barrios. "And in that case, global support for Panama will be crucial. Any concerns with slowing down the epidemic are due to the rapid rate of migration being experienced by Panama due to instability in surrounding nations. But, despite these challenges, Panama is a great success story." The memorandum of understanding (MOU) signed in 2014 in the global fight against HIV/AIDS, made Panama the first country in Central America to embrace TasP®. The country joined China, France, and Brazil, among others in adopting the strategy as their national HIV/AIDS policy. TasP® has also been implemented by cities across the United States, including San Francisco, New York City, and Washington, D.C. | Epidemiology and Population Health, Laboratory | Treatment as Prevention® | Forecast Newsletter | Download | |||||||||||||||||||||
| March, 2018 | BC-CfE Drug Treatment Program Monthly Report (December 2017) | Drug Treatment Program | DTP Status Report | Download | |||||||||||||||||||||||
| March, 2018 | PrEP Baseline Assessment Tool | PrEP | PrEP Documents and Forms | Download | |||||||||||||||||||||||
| March, 2018 | BC-CfE Drug Treatment Program Monthly Report (November 2017) | Drug Treatment Program | DTP Status Report | Download | |||||||||||||||||||||||
| February, 2018 | Phylogenetics: The future of the fight against HIV/AIDS and other targeted diseases |
A revolutionary phylogenetic monitoring program developed at the BC Centre for Excellence in HIV/AIDS (BC-CfE) demonstrates how HIV is spreading across five provinces in Canada. This first-of-its-kind system identifies HIV transmission outbreaks, or "clusters" (groups of recent, related, HIV infections) in near real-time. "HIV does not stop at jurisdictional boundaries. Yet time and time again, we treat it like it does," says Dr. Jeff Joy, Research Scientist. "And while we can see the value of applying this system to HIV in Canada – the long-term impact of this type of phylogenetic monitoring could be significant with the rise of HIV drug resistance testing in other countries and in monitoring the spread of other infectious diseases." The HIV phylogenetic map spanning British Columbia, Alberta, Saskatchewan Ontario and Quebec and developed with the support of the Public Health Agency of Canada, tells the story of Canada's continuing battle with HIV. While most of the provinces contain large, localized HIV clusters, a full 55 clusters span across three or more provinces - including one cluster involving the five provinces. Researchers say the way HIV travels makes it clear the variation across the country in HIV treatment needs to be replaced by a consistent, coordinated national effort. "The federal government's embrace of the UN 90-90-90 Target, harm reduction, as well as progressive and inclusive attitudes towards the LGBTQ2 community will help move to eliminate HIV in Canada," says Joy. "We also need to ensure there is equitable access to treatment in hard to reach communities and equal access to antiretroviral treatment. Phylogenetics allows us to make a strong case for this." The potential application of this technology does not stop at HIV transmission. The phylogenetic technology being used by the BC-CfE has evolved from science to implementation to public health benefit, not just for British Columbia, but nationally. The program is designed to respond to a variety of challenges in the context of different epidemics for any virus or pathogen that evolves rapidly. Researchers plan to apply phylogenetics to examine the spread and containment of Hepatitis C nationally. "Canada has historically been a leader in the fight against HIV/AIDS. The BC-CfE pioneered HAART (highly active anti-retroviral therapy) as the most effective treatment and Treatment as Prevention (TasP) which is now the standard strategy to tackle HIV around the world," says Dr. Julio Montaner, BC-CfE Director. "This is the progression of that innovation – getting one step ahead of HIV. In addition, we can use lessons from one of the deadliest infectious diseases in the world to promote a Targeted Disease Elimination (TDE™) approach to tackle other high-burden diseases." "There is no need to stop inside our borders," says Joy. "There has been a positive reaction to this technology and the question we are asked most often is ‘how do we do this in other jurisdictions? In China or Australia?'" The system in Canada is unique to Canada, largely because the data systems in countries like the US are not as centralized, allowing them to look at Canadian results as a representation of what maybe happening in the US. The Canadian system will include every HIV sequence from nearly all the provinces and territories of Canada. "This is exciting. We have built a system that allows us to develop a unified, national response to HIV, examine how to coordinate a response to other infectious disease and use our resources more effectively," says Joy. "Going forward we can look at global epidemics, their evolution, migration and the impact of drug resistance. Phylogenetics offers endless possibilities to improve public health around the world and positively impact health care sustainability." | Treatment as Prevention® | Forecast Newsletter | Download | ||||||||||||||||||||||
| February, 2018 | HIV Monitoring Quarterly Reports, Fourth Quarter 2017 |
| STOP HIV/AIDS | ||||||||||||||||||||||||
| January, 2018 | BC aims to reduce new cases of HIV with expanded PrEP |
British Columbians, including men and transwomen who have sex with men, people who inject drugs, and people who have sex with individuals living with HIV, can now access free medication to protect against HIV. As of January 1st, the province of British Columbia is covering the cost of pre-exposure prophylaxis treatment (PrEP), recommended by the BC Centre for Excellence in HIV/AIDS (BC-CfE) as an effective method to prevent HIV in people at risk of infection. "The addition of PrEP to our Treatment as Prevention strategy will further accelerate the decline of new HIV infections in the province," said Dr. Julio Montaner, director, BC-CfE. "This move further demonstrates BC's continuing leadership in decreasing HIV and AIDS by addressing the specific healthcare needs of all British Columbians." The new program joins the existing, and newly expanded, PEP (post exposure prophylaxis) program. Developed and managed by the BC-CfE for the past twenty years, the PEP program has provided HIV prevention medication in instances of sexual assault and occupational exposure. With the support of the provincial government, the BC-CfE has expanded NPEP (non-occupational post-exposure prophylaxis) provincially. NPEP covers individuals who may have been exposed to HIV through consensual drug use or sexual encounters. "Our government is committed to helping fight the spread of HIV/AIDS and supporting people as they take action to protect themselves from this virus," said Adrian Dix, Minister of Health in a press release. "Making this medication free for people will prevent new HIV infections, remove barriers to care and services, and help people live longer and healthier lives." In August 2016, the Common Drug Review recommended PrEP coverage be expanded based on securing a lower price for the generic version of the drug Truvada. "By reducing the cost of PrEP, both for treatment and prevention, we now have an opportunity to expand our abilities to effectively decrease new HIV infections in the province," said Dr. Montaner. He says identifying groups who are most at-risk for being infected with HIV will be a key part of the success of the medication. "The team at the BC-CfE has been working hard to make PrEP accessible and economical. The good news is we have a more complete range of tools at our disposal to pursue the elimination of HIV in BC based on our Treatment as Prevention model," says Dr. Mark Hull. "We are now working on educating physicians and British Columbians about access and availability." The BC-CfE website features detailed prescribing practices, enrollment information, education and training. Updated guidelines, course information and frequently asked questions will be addressed through online channels and social media. Ongoing online education courses, including webinars, will offer updates regarding all BC-CfE programs including PEP, NPEP and PrEP. | PrEP, Treatment as Prevention® | Forecast Newsletter | Download | ||||||||||||||||||||||
| January, 2018 | Raltegravir 600mg HD tablet (Isentress™ HD) | Formulary Addition | Dear Doctor Letter | Download | |||||||||||||||||||||||
| December, 2017 | BC HIV/AIDS and Addictions Health Care Resources | The British Columbia Centre for Excellence in HIV/AIDS (BC-CfE) does not endorse any resource listed in the below document. The pdf provides links to other Internet sites for informational purposes and the convenience of its users. When users select a link to an external Web site, they are subject to the privacy and security policies of the owners/sponsors of the external site. Acknowledgements: We acknowledge that the information contained in this resource package was compiled from multiple existing online sources including the British Columbia Centre on Substance Use (BCCSU), BC Housing, Greater Vancouver Food Bank, Food Bank BC, Lookout Society, Opiate addiction and Treatment Resource and Positive Living Society of British Columbia. | Download | ||||||||||||||||||||||||
| December, 2017 | BC-CfE Drug Treatment Program Monthly Report (October 2017) | Drug Treatment Program | DTP Status Report | Download | |||||||||||||||||||||||
| December, 2017 | BC-CfE's decades-long HIV/AIDS leadership takes centre stage in BC and Ottawa on World AIDS Day |
BC leads the way nationally In 1996, BC was the epicenter of the HIV/AIDS crisis in Canada, with the province diagnosing up to 800 people a year at the height of the crisis. Being in the ‘eye of the storm' forced the province and researchers to address the disease with an innovative spirit and ground-breaking treatment - setting the standard nationally and around the world. New research from the BC Centre for Excellence in HIV/AIDS (BC-CfE) shows by 2020 90% of people living with HIV in BC will be diagnosed, 91% of those diagnosed will be on treatment, and 90% on effective treatment and unable to pass on HIV (virologically suppressed), showing BC is leading the way in Canada. However, the research also found disparities: females are 30% less likely to be on HIV treatment compared to men; people with a history of injection drug use are 49% less likely to be on treatment than other groups; and people ages 18 to 29 are 35% less likely to be on treatment. BC-CfE marks World AIDS Day in Ottawa BC-CfE Director Dr. Julio Montaner attended a flag-raising event at World AIDS Day in Ottawa where he spoke about the importance of education and patient-centered services in fighting HIV/AIDS. Montaner appeared alongside UNAIDS Executive Director Michel Sidibe for the presentation of the UNAIDS report Blind Spot, highlighting the importance of reaching out to men and boys to get tested for HIV and access and adhere to treatment. Dr. Montaner participated in panel discussions with Minister of Health, Hon. Ginette Petitpas-Taylor. In a one-on-one meeting with the minister, Dr. Montaner discussed Canada's progress in HIV prevention, the revolutionary Canada-wide phylogenetics program developed by BC-CfE to pinpoint clusters of HIV infection nationally and how Treatment as Prevention® (TasP®) can be further applied to Targeted Disease Elimination (TDE) in the realm of infectious and non-infectious diseases. Montaner discussed Diabetes Canada's recent adoption of the TasP®-based 90-90-90 Target as the first example of applying TasP® to a non-infectious disease. A path to HIV decriminalization Justice Minister, Judy Wilson-Raybould announced Canada-wide guidelines for the prosecution of HIV-related cases in the report, Criminal Justice System's Response to Non-Disclosure of HIV. While the report addresses the broad over-criminalization of HIV in Canada, the BC-CfE believes the guidelines could go further to prevent HIV criminalization across the country. "People forget that the universal access to HIV medication enjoyed by people in British Columbia is not a reality for all Canadians," says Dr. Julio Montaner. "While we welcome the guidelines, we need a clear, national and consistent response to de-criminalizing HIV. Simply declaring it a public health issue, and not a criminal issue, I fear, doesn't not go far enough." The Justice Canada report states criminal law should not be applied to people living with HIV who are on treatment, not on treatment but use condoms, or engage only in oral sex (unless other risk factors are present and the person living with HIV is aware of those risks) because the possibility of transmission "is not met" in these circumstances. However, as we have seen in the case of Ontario, provinces can selectively apply the guidelines. Ontario has announced the province will refrain from prosecuting people who have a suppressed viral load for six months – leaving all others who manage the risk of transmission open to criminal prosecution. "The still-present fear of criminalization under these unevenly applied guidelines may keep people from getting tested and treated," says Dr. Montaner. "In the case of condom breakage, for example, disclosure of positive HIV status immediately after exposure allows HIV-negative sexual partners to access post-exposure prophylaxis to significantly reduce the risk of transmission. People need to feel comfortable coming forward about their status without the fear of criminalization. This is how you keep Canadians HIV-free." | Treatment as Prevention® | Forecast Newsletter | Download | ||||||||||||||||||||||
| December, 2017 | BC-CfE Drug Treatment Program Monthly Report (September 2017) | Drug Treatment Program | DTP Status Report | Download | |||||||||||||||||||||||
| November, 2017 | Cancer, cardiovascular disease, new PEP guidelines and more: The Fall ARV Update |
PEP: Start early, follow up and start a conversation Dr. Marianne Harris, Clinical Research Advisor with the BC Centre for Excellence in HIV/AIDS (BC-CfE), provided an overview of the new BC-CfE PEP (post-exposure prophylaxis) guidelines. Dr. Harris emphasized the safety and tolerability of the PEP regimen will be improved with the use of raltegravir and due to improved lab technology, the final HIV test can be done 3 months (instead of 12) after the event. PEP will be available to everyone who has had a significant HIV exposure, regardless of the circumstances. For many clients, the challenges to follow-up can be exacerbated by shame and anxiety around accessing PEP, according to registered nurse Liz Kirkpatrick. In applying PEP guidelines to clinical practice, Fitzpatrick encouraged clinicians to develop a rapport with clients to understand their individual circumstances and the role played by social and behavioral determinants of health. Kirkpatrick recommends nurturing an inclusive, respectful discussion about healthy sex and risk reduction into conversations about PEP treatment. Risk of cancer higher and occurring earlier in people with HIV: Salters, Ramji and Leung Dr. Janice Leung, a Respirologist at St. Paul's Hospital, showed lung cancer appears earlier and more aggressively in people with HIV and is often deadlier in this group compared to the general population. People with HIV are at increased risk of not receiving stage appropriate treatment, "falling through the cracks", and suffering higher mortality from lung cancer. The research shows 40-84% of HIV patients are current smokers compared to 20% in the HIV-negative population. Dr. Kate Salters, Post-Doctoral Fellow with the BC-CfE, addressed the HIV/ARV Update with preliminary data from the COAST (Comparative Outcomes And Service Utilization Trends) study suggesting cancer incidence is twice as high in people with HIV, compared to the general population, but varies significantly based on the type of cancer. The largest disparities in cancer rates occur earlier in life - before age 50 - and for infectious-related cancers. Although unclear, there is some promising evidence that early initiation of cART (combination antiretroviral therapy) with higher CD4 cell counts may reduce the risk of infectious-related cancers, such as HPV-related cancers. As the sixth most common cancer in people with HIV, says Dr. Alnoor Ramji, Clinical Associate Professor at the University of British Columbia, hepatocellular carcinoma (HCC) results in 700,000 deaths a year worldwide. HIV is not an independent cause of HCC, but there is more incidence in the HIV positive population related to Hepatitis C and Hepatitis B co-infections. Active screening of HCC in persons with HBV or HCV co-infection, particularly in baby boomers, is strongly encouraged. Cardiovascular risk underestimated in people with HIV Data collected over the last two decades shows the chances of having heart attack goes up by 50% for people with HIV - this is above the traditional risk factors. Dr. Greg Bondy, a specialist at St. Paul's Hospital, revealed virtually all men with HIV over the age of 35 and women over 50 will be at moderate risk of cardiovascular disease. However, there is some promising news related to a large HIV trial with Evolocumab. It shows the drug is effective in people with HIV, driving down risk from cardiovascular disease 60-70%. It is safe, free of side effects; however, access is limited due to cost. Opioid treatment for people with HIV Chronic opioid therapy for chronic pain and prescription opioid use disorder appears to be more common in people with HIV who are much more likely to be prescribed opioids for pain compared to uninfected patients. One in five people with HIV are prescribed chronic opioid therapy for pain. Dr. Jeffrey Samet, Chief, Section of General Internal Medicine, Boston Medical Center, discussed practice guidelines for managing pain using inter-disciplinary teams for complex chronic pain, considering non-opioid options and prescribing smaller doses with routine monitoring. Most importantly, Dr. Samet says, "judge the treatment, not the patient". Most people living with HIV recognize there is a danger in becoming addicted to opioids. Generic ARVs in BC: A work in progress The potential economic impact of generic antiretrovirals in BC continues to be a work in progress, according to Dr. Viviane Lima, BC-CfE Research Scientist & Senior Statistician. However, the results so far suggest generic ARVs may have a beneficial and substantial impact on the fiscal needs of the ARV program in BC. Dr. Lima encouraged caution, saying the projections and estimates presented are only intended to give an overall sense of the anticipated cost-savings trends over time. While the preliminary, short-term projections are encouraging, Dr. Lima recommends monitoring the trends in the use of generic ARVs in the long-term to get a clearer picture of their economic impact in BC. | Treatment as Prevention® | Forecast Newsletter | Download | ||||||||||||||||||||||
| November, 2017 | HIV Monitoring Quarterly Reports, Third Quarter 2017 |
| STOP HIV/AIDS | ||||||||||||||||||||||||
| November, 2017 | BC-CfE Drug Treatment Program Monthly Report (August 2017) | Drug Treatment Program | DTP Status Report | Download | |||||||||||||||||||||||
| November, 2017 | BC-CfE Pharmacovigilance 2016 Annual Report | Pharmacovigilance Initiative, Quality and Safety | Download | ||||||||||||||||||||||||
| November, 2017 | Treatment as Prevention model (TasP) and 90-90-90 Target adopted by Diabetes Canada |
Diabetes Canada announced it is adapting the made-in-BC Treatment as Prevention (TasP) strategy to diabetes to make over 6 million Canadians living with pre-diabetes, and diabetes, aware of their status. The epidemic of diabetes and prediabetes affects over 11 million Canadians and can cause blindness, kidney failure, heart attack, stroke and lower limb amputation. Diabetes prevalence has more than doubled since 2000 and estimated to increase by 40 per cent by 2025. "Canada needs a bold, new strategy to slow the pace at which the diabetes epidemic is growing, and we believe this approach can be a cornerstone of that strategy," says Russell Williams, vice president of Government Relations and Public Policy at Diabetes Canada. Adapting the TasP strategy, and the related 90-90-90 Target, to diabetes will encourage early diagnosis, treatment, and engagement into care to prevent diabetes-related complications that cost the Canadian healthcare system billions of dollars a year. Studies show that as much as 60 per cent of people with prediabetes who make modest lifestyle changes can delay or prevent developing diabetes. This is the first time the made-in-BC TasP strategy, and the related global 90-90-90 Target for the control of HIV/AIDS, will be applied to a non-infectious disease. "We have always believed TasP can be applied to other high burden diseases aside from HIV/AIDS including contagious diseases - whether infectious as in viral hepatitis, or socially contagious as in type 2 diabetes," says Dr. Montaner. "Expanding TasP® beyond HIV/AIDS will ease the burden on our healthcare system and substantially contribute to enhanced healthcare sustainability." Diabetes Canada convened a multi-stakeholder workshop in September with Dr. Montaner providing the keynote address, to discuss the benefits of adopting a 90-90-90 Target for diabetes in Canada and the reaction was overwhelmingly positive. "We were very pleased that the 48 representatives of 30 different stakeholder organizations – people living with diabetes, health-care providers, policy makers and more – all agreed that it's worth investing further in a 90-90-90 Target for Canada," says Mr. Williams. "Not only will it impact the health of Canadians and decrease the diabetes-related burden on our health-care system, but it will also contribute to Canada resuming its place as a global leader in the treatment of diabetes." Developed by Dr. Julio Montaner, the 90-90-90 Target proposes to have at least 90 per cent of all people living with HIV diagnosed, at least 90 per cent of them on antiretroviral therapy and at least 90 per cent of them virologically suppressed by 2020. Achieving the 90-90-90 Target by 2020 would lead to a 90 per cent reduction in HIV/AIDS morbidity and mortality and a 90 per cent decrease in new HIV infections by 2030. "We plan to implement the 90-90-90 Target to diabetes by encouraging 90 per cent of the 6 million Canadians with prediabetes, and the 1.5 million Canadians who are currently unaware that they are living with diabetes, to learn their status through expanded screening," says Williams. "Our goal is to work toward changing the approach to treating and managing diabetes before it impacts Canadians' quality of life." 90 per cent of those diagnosed with prediabetes and diabetes (along with the 3.5 million Canadians who have already been diagnosed with diabetes) would receive treatment, lifestyle counseling or care to prevent or manage the disease. 90 per cent of those receiving treatment would be seeing improved health indicators, such as lower three-month average blood glucose, with consequent improvements in blood pressure and lipids. Diabetes Canada will present a report on the progress against the 90-90-90 Target in Canada by 2021 to coincide with the 100th anniversary of the discovery of insulin by Canadians. | Treatment as Prevention® | Forecast Newsletter | Download | ||||||||||||||||||||||
| October, 2017 | BC-CfE Drug Treatment Program Monthly Report (July 2017) | Drug Treatment Program | DTP Status Report | Download | |||||||||||||||||||||||
| October, 2017 | Patterns of Online and Offline Connectedness among Gay, Bisexual and Other Men who have Sex with Men | How do patterns of online and offline connectedness relate to beliefs and behaviours around HIV prevention among gay and bi men in Metro Vancouver? | Epidemiology and Population Health, Momentum | Research Summary | Download | ||||||||||||||||||||||
| September, 2017 | Innovation and experience at the heart of BC-CfE addictions pilot project |
It's the first program of its kind in Canada and could mark a radical change in the way treatment is offered to people living with opioid use disorder. The BC Centre for Excellence in HIV/AIDS (BC-CfE) and Vancouver Coastal Health (VCH) marked the launch of the BOOST (Best-practices in Oral Opioid agoniSt Therapy) Collaborative by bringing together twenty teams from across VCH to improve access to - and retention in - suboxone and methadone treatment. Based on the highly effective, made in BC HIV/AIDS Treatment as Prevention (TasP) model, BOOST will use the methodology behind STOP (Seek and Treat for Optimal Prevention) HIV/AIDS – the program that successfully sought out untreated HIV positive people and provided them with lifesaving anti-retroviral therapy. "There are many parallels between the HIV/AIDS epidemic and the overdose crisis we are experiencing now," says Dr. Rolando Barrios, assistant director at the BC-CfE. "Keep in mind, however, missing a dose of HIV medication could make you sick but missing a dose of suboxone can have immediate life or death consequences. The BOOST Collaborative is designed to help front-line staff ensure people get their treatment daily and stay in treatment long-term." The strategy known as TasP is being deployed as a key tool to promote Targeted Disease Elimination and healthcare sustainability to therapeutic areas beyond HIV/AIDS, including addiction and viral hepatitis. The program will expand the BC-CfE's demonstrated success in the control of HIV/AIDS, centered on the optimization of therapeutic opportunities to decrease morbidity, mortality and new HIV cases. "The work we did, we did together, during the HIV/AIDS era which enhanced access to life saving services for our most marginalized patients - stopping premature deaths and transmissions," Dr. Julio Montaner, director of the BC-CfE told the BOOST Collaborative. "We had effective therapy in the form of anti-retroviral medication, so we changed our approach dramatically - from a passive approach to engaging with our clients to facilitate their access to services. We realized this was good for our clients, public health and promoting healthcare sustainability." For families, friends and harm reduction advocates, a new approach aimed at saving lives is welcome news. "As parents and family members we are always on a never-ending search for treatment for our loved ones and the current opioid crisis has us in a constant state of fear and anxiety," Frances Kenny, Founder of PARENTS FOREVER told the doctors, nurse and front-line workers with the Collaborative. "We are excited to welcome a pilot project that seeks to close any gaps in the system and will attempt to proactively reach out to people with OUD, engage them in care and attempt to keep them in care." After sharing learnings on how to improve opioid agonist therapy with system change, Dr. Dennis McCarty, Division Head, Health Services Research, Oregon Health and Science University spoke about how BOOST could set the standard internationally for delivering opioid agonist treatment around the world. "Vancouver broadly - and British Columbia - is setting the stage at a higher level of excellence and that's something to aspire to," says McCarty. "Vancouver has a high penetration of fentanyl - and fentanyl is a much more dangerous opioid than heroin - but you also have a more organized system of care because it is a provincial health system. The province benefits from reductions in health care expenses, they benefit from reductions in mortality and morbidity and a reduction in stress on the criminal justice system." The first set of results from the BOOST Collaborative will be available in the winter of 2017, with the entire project set to conclude in July 2018. | STOP HIV/AIDS | Forecast Newsletter | Download | ||||||||||||||||||||||
| September, 2017 | BC-CfE Drug Treatment Program Monthly Report (June 2017) | Drug Treatment Program | DTP Status Report | Download | |||||||||||||||||||||||
| August, 2017 | HIV Monitoring Quarterly Reports, Second Quarter 2017 |
| STOP HIV/AIDS | ||||||||||||||||||||||||
| August, 2017 | Increasing HIV Treatment Optimism but No Changes in HIV Risk Behaviour among Men who have Sex with Men in Vancouver, Canada | Has increased optimism in the effectiveness of HIV treatment resulted in increased risky sex among men who have sex with men in Metro Vancouver? | Epidemiology and Population Health, Momentum | Research Summary | Download | ||||||||||||||||||||||
| August, 2017 | BC-CfE Drug Treatment Program Monthly Report (May 2017) | Drug Treatment Program | DTP Status Report | Download | |||||||||||||||||||||||
| July, 2017 | Elvitegravir-cobicistat-emtricitabine-tenofovir alafenamide (Genvoya™) | Formulary Addition and Criteria | Dear Doctor Letter | Download | |||||||||||||||||||||||
| July, 2017 | BC-CfE 2017 Spring HIV/Antiretroviral Update: Overdose epidemic will worsen, continuing hope for expanded HCV treatment and coverage |
The 2017 Spring HIV/Antiretroviral update featured a diverse roster of leading health professionals to discuss the latest numbers from the front lines of the opioid epidemic, advances in Hepatitis C screening and progress in meeting 90-90-90 HIV/AIDS targets around the world. ADDICTIONDr. Patricia Daly characterized the current state of the opioid crisis in Vancouver as one of the most challenging public health emergencies of her career. Vancouver is on track to exceed the number of opioid related deaths in 2016, with most of this year's fatalities occurring as a direct result of fentanyl or carfentanil contamination. Over 80 percent of people presenting with overdose are male, and while status First Nations people form only 2 percent of the population, 18 percent of overdoses seen in Vancouver's emergency departments from 2012-2016 were among this group. While the crisis continues and harm reduction remains a priority, Dr. Daly highlighted the importance of early intervention, reaching out to Indigenous communities, supporting early childhood development, and addressing the needs of vulnerable youth. Dr. Nadia Fairbairn followed Dr. Daly with a warning that Vancouver's current opioid epidemic resembles another public health crisis from Vancouver's past. "The opioid crisis has been rivalled in modern history only by the peak of the AIDS epidemic in the 1990's," she said. "Although these epidemics differ in nature, the large scale, highly coordinated response to HIV and AIDS that had such a huge impact on changing its course, may be instructive today in combating the opioid epidemic." Dr. Fairbairn discussed loss of tolerance to opioids through detox, incarceration and hospitalization and the resulting increased risk of overdose post-release and increased risk of HIV morbidity and mortality. Fairbairn spoke to an alternative - initiating a "slow taper" using methadone or buprenorphine/nalaxone in an outpatient setting - combined with counseling about overdose risk and take-home naloxone training. SYPHILISDr. Peter Phillips began his syphilis update with the question - is the epidemic under control? The short answer is no. While syphilis rates improved around 2010, they increased fivefold by 2015 in BC, and are projected to further increase in 2016. Over 86 percent of men diagnosed with syphilis were men who have sex with men (MSM). Forty percent of newly diagnosed cases were also among HIV positive populations. Phillips suggested new paradigms in treatment and treatment options as well as information about the impact of having HIV on treatment options – need to be explored. HEPATITIS CDr. Lianping Ti shared good news regarding Hepatitis C (HCV) including a reduction in price for life saving drugs for Canadians, the introduction of safer and more tolerable medications, the development of new guidelines around the testing for HCV and the potential for universal coverage under BC's Pharmacare program in 2018-19 for those living with the virus. However, there continue to be challenges around testing for HCV. Only 44 percent of people living with HCV are aware of their status. While mortality related to tuberculosis, HIV and malaria is on the decline, HCV-related mortality continues to rise. Despite a large body of evidence and clinical guidelines to support one-time screening for HCV among baby boomers, the Canadian Task Force on Preventive Health Care recommended against screening for this population stating it found "no evidence on the effectiveness of screening HCV in the asymptomatic adult population". Following Dr. Ti's presentation, Dr. Alnoor Ramji discussed the importance of providing timely HCV treatment to ensure improvement in all-cause mortality and decreases in liver related mortality, liver failure and liver cancer. Ramji says HCV elimination is a reality, provided physicians actively check patients for fibrosis and offer treatment regimens that are simple and effective in 90-95 percent of patients. HIVIn Canada, 70 percent women living with HIV are between the reproductive ages of 15 and 39. Dr. Melanie Murray spoke about birth control options for HIV positive women, considerations for conception, preparing for pregnancy and pregnancy outcomes in HIV positive women. She pointed out that almost 50 percent of pregnancies among women with HIV are not planned, and that healthcare providers should consider the possibility of pregnancy throughout the reproductive years. Murray says planning for pregnancy must consider pre-conception health (undetectable viral load and adherence to therapy as well as management of co-morbidities), possibility of transmission between partners during conception, transmission from mother to infant and management of infertility issues. Dr. Reuben Granich discussed the current state of global HIV care continua, global HIV policy and the worldwide progress on the 90-90-90 target. There are 2 million new HIV infections every year, 37 million people with HIV worldwide and 1.1 million deaths. Roughly 60 percent of people know their status, 50 percent are on treatment and $20 billion is being spent on HIV globally per year. One of the biggest challenges to "ending AIDS" is the global inconsistency in adopting the policy of testing and offering immediate treatment, but countries are rapidly moving towards this strategy. Dr. Granich says the end of AIDS is feasible, but for the 90-90-90 target to be truly successful, the goal is to engage and keep 37 million people on life-long treatment until a vaccine and/or cure is available. Dr. Réka Gustafson delivered Dr. Rolando Barrios' presentation discussing the gaps in the HIV continuum of care in British Columbia. Gustafson highlighted the significant drop that occurs between linked to care and retained in care among people over 50 and under 30. An area identified for further study was the low percentage of viral suppressions among women. The numbers show a major drop between diagnosis and linkage to care for women under 30. Dr. Ronald Werb spoke about the effects of HIV on renal tissues, the immune response to the virus and the reaction within the kidneys as well as the impact of HIV treatment on renal function. Dr. Greg Bondy discussed the management of obesity and metabolic disorders among people with HIV. Most patients who see body fat redistribution and increased obesity may be seeing these changes due to a higher baseline viral load, anti-retroviral therapy, chronic inflammation, body type, or hormones. Dr. Robin Hsiung presented an update on HIV-associated neurocognitive disorders (HAND) and the range of disorders that fall under that category - from HIV associated dementia, mild neurocognitive disorders to asymptomatic neuro-cognitive impairment. Hsiung also discussed the current issues related to the diagnosis and management of HAND. | Treatment as Prevention® | Forecast Newsletter | Download | ||||||||||||||||||||||
| June, 2017 | BC-CfE Drug Treatment Program Monthly Report (April 2017) | Drug Treatment Program | DTP Status Report | Download | |||||||||||||||||||||||
| June, 2017 | Dr. Julio Montaner accepts inaugural Gold Leaf Prize for Impact on behalf of the BC Centre for Excellence in HIV/AIDS |
In recognition of the BC Centre for Excellence in HIV/AIDS' (BC-CfE) 25 years of leadership in the battle against HIV/AIDS Dr. Julio Montaner was in Ottawa on May 16th, 2017 to accept the CIHR Gold Leaf Prize for Impact on behalf of the staff of the BC-CfE. The CIHR Gold Leaf Prize for Impact is awarded to an individual or team that demonstrates proven impact on health outcomes, practices, policies, and on the health system. The award acknowledges the role the BC-CfE has played for over 30 years developing effective treatment and providing care for those living with HIV/AIDS, educating health professionals worldwide, and promoting evidence-based policy to protect people and populations from the virus. "I was incredibly proud to accept this award on behalf of the BC Centre for Excellence in HIV/AIDS," said Dr. Julio Montaner, Director, BC-CfE. "Throughout its history, the BC-CfE has been a leader in tackling one of the world's deadliest diseases with an innovative and compassionate approach. The Gold Leaf Prize is recognition of the ground-breaking work of the scientists, doctors, researchers, health care providers and community members. All who tackled the complex challenges presented by the HIV/AIDS virus in the early days, developed innovative treatments and advocated for those most impacted by the disease." Since 1981, the year HIV/AIDS first appeared in North America, an estimated 39 million people have died of AIDS worldwide. In British Columbia in the early 1990s, one person was dying of AIDS almost every day. Since then, as a result of the innovation by BC-CfE and the introduction of life-saving drug therapies, HIV has become a chronic and manageable disease for those who can access highly active antiretroviral treatment (HAART). In the early days of the HIV/AIDS crisis, innovation drove Dr. Montaner and the Centre's early successes in transforming the lethal Pneumocystis pneumonia (PCP), the most frequent cause of death among HIV-infected individuals, into a treatable and preventable condition. Over the following decade, the Centre's work on the development of new drugs and therapies lead to Dr. Montaner's landmark study establishing the ability of NNRTI-based triple drug therapy (later known as HAART) to suppress HIV replication and put the disease into full and lasting remission. The BC-CfE continued to lead advancements in the area of HIV/AIDS, with Dr. Montaner spearheading the single most successful example of knowledge translation in the history of medicine. Montaner used the Vancouver Conference to disseminate the emerging HAART strategy, ensuring it was accepted as the new standard of care by the end of the conference - 12 to 18 months before the research was published in peer-reviewed journals. Providing full and early access to crucial drug treatments to all, including marginalized communities, and ensuring universal coverage is the concept behind Treatment as Prevention (TasP), an approach pioneered by Dr. Julio Montaner. Based on its success in improving quality of life and longevity of HIV/AIDS patients, while reducing the spread of illness, TasP has been adopted by jurisdictions including Brazil, China, France, Panama, Spain, major US cities, and the state of Queensland in Australia. In 2015, a widely covered US National Institutes of Health (NIH) clinical study based in 35 countries, confirmed what the BC-CfE had been advocating for many years: early treatment is best to improve health outcomes and reduce transmission. Since 1992, the BC-CfE has provided evidence to support policies and programs that improve the health and welfare of populations most vulnerable to HIV and other related diseases. From leading the development of new treatments for HIV/AIDS to pioneering the advancement of the TasP model, the BC-CfE has grown to include 375 staff and a research laboratory, drug treatment program, epidemiology and population health program, the Urban Health Research Initiative and the Gender and Sexual Health Initiative. | Treatment as Prevention® | Forecast Newsletter | Download | ||||||||||||||||||||||
| June, 2017 | SAFETY UPDATE: Antiretroviral drug interactions with non-prescription medications | June 2017 - Drug interactions between antiretroviral drugs and other medications can result in loss of therapeutic efficacy or drug toxicity. Selected proton pump inhibitors and inhaled corticosteroids recently became available as non-prescription products in BC. These, and other non-prescription medications, can have clinically important interactions with certain antiretroviral drugs. This bulletin summarizes clinically important antiretroviral drug interactions with non-prescription drugs. | Pharmacovigilance Initiative, Quality and Safety | HIV Clinical Care | Download | ||||||||||||||||||||||
| May, 2017 | BC-CfE Drug Treatment Program Monthly Report (March 2017) | Drug Treatment Program | DTP Status Report | Download | |||||||||||||||||||||||
| May, 2017 | HIV Monitoring Quarterly Reports, First Quarter 2017 |
| STOP HIV/AIDS | ||||||||||||||||||||||||
| May, 2017 | BC-CfE Drug Treatment Program Monthly Report (February 2017) | Drug Treatment Program | DTP Status Report | Download | |||||||||||||||||||||||
| May, 2017 | BC-CfE Drug Treatment Program Monthly Report (January 2017) | Drug Treatment Program | DTP Status Report | Download | |||||||||||||||||||||||
| March, 2017 | BC-CfE welcomes Prime Minister Trudeau and members of cabinet to its Hope to Health Research Clinic |
Welcoming a new government that embraces evidence-based science has been a breath of fresh air for researchers across the country after a decade of silence from the Canadian government. This is in stark contrast to the previous Conservative government who fought Insite all the way to the Supreme Court of Canada and, subsequently, passed Bill C-2, which created substantial barriers to the establishment of safe consumption sites. The BC Centre for Excellence in HIV/AIDS (BC-CfE) is deeply appreciative of the support shown for our research in HIV, viral hepatitis and addiction work, part of the government's commitment to improving the health of Canadians. The BC-CfE had the pleasure to recently welcome Prime Minister Justin Trudeau, accompanied by Defense Minister Harjit Sajjan, to 625 Powell Street, its newly expanded Hope to Health Research Clinic. The BC-CfE hosted a roundtable discussion with the Prime Minister, first responders and community partners on the overdose crisis. The Hope to Health Research Clinic, located on the Downtown Eastside, is a BC-CfE research clinic which supports research to adapt, evaluate and expand Treatment as Prevention (TasP) to other contagious diseases. Under the leadership of Dr. Julio Montaner, BC-CfE Director, in the beginning, the clinic will focus on three pillars: HIV, addiction and viral hepatitis. The roundtable meeting was informative and moving as attendees spoke passionately about the overwhelming toll the overdose crisis has had on communities in B.C. To date, B.C. is the only province to declare a public health emergency after experiencing a surge in drug-related overdoses and deaths. Prime Minister Trudeau announced the federal government will provide $65-million over five years to respond to Canada's opioid crisis, with $10-million earmarked for B.C. Health Minister Jane Philpott's visit to Vancouver's Downtown Eastside last January 2016 during the provincial and territorial ministers meeting, where Dr. Montaner was invited to speak, was yet another sign of the present government's changing attitudes. Minister Philpott has returned for subsequent visits where she has met with Dr. Montaner, Irene Day, BC-CfE Operations Director, and Dr. Evan Wood, Director of the BC Centre on Substance Use, part of the BC-CfE, for a tour of the Hope to Health Research Clinic and an update on the BC-CfE's ground breaking research. Having worked as a family doctor for over 30 years, both in Canada and sub-Saharan Africa, Minister Philpott has not shied away from expressing her commitment to ending the HIV epidemic. The Health Minister and the Canadian Government have both officially endorsed the Joint United Nations Programme on HIV/AIDS (UNAIDS) global targets for HIV, including the 90-90-90 Target. The global Treatment Target calls for 90% of people living with HIV to know their status, 90% of people diagnosed with HIV to be in treatment, and 90% of people in treatment to have undetectable viral loads. The December 1, 2016, World AIDS Day statement by Prime Minister Trudeau reaffirmed the government's commitment to eliminating HIV. The statements closes by saying, "The fight against HIV/AIDS is a winnable one. I encourage all Canadians to support efforts to raise awareness about HIV/AIDS prevention through the UN-led #HIVPrevention campaign. By working together with researchers, activists, civil society, other countries, and the courageous people living with HIV/AIDS around the world, we can bring this global epidemic to an end." On the heels of Minister Philpott's visit, Dr. Montaner, and colleagues were honoured to welcome Minister of Justice and Attorney General of Canada, Jody Wilson-Raybould for a discussion and tour of the Hope to Health Research Clinic. Minister Wilson-Raybould acknowledged the problem of the over-criminalization of HIV non-disclosure in the criminal justice system. Dr. Kate Shannon, Director of BC-CfE's Gender and Sexual Health Initiative, also discussed with the Minister how HIV non-disclosure disproportionately affects women in the criminal justice system. Minister Wilson-Raybould was supportive of working with the BC-CfE on these issues. An important consensus statement signed by Dr. Montaner and 75 other prominent Canadian medical experts reflects the need for the criminal justice system to adapt to better reflect the current scientific evidence on HIV transmission. The BC-CfE celebrates the federal government's renewed commitment to support HIV and AIDS domestically and internationally, and we look forward to working together. | Treatment as Prevention® | Forecast Newsletter | Download | ||||||||||||||||||||||
| March, 2017 | Integrated HIV Care and Service Engagement among People Living with HIV who Use Drugs in a Setting with a Community-Wide Treatment as Prevention Initiative | It is well known that social and structural inequities, such as poverty and homelessness, can create barriers to routine HIV care among people living with HIV (PLHIV) who use drugs. Such barriers can contribute to poor HIV-related health outcomes among PLHIV who use drugs and undermine HIV treatment and prevention strategies. In British Columbia, treatment is offered universally upon diagnosis with HIV, as part of province-wide Treatment as Prevention (TasP) strategy. Citation: Collins, A., Parashar, S., Hogg, R., Fernando, S., Worthington, C., McDougall, P., Baltzer Turje, R., & McNeil, R. (2017). Integrated HIV care and service engagement among people living with HIV who use drugs in a setting with a community-wide treatment as prevention initiative: a qualitative study in Vancouver, Canada. Journal of the International AIDS Society, 20(1). | Dr Peter Study, Epidemiology and Population Health | Research Summary | Download | ||||||||||||||||||||||
| March, 2017 | Meaningful Engagement of People Living with HIV Who Use Drugs | This research is part of the Dr. Peter Study, a project co-led by the BC Centre for Excellence in HIV/AIDS (BC-CfE) and the Dr. Peter AIDS Foundation (DPAF). The Dr. Peter Study evaluates the effectiveness of the Dr. Peter Centre (DPC), an HIV day health program and residence facility in Vancouver, Canada funded by the DPAF. The paper described here aims to describe the PRA hiring process used for the Dr. Peter Study, in order to meet one of the study's goals of adding to the literature on engaging community members and affected populations in research. Citation: Closson, K., et al. "Meaningful engagement of people living with HIV who use drugs: methodology for the design of a Peer Research Associate (PRA) hiring model." Harm Reduction Journal 13.1 (2016): 26. | Dr Peter Study, Epidemiology and Population Health | Research Summary | Download | ||||||||||||||||||||||
| March, 2017 | “We're giving you something so we get something in return” | While there are concerns of increasing vulnerability and undue risk taking with compensation, there is a need to explore the impact of different types of compensation on vulnerable populations' voluntary consent and how it shapes research-related interactions. By exploring the impact of compensation on study participants, the researchers hope to inform the ethical framework around compensation policy. This study draws on five focus groups conducted with 25 people living with HIV who use drugs and are clients at the Dr. Peter Centre, a community based HIV care facility in Vancouver, Canada. It explores the ethics surrounding perceptions of research compensation practices by research participants. Citation: Collins, Alexandra B., et al. "“We're giving you something so we get something in return”: Perspectives on research participation and compensation among people living with HIV who use drugs." International Journal of Drug Policy 39 (2017): 92-98. | Dr Peter Study, Epidemiology and Population Health | Research Summary | Download | ||||||||||||||||||||||
| March, 2017 | Changes in Mortality Rates and Causes of Death in a Population-Based Cohort of Persons Living with and Without HIV from 1996 to 2012 | In this study, we aimed to characterize and compare changes over time (from 1996 to 2012) in mortality rates and causes of death among persons living with and without HIV in British Columbia. Citation: Eyawo O, Franco-Villalobos C, Hull MW, Nohpal A, Samji H, Sereda P, Lima VD, Shoveller J, Moore D, Montaner JS, Hogg RS; Comparative Outcomes And Service Utilization Trends (COAST) study. Changes in mortality rates and causes of death in a population-based cohort of persons living with and without HIV from 1996 to 2012. BMC Infect Dis. 2017 Feb 27;17(1):174. | COAST, Epidemiology and Population Health | Research Summary | Download | ||||||||||||||||||||||
| March, 2017 | nPEP Use Remains Low among Vancouver Gay, Bisexual and Men who Have Sex with Men | What are the key study findings? ¥ 51.9% of GBM living with HIV and 48.5% HIV-negative GBM had heard of nPEP. ¥ 3% of HIV-negative GBM who reported recent high-risk sex had used nPEP. ¥ Among HIV-negative GBM, nPEP awareness was higher among participants who were students, Caucasian, had used alcohol recently, had more sex partners, attended group sex parties, had been previously diagnosed with an STI, and identified as gay as opposed to bisexual. ¥ Among HIV-positive GBM, nPEP awareness was higher among participants who were Caucasian, had greater access to condoms, only had condomless sex with partners of the same HIV status, and had greater perceived agency to ask sexual partners their HIV status. Citation: S.Y, Lin, N.J. Lachowsky, M. Hull, A. Rich, Z. Cui, P. Sereda, J. Jollimore, K. Stephenson, M. Thumath, J.S.G. Montaner, E.A. Roth, R.S. Hogg, and D.M. Moore. "Awareness and Use of Nonoccupational Post-exposure Prophylaxis among Men Who Have Sex with Men in Vancouver, Canada." HIV Medicine HIV Med (2016). | Epidemiology and Population Health, Momentum | Research Summary | Download | ||||||||||||||||||||||
| March, 2017 | PrEP Awareness among Gay, Bisexual and Men who Have Sex with Men in Vancouver, Canada | Why is this study important? ¥ Gay, bisexual, and other men who have sex with men (GBM) account for about half of new HIV infections in Canada. ¥ Pre-exposure prophylaxis (PrEP) is an emerging biomedical HIV prevention tool for GBM and is approved for use in Canada, but does not currently receive public funding outside Quebec. ¥ This study aimed to evaluate awareness of PrEP among GBM living in Vancouver using data from 2012 to 2014. Citation: Lachowsky NJ, Lin SY, Hull M, Cui Z, Sereda P, Jollimore J, Rich A, Montaner JSG, Roth EA, Hogg RS, Moore DM. âPre-exposure Prophylaxis Awareness Among Gay and Other Men who have Sex with Men in Vancouver, British Columbia, Canada.â AIDS and Behavior (2016). | Epidemiology and Population Health, Momentum | Research Summary | Download | ||||||||||||||||||||||
| March, 2017 | Seroadaptive Strategies of Gay and Bisexual Men with the Highest Quartile Number of Sexual Partners in Vancouver, Canada | What is the importance of this study? ¥ Recent global reviews of HIV research literature have demonstrated continued disparities in the sexual health and wellbeing of gay and bisexual men (GBM) as compared with other men and women. ¥ One prominent factor associated with increased HIV risk is an individual's number of sexual partners. ¥ Despite continued research among this population, few studies have examined how men with more sexual partners manage their increased risk for HIV. Citation: Kiffer G Card, Nathan J Lachowsky, Zishan Cui, Paul Sereda, Ashleigh Rich, Jody Jollimore, Terry Howard, Robery Birch, Allison Carter, Julio Montaner, David Moore, Robert S Hogg, & Eric Abella Roth. (2016) Seroadaptive Strategies of Gay & Bisexual Men (GBM) with the Highest Quartile Number of Sexual Partners in Vancouver, Canada, AIDS and Behavior, DOI 10.1007/s10461-016-1510-y. | Epidemiology and Population Health, Momentum | Research Summary | Download | ||||||||||||||||||||||
| March, 2017 | Including Online-Recruited Seeds: A Respondent-Driven Sample of Men who Have Sex with Men | What is the importance of this study? ¥ Initial participants ('seeds') are critical to respondent-driven sampling (RDS) as they lead to more participants joining the study. Yet, there is little information available on how seeds that were recruited through online strategies may effect RDS implementation. ¥ We compared online-recruited seeds with offline-recruited seeds, as well as participants recruited by online-recruited seeds with participants recruited by offline-recruited seeds. Citation: Nathan J Lachowsky, Allan Lal, Jamie I Forrest, Kiffer G Card, Zishan Cui, Paul Sereda, Ashleigh Rich, Henry F Raymond, Eric A Roth, David M Moore, & Robert S Hogg. (2016). Including Online-Recruited Seeds: A Respondent-Driven Sample of Men Who Have Sex With Men, Journal of Medical Internet Research, 18:3, e51. DOI: 10.2196/jmir.5258 | Epidemiology and Population Health, Momentum | Research Summary | Download | ||||||||||||||||||||||
| March, 2017 | Lifetime Doctor-Diagnosed Mental Health Conditions and Current Substance Use among Gay and Bisexual Men Living in Vancouver, Canada | What is the importance of this study? ¥ Marginalization on the basis of sexual orientation increases the risk for problematic substance use and poor mental health. ¥ There is a link between an individual's mental health and substance use. ¥ Mental health conditions and substance use have important implications for clinical and public health practice. Citation: Nathan J Lachowsky, Joshun J S Dulai, Zishan Cui, Paul Sereda, Ashleigh Rich, Thomas L Patterson, Trevor T Corneil, Julio S G Montaner, Eric A Roth, Robert S Hogg, David M Moore. (2017). Lifetime Doctor-Diagnosed Mental Health Conditions and Current Substance Use Among Gay and Bisexual Men Living in Vancouver, Canada, Substance Use & Misuse. DOI: 10.1080/10826084.2016.1264965 | Epidemiology and Population Health, Momentum | Research Summary | Download | ||||||||||||||||||||||
| March, 2017 | A Latent Class Analysis of Seroadaptation among Gay and Bisexual Men | What is the importance of this study? ¥ Gay, bisexual, and other men who have sex with men (GBM) are at a disproportionately higher risk of HIV infection. ¥ Seroadaptive strategies take into consideration the known or assumed HIV status of individuals and their partners to avoid transmission. ¥ Understanding the patterns of seroadaptive behaviours may be useful for addressing GBM's sexual health needs. Citation: Card KG, Lachowsky NJ, Cui Z, Sereda P, Rich A, Jollimore J, Howard T, Birch R, Carter A, Montaner J, Moore D. Seroadaptive strategies of gay & bisexual men (GBM) with the highest quartile number of sexual partners in Vancouver, Canada. AIDS and Behavior. 2016 Aug 27:1-5. | Epidemiology and Population Health, Momentum | Research Summary | Download | ||||||||||||||||||||||
| March, 2017 | An Event-Level Analysis of Condom Use During Anal Intercourse among Self-Reported HIV-Negative Gay and Bisexual Men | What is the importance of this study? ¥ Across Canada, gay, bisexual and other men who have sex with men (GBM) accounted for over half of the new cases of HIV in 2014. ¥ New medical innovations may unintentionally lead to less condom use. ¥ There are gaps in knowledge of how condom use may have changed recently for HIV-negative GBM. Citation: Nathan J Lachowsky, Zach Tanner, Zishan Cui, Paul Sereda, Ashleigh Rich, Jody Jollimore, Julio SG Montaner, Robert S Hogg, David M Moore, & Eric A Roth. (2016). An Event-Level Analysis of Condom Use During Anal Intercourse Among Self-Reported Human Immunodeficiency Virus-Negative Gay and Bisexual Men in a Treatment as Prevention Environment. Sexually Transmitted Diseases, 43(12): 765-770. | Epidemiology and Population Health, Momentum | Research Summary | Download | ||||||||||||||||||||||
| March, 2017 | Does Age Matter? Sexual Event-Level Analysis of Age-Disparate Sexual Partners among GBM in Vancouver, Canada | What is the importance of this study? ¥ In Vancouver, one in five gay, bisexual and other men who have sex with men (GBM) live with HIV, with increasing prevalence by increasing age. ¥ There is a gap in knowledge and understanding of the sexual health implications of intergenerational relationships, which are relationships with a significant age difference between partners. Citation: Closson K, Lachowsky NJ, Cui Z, Shurgold S, Sereda P, Rich A, Moore DM, Roth EA, Hogg RS. Does age matter? Sexual event-level analysis of age-disparate sexual partners among gay, bisexual and other men who have sex with men (GBM) in Vancouver, Canada. Sexually Transmitted Infections. 2016 Nov 16:sextrans-2016-052721 | Epidemiology and Population Health, Momentum | Research Summary | Download | ||||||||||||||||||||||
| March, 2017 | Does Size Really Matter? A Sensitivity Analysis of the Number of Seeds in a Respondent-Driven Sampling Study of GBM in Vancouver, Canada | What is the importance of this study? ¥ While there is an estimate of the number of gay, bisexual and other men who have sex with men (GBM) in Vancouver, it is difficult to get a diverse and representative sample. ¥ Previous researchers have found certain sub-populations may be underrepresented in research data. Citation: Lachowsky NJ, Sorge JT, Raymond HF, Cui Z, Sereda P, Rich A, Roth EA, Hogg RS, Moore DM. Does size really matter? A sensitivity analysis of number of seeds in a respondent-driven sampling study of gay, bisexual and other men who have sex with men in Vancouver, Canada. BMC Medical Research Methodology. 2016 Nov 16;16(1):157. | Epidemiology and Population Health, Momentum | Research Summary | Download | ||||||||||||||||||||||
| March, 2017 | Exploring the Role of Sex-Seeking Apps and Websites in the Social and Sexual Lives of GBM | What is the importance of this study? ¥ There has generally been increased use of the internet and social networking tools, which may influence social behaviours. ¥ Gay and bisexual men's community involvement has changed over time: internet apps and websites are increasingly used to seek new partners. ¥ An individual's social network can influence their health and sex-seeking behaviour. Citation: Card KG, Lachowsky NJ, Cui Z, Shurgold S, Gislason M, Forrest JI, Rich AJ, Moore D, Roth E, Hogg RS. Exploring the role of sex-seeking apps and websites in the social and sexual lives of gay, bisexual and other men who have sex with men: a cross-sectional study. Sexual Health. 2016 Dec 16. | Epidemiology and Population Health, Momentum | Research Summary | Download | ||||||||||||||||||||||
| March, 2017 | Factors Associated with Productive Recruiting in a Respondent-Driven Sample of Men who Have Sex with Men in Vancouver, Canada | What does this study demonstrate? ¥ Underreported operational challenges of implementing respondent-driven sampling (RDS). ¥ Factors associated with productive recruiting in an urban RDS-generated sample of gay, bisexual and other men who have sex with men (MSM) in order to help other RDS researchers. ¥ The importance of social network size in RDS adjustment to validate RDS methods. ¥ Other social and behavioural variables that can improve the implementation of the recruitment strategy. Citation: Jamie I Forrest, Nathan J Lachowsky, Allan Lal, Zishan Cui, Paul Sereda, Henry F Raymond, Gina Ogilvie, Eric A Roth, David Moore, Robert S Hogg. (2016). Factors Associated with Productive Recruiting in a Respondent-Driven Sample of Men who have Sex with Men in Vancouver, Canada, Journal of Urban Health, 93:2, 379-387. DOI: 10.1007/s11524-016-0032-2. | Epidemiology and Population Health, Momentum | Research Summary | Download | ||||||||||||||||||||||
| March, 2017 | Emtricitabine-tenofovir alafenamide (Descovy™) | Formulary Addition and Criteria | Dear Doctor Letter | Download | |||||||||||||||||||||||
| February, 2017 | Women and HIV in British Columbia | Women make up approximately 18% of the population living with HIV in British Columbia. Women living with HIV can face unique barriers to care and challenges adhering to antiretroviral therapy (ART), compared with men. As a result, women often are not fully benefitting from the life-saving treatment available to them. In this issue of the HIV Pulse, we report on women living with HIV in British Columbia, using data from recent BC-CfE publications, the Provincial Quarterly Monitoring Reports and the BCCDC 2014 HIV Annual Report. | HIV Pulse | Download | |||||||||||||||||||||||
| February, 2017 | BC-CfE Drug Treatment Program Monthly Report (November 2016) | Drug Treatment Program | DTP Status Report | Download | |||||||||||||||||||||||
| February, 2017 | HIV Monitoring Quarterly Reports, Fourth Quarter 2016 | STOP HIV/AIDS | Treatment as Prevention¨ | ||||||||||||||||||||||||
| February, 2017 | Generic Antiretroviral Products | Notice of Change | Dear Doctor Letter | Download | |||||||||||||||||||||||
| January, 2017 | Government funding helps BC-CfE's Hope to Health grow |
Some of the province's most vulnerable people will benefit from research into HIV/AIDS, addiction and viral hepatitis that will be carried out at the world-class Hope to Health Research Centre following a successful expansion project supported in part through $2 million in government funding. "Through the BC Centre for Excellence in HIV/AIDS (BC-CfE), Vancouver has long been a leader in the research and treatment of HIV/AIDS," said Health Minister Terry Lake. "This work has dramatically changed the lives of people around the world. And now, through Hope to Health Research Clinic, the BC-CfE will continue to strengthen and inform health strategies through its groundbreaking research on HIV/AIDS, viral hepatitis and addiction." Hope to Health is a BC-CfE research clinic, which supports research to adapt, evaluate and expand Treatment as Prevention to other contagious diseases. Under the leadership of BC-CfE Director, Dr. Julio Montaner, the clinic focuses on three pillars: HIV, addiction and viral hepatitis. The expanded facility at 625 Powell Street will open to clients in February 2017. Hope to Health officially opened in June 2015 at 611 Powell Street in the Downtown Eastside. Following support from the world's most competitive peer-reviewed granting agencies and the $2 million provided to St. Paul's Foundation in 2015 to help the clinic expand, 625 Powell Street was further developed, adding an additional 186 square metres (20,000 square feet) to the existing facility. "The BC-CfE has a long and successful history of addressing the needs of some of the most vulnerable populations in B.C.," said Dr. Julio Montaner. "We are grateful to the Province for the trust it has put in our team to continue our research towards developing innovative, evidence-based health policy strategies to improve the lives of British Columbians and people around the world." Research from Hope to Health is helping to inform the work of the BC Centre on Substance Use (BCCSU), which was established in part through a $5 million investment announced in September 2016. The BCCSU is working with addictions experts around the province on research, education and training, and treatment guidelines to make sure substance-use treatment in B.C. is effective and evidence-based. "Addiction is one of the most prevalent and costly diseases in our society," said Dr. Evan Wood, interim director, BC Centre on Substance Use, BC-CfE, and medical director, Addictions Services, Vancouver Coastal Health and Providence Health Care. "The B.C. government's investment in the establishment of the BC Centre on Substance Use and in the expansion of Hope to Health is a reflection of its continued commitment to improve the lives of some of the most vulnerable people living in B.C., and will also play an important role in addressing the overdose crisis over the long-term." The BC-CfE has partnered with Vancouver Coastal Health to establish a low-threshold addiction clinic and an eye clinic also located at 625 Powell Street to serve people in the Downtown Eastside. Both clinics are set to open this spring. The addiction clinic will have a pharmacy onsite and will be able to dispense medications for treating substance use disorders and other issues including HIV and hepatitis C. Referrals can be made for treatment beds, counselling and other services not offered at the clinic. "Vancouver Coastal Health has worked successfully with the BC-CfE on numerous initiatives over the years, and we are pleased to expand that relationship with the opening of the addictions clinic, Connections, and our eye clinic," said Dr. Patricia Daly, vice-president, public health and chief medical health officer, Vancouver Coastal Health. "We strongly believe that together we can make a significant difference in addressing the overlapping health challenges of HIV, addictions and viral hepatitis." | Forecast Newsletter | Download | |||||||||||||||||||||||
| January, 2017 | BC-CfE Drug Treatment Program Monthly Report (October 2016) | Drug Treatment Program | DTP Status Report | Download | |||||||||||||||||||||||
| December, 2016 | Dr. Julio Montaner Responds to the Honourable Minister Jody Wilson-Raybould's World AIDS Day Statement |
The BC Centre for Excellence in HIV/AIDS (BC-CfE) supports and congratulates the Honourable Minister of Justice Jody Wilson-Raybould's statement regarding the criminalization of HIV non-disclosure. Her promise to re-examine the legislation is a welcome sign of an impending shift towards evidence-based laws to protect the human rights of those living with HIV, while reducing stigma. "… The over-criminalization of HIV non-disclosure discourages many individuals from being tested and seeking treatment, and further stigmatizes those living with HIV or AIDS. Just as treatment has progressed, the criminal justice system must adapt to better reflect the current scientific evidence on the realities of this disease," says Minister Wilson-Raybould in her World AIDS Day statement. Well-established and expanding scientific evidence shows an individual living with HIV can achieve a sustained undetectable viral load on effective and sustained HIV treatment. This leads to better quality of life and improved longevity for an individual, while reducing the chances they can transmit HIV to negligible. Despite research evidence and broad scientific consensus against it, in Canada an individual living with HIV is expected to proactively disclose his or her status before a sexual encounter—unless the individual has both an undetectable viral load and uses a condom. An individual living with HIV who doesn't disclose can be criminalized, even if HIV transmission did not occur. This places an excessive burden on individuals living with HIV who participate in consensual sexual relationships. In 2014, a group of leading Canadian scientists, including myself, released a statement expressing their concern that "the criminal law is being used in an overly broad fashion against people living with HIV in Canada because of, in part, a poor appreciation of the scientific understanding of HIV and its transmission." Next only to the United States, Canada has the dubious distinction of being one of the world's leaders in prosecuting individuals living with HIV for non-disclosure. The charge for HIV non-disclosure is mostly aggravated sexual assault, for which the penalty can be up to 10 years and a damaging sexual offender registration. The law can negatively impact already marginalized and criminalized populations, including marginalized women. Out of 14 women charged for HIV non-disclosure in Canada, 10 have been charged with aggravated sexual assault. If Canada is to be a leader in the effort to reach an AIDS-free generation, as established as a goal by the United Nations, we need to set the example for the world. Already, other countries including Switzerland, Congo, Guinea, Togo, and Senegal have revised their HIV non-disclosure laws or adopted new legislation limiting the use of criminal law only to cases of intentional transmission. On behalf of the BC-CfE, I applaud Minister Wilson-Raybould's commitment to advancing progress against discrimination and stigma towards people with HIV. The Minister's highlighting on World AIDS Day of HIV non-disclosure criminalization and her commitment to address this law as an important issue show her compassion and dedication to the more than 70,000 individuals living with HIV in Canada — and to the millions living with HIV worldwide. | Forecast Newsletter | Download | |||||||||||||||||||||||
| December, 2016 | BC-CfE Drug Treatment Program Monthly Report (September 2016) | Drug Treatment Program | DTP Status Report | Download | |||||||||||||||||||||||
| November, 2016 | HIV Monitoring Quarterly Reports, Third Quarter 2016 | STOP HIV/AIDS | Treatment as Prevention¨ | ||||||||||||||||||||||||
| October, 2016 | BC-CfE Drug Treatment Program Monthly Report (August 2016) | Drug Treatment Program | Download | ||||||||||||||||||||||||
| October, 2016 | Together, we can stop HIV/AIDS: Treating Social Determinants Of Health Can Help End HIV/AIDS |
Picture this scenario: An individual living with HIV in British Columbia, "Doug" (whose name has been changed for privacy), was being "shuffled around" through care. As a result, he had grown tired and had mostly given up on treating his HIV. Sadly, he had begun telling family and friends that he wouldn't be around much longer. Can you see a solution to a situation like this? There was an answer for Doug. An outreach worker, with the province of British Columbia's STOP® Program (Seek and Treat for Optimal Prevention of HIV/AIDS), knocked on his door and started to connect him to services to help support his medical adherence. Doug needed to have a regular health care provider, and the outreach worker set him up with one. Beyond that, he needed the supports to help him stay consistent with care. He was placed in supportive housing, as well as in an integrative care program where he could develop his interests in music. Eventually, Doug (an electrician by trade who plays and builds musical instruments) became healthy, fully adherent to HIV medications and achieved an undetectable viral load. Stories like Doug's are very personal and individual victories. However, they show the changes that can take place when addressing systemic social and economic barriers. B.C.'s STOP® Program, based on principles of the Treatment as Prevention (TasP®) strategy developed at the BC Centre for Excellence in HIV/AIDS (BC-CfE), acknowledges the importance of addressing social and economic inequities — termed social determinants of health. The STOP® Program aims to expand and offer access to HIV testing, care and treatment for medically eligible B.C. residents, particularly for populations experiencing difficulties in accessing traditional services. The concept behind STOP® is to immediately offer universal HIV treatment to those diagnosed with the disease. This TasP® approach has led to improved health outcomes and to a consistent drop in new HIV cases in B.C. Once on sustained and consistent treatment, an individual's viral load declines making it highly unlikely they will transmit the virus. B.C. is the only province to implement TasP® and the only one to see a consistent drop in new HIV cases. Globally, the United Nations has adopted a plan to end AIDS by 2030 that is based on principles of TasP®. Organizations like the Global Fund are on board with this plan to #EndItForGood and make the next generation AIDS-free. In B.C., through TasP® and STOP® we have seen successes like Doug's. We have seen people living with HIV who use injection drugs, a population some doubted could maintain consistent treatment, achieve improved health and see significant reductions in HIV transmission (in B.C., through consistent access to HIV treatment, the number of people who inject drugs who achieved an undetectable viral load increased from 30% in 2006 to 71% in 2012). How does the STOP® program work? It all starts with using resources to build more pathways to care and treatment. Even in a largely resource-rich nation like Canada, mental health, addiction, homelessness and poverty can present obstacles to this goal. Across the province, members of multi-disciplinary, collaborative outreach teams under the STOP® program — which can include nurses, outreach workers, social workers and others — serve the most vulnerable populations. Clients may have suffered trauma and lack trust in traditional health care systems. For example, people who inject drugs and sex workers may feel stigmatized or discriminated against within the health care setting. Many clients are confronting an intersection of challenges: They may simultaneously be facing addiction and homelessness problems, while dealing with access to HIV treatment and care. Individuals living with HIV may also have mental health disorders, like depression or anxiety, leaving them unable to take the steps towards self-care. According to previous research, individuals living with HIV are two to ten times more likely to have at least one mental health condition, in comparison to the general population. Despite such challenges, the STOP® program, conducted through B.C.'s health authorities has made headway in the fight against HIV/AIDS: After initial success as a pilot program in Vancouver and Prince George, STOP® was expanded provincially along with a $19.9 million investment from the provincial government. In September, Northern Health, a B.C. health authority providing health services to 300,000 people over an area of 600,000 square kilometers, awarded $1.59 million to eight agencies and 23 First Nations communities as part of the provincial STOP® initiative. | Treatment as Prevention® | Forecast Newsletter | Download | ||||||||||||||||||||||
| October, 2016 | BC-CfE Drug Treatment Program Monthly Report (July 2016) | Download | |||||||||||||||||||||||||
| September, 2016 | Queensland HIV Treatment as Prevention® Roadshow a Success |
The BC Centre for Excellence in HIV/AIDS (BC-CfE) was thrilled to have been invited to take part in a two-week Queensland, Australia, HIV Treatment as Prevention (TasP®) Roadshow, organized by the HIV Foundation Queensland (HIVFQ). Since signing a memorandum of understanding with the BC-CfE and formally adopting the TasP strategy in 2014, Queensland has worked diligently to improve education and engagement with health professionals and the community for timely access to highly active antiretroviral treatment (HAART). The TasP Roadshow traveled to eight different locations across Queensland between July 25 and August 4, 2016, in a series of accredited meetings with a broad range of health professionals and Hospital and Health Services (HHS) executive teams and community representatives. This platform provided a unique opportunity for the HIVFQ and the BC-CfE to provide updates on state, national and international policy, program and clinical developments in the rapidly evolving landscape of HIV TasP®. Key discussion points included increased testing, early engagement and sustainment in care, treatment, postexposure prophylaxis (PEP), preexposure prophylaxis (PrEP), and development of communication strategies. Key BC-CfE speakers included Dr. Rolando Barrios, Assistant Director; Irene Day, Director of Operations; Glen Bradford, Peer Navigation and Prison Outreach Programs, Positive Living British Columbia; Prof. James Ward, South Australia Health and Medical Research Institute; Dr. Andrew Redmond, Infectious Disease Physician, Royal Brisbane and Women's Hospital; and Simon Doyle Adams, Queensland PrEP Demonstration Project Coordinator, Cairns Sexual Health Clinic. Dr. Darren Russell, Chairperson of the HIV Foundation Queensland, and Dr. Barrios discussed the TasP Roadshow. HIV TasP Roadshow Objectives:
| Treatment as Prevention® | Forecast Newsletter | Download | ||||||||||||||||||||||
| September, 2016 | nPEP Use Remains Low among Vancouver Gay, Bisexual and Men who Have Sex with Men | Epidemiology and Population Health, Momentum | Download | ||||||||||||||||||||||||
| September, 2016 | PrEP Awareness among Gay, Bisexual and Men who Have Sex with Men in Vancouver | Epidemiology and Population Health, Momentum | Download | ||||||||||||||||||||||||
| September, 2016 | BC-CfE Drug Treatment Program Monthly Report (June 2016) | Drug Treatment Program | DTP Status Report | Download | |||||||||||||||||||||||
| August, 2016 | HIV Monitoring Quarterly Reports, Second Quarter 2016 | STOP HIV/AIDS | Treatment as Prevention¨ | ||||||||||||||||||||||||
| August, 2016 | Opioid Addiction Guidelines from British Columbia featured in leading medical journal |
A novel approach to treating opioid addiction in British Columbia is attracting major international attention after being reviewed and featured in the prestigious Journal of the American Medical Association (JAMA). A Guideline for the Clinical Management of Opioid Addiction, a first-of-its-kind in Canada, aims to improve health professionals' knowledge of the range of evidence-based treatments available for opioid addiction, one of the most challenging forms of addiction facing the health care system today. Untreated opioid addiction is a major driver of the recent surge in illicit drug overdose deaths, which prompted B.C.'s Provincial Health Officer, Dr. Perry Kendall, to declare a public health emergency earlier this year. In the absence of evidence-based recommendations, dangerous practices like offering medical detoxification as an isolated strategy have been common for many years whereas methadone has been the primary first line medication for treating opioid addiction. With support from the Province of British Columbia, the guidelines were developed to articulate the diversity of possible treatment options that can be staged and tailored to individual patient needs. The guideline's unique suggestions include recommending buprenorphine/naloxone (trade name Suboxone®), as the preferred first-line treatment for opioid addiction. According to research summarized in the guidelines, Suboxone® is six times safer than methadone in terms of overdose risk, and permits more flexible "take home" rather than pharmacy dosing. The guidelines support using a stepped and integrated care approach where treatment intensity is continually adjusted to match individual patient needs and circumstances over time, and recognize many individuals may benefit from the ability to move between treatments. "By incorporating principles of evidence-based medicine into addiction care, the province has the potential to realize a dramatic reduction in the public health and community concerns arising from untreated addiction," said Dr. Evan Wood, guideline committee chair and Professor of Medicine at the University of British Columbia, Medical Director of Addiction Services at Vancouver Coastal Health and Providence Health Care, and Director of the Urban Health Research Initiative at the BC Centre for Excellence in HIV/AIDS. In August 2014, Health Minister Terry Lake announced an initial $3 million investment to support Dr. Wood's research, education and clinical care guidance program in an effort to harness new ways to treat addiction and related health concerns. The guidelines are one example of the foundational work made possible through this partnership. "It is great to see our investments in improving the addiction system of care are generating international recognition and, given the seriousness of the opioid overdose crisis, there is an urgent need to expand this work provincially and move on recent changes that have been made to improve access to evidence-based treatment," said B.C. Health Minister, Terry Lake. Most recently, in order to expand patient access to opioid addiction treatment in the province, the College of Physicians and Surgeons of B.C. lifted restrictions on prescribing Suboxone®. This regulatory change has been recommended by health researchers in the Canadian Research Initiative in Substance Misuse (CRISM), who issued a report calling for improved access to evidence-based treatment for opioid addiction as a strategy to address the provincial overdose crisis. Credited with an 80 per cent reduction in fatal opioid overdoses in France, Suboxone® can now be prescribed by primary care and generalist physicians in B.C. "I'm pleased to see the province's approach to addiction is moving towards one where care providers can be guided by the best available evidence for the prevention and treatment of addiction," said Leslie McBain, community advocate and founding member of Moms Stop the Harm, whose son Jordan died of a prescription drug overdose. "If these new policies and expert guidelines were available provincially when my son was struggling with addiction, we may have been successful in our efforts to identify a physician who could provide life-saving treatment." The opioid addiction treatment guidelines were developed by an interdisciplinary committee comprised of individuals from Vancouver Coastal Health, Providence Health Care and representatives from the B.C. Ministry of Health. The guidelines were subsequently peer-reviewed by patient and family groups as well as local and international experts in the field. Authors of the opioid addiction treatment guidelines have partnered with the BC Association for People on Methadone to disseminate the guidelines and information to public and private clinics around the Lower Mainland, with additional outreach efforts underway in other B.C. health authorities. | Treatment as Prevention® | Forecast Newsletter | Download | ||||||||||||||||||||||
| August, 2016 | BC-CfE Drug Treatment Program Monthly Report (May 2016) | Drug Treatment Program | DTP Status Report | Download | |||||||||||||||||||||||
| June, 2016 | BC-CfE welcomes delegation from Saskatchewan and Alberta to present TasP®-focused HIV research |
Dr. Julio Montaner and his team from the BC Centre for Excellence in HIV/AIDS (BC-CfE) were pleased to host guests from the Saskatoon Tribal Council, Alberta Medical Office of Health, Alberta Health Services, Saskatoon Police Service, Saskatoon Health Region, Kahui Taotoko, and Health Canada over two days this past June to highlight the latest cutting-edge HIV research from the BC-CfE. New HIV diagnoses have continued to escalate in Saskatchewan, disproportionately affecting injection drug users, women, and the Indigenous community. This is a dramatic shift from a decade ago when HIV/AIDS cases in Canada were mostly found in B.C., Ontario and Quebec. As a result, leading health care professionals, policy makers, and community members from Saskatchewan reached out to the BC-CfE to learn more about its successful Treatment as Prevention Strategy (TasP®). It was not that long ago when B.C. was the Canadian epicentre of the HIV/AIDS epidemic. Twenty-five years later, B.C. is considered a world-wide success story. Yet, there are parallels to Saskatchewan which mirror the British Columbia of those early days. How was B.C. able to dramatically reduce HIV morbidity and mortality, as well as new cases of HIV, and what learnings can Saskatchewan embrace from BC-CfE's experience to curb the spread of HIV? It took the collective effort of the community; scientific, academic and medical researchers; funding and support from the B.C. government; and buy-in from the Vancouver Police Department to get to where B.C. is today. The introduction of highly active antiretroviral therapy (HAART) in 1996 transformed HIV. HAART virtually eliminates progression of the disease. As a result, HAART has converted HIV/AIDS into a chronic manageable disease, with an anticipated near normal longevity. Beyond the individual level impact of HAART, the treatment has a public health impact because it virtually stops HIV transmission. As a result, a properly implemented and facilitated HAART program can virtually stop disease progression to AIDS and death and new infections. Of note, the strategy has now been shown to be highly cost effective in the short-term, and cost averting over a decade or two. The made-in-BC TasP strategy has been implemented around the world in China, Panama, France, Brazil, Spain, Argentina, Swaziland, Queensland, San Francisco, New York City, and many more. More recently, in June 2016, the United Nations and member countries formally endorsed our TasP inspired 90-90-90 treatment target as the means to transform the HIV/AIDS pandemic into a sporadic disease by 2030. The 90-90-90 treatment target proposes that by 2020:
Currently, cities such as Indiana, Indianapolis, and Glasgow, Scotland, are reeling from an epidemic of HIV and hepatitis C with some striking similarities to the situation in Saskatchewan. The proven success of TasP®, combined with harm reduction and addiction management efforts, offer the hope of eventually eliminating HIV/AIDS in these areas and around the world. The BC-CfE would like to extend special thanks to the BC-CfE Staff, as well as Réka Gustafson, medical health officer and director of Vancouver Coastal Health Disease Control; Elizabeth Holiday, Regional Leader HIV Prevention, Regional HIV Services, Vancouver Coastal Health; Inspector Howard Tran and Superintendent Michelle Davey from the Vancouver Police Department; and Gina McGowan, Director, Blood Borne Pathogens, Population and Public Health, B.C. Ministry of Health; who graciously joined the meeting to present their findings and answer questions. | Treatment as Prevention® | Forecast Newsletter | Download | ||||||||||||||||||||||
| June, 2016 | BC-CfE Drug Treatment Program Monthly Report (March 2016) | Drug Treatment Program | DTP Status Report | Download | |||||||||||||||||||||||
| May, 2016 | HIV Monitoring Quarterly Reports, First Quarter 2016 | STOP HIV/AIDS | Treatment as Prevention¨ | ||||||||||||||||||||||||
| May, 2016 | B.C. gives $5 million to expand efforts to curb hepatitis C infection |
The provincial government has provided $5 million to the St. Paul's Hospital Foundation for a research study on how to reduce new infections of hepatitis C virus (HCV) in the province, announced Health Minister Terry Lake today, along with BC Centre for Excellence in HIV/AIDS (BC-CfE) director Dr. Julio Montaner. "This investment will help those at increased risk of re-infection with hepatitis C, by focusing on engagement with the health system, and it will help to evaluate the health outcomes with our current treatment regimens," said Lake. "Through this project, we are working to improve the lives of those people with hepatitis C. "This initiative offers a unique opportunity to potentially curb the rapidly rising toll of hepatitis C in North America," said Dr. Montaner." It will inform the next steps needed to improve engagement in care and timely treatment of HCV positive British Columbians to improve patient outcomes." The research will focus on individuals in Vancouver who have been successfully cured of hepatitis C, but who have been identified as being at increased risk of re-infection. It will also evaluate the impact and outcomes of current hepatitis C treatments, and identify the next steps required to optimize treatment outcomes in B.C. "Participants will be engaged with the full array of harm reduction and support services available through Vancouver Coastal Health," said Dr. Patricia Daly, Vancouver Coastal Health's chief medical health officer and vice president, public health. "We will work with the project team to evaluate how these supports help to prevent re-infection with hepatitis C." Under the leadership of Dr. Montaner, the project will be a collaboration between the BC-CfE, BC Centre for Disease Control, Vancouver Coastal Health, St. Paul's Hospital Foundation and University of British Columbia. "By understanding how to optimize treatment outcomes, we can maximize the individual and societal impact of these very promising therapies," said Dr. Mel Krajden, medical lead for hepatitis at the BC Centre for Disease Control. Hepatitis C virus infection can be a life-threatening communicable disease affecting an estimated 50,000-60,000 British Columbians. Approximately 35 per cent of people currently living with hepatitis C may be at higher risk for re-acquiring the virus after successful treatment, including people who inject drugs, men who have sex with men, and commercial sex workers. Modern hepatitis C therapies are highly effective, with cure rates over 95 per cent. However, the risk for re-infection following successful treatment is potentially high among certain groups, unless they engage in risk reduction practices. Hepatitis C is the most frequent cause of premature death among reportable infectious diseases in North America, and has become the most frequent cause of premature death among people living with both hepatitis C and HIV. Learn more at www.cfenet.ubc.ca. | Forecast Newsletter | Download | |||||||||||||||||||||||
| May, 2016 | Low Prevalence of Unsuppressed Viral Load among Gay and Bisexual Men Living with HIV in Vancouver: BC-CfE Momentum Study | 93% of gay and bisexual men living with HIV are accessing HIV treatment, but additional strategies are needed to engage low-income and non-white men.What are the key study findings?
| Epidemiology and Population Health, Momentum | Download | |||||||||||||||||||||||
| May, 2016 | BC-CfE Drug Treatment Program Monthly Report (February 2016) | Drug Treatment Program | DTP Status Report | Download | |||||||||||||||||||||||
| April, 2016 | Western Aboriginal Harm Reduction Society peer-driven research helping to bridge knowledge gaps |
Located in Vancouver's Downtown Eastside (DTES), on the unceded territories of the Coast Salish peoples, many have found welcome at the Western Aboriginal Harm Reduction Society (WAHRS), where groundbreaking research is helping to rewrite our understanding of substance use and addiction. Members are current or former illicit drug and/or illicit alcohol users from diverse Indigenous backgrounds. At WAHRS, members are given an opportunity to have their voices heard, empowered to fight for themselves and to educate policy makers, healthcare professionals, researchers, and others about members' strengths and challenges. The group's membership includes over 300 individuals and falls under the umbrella of the Vancouver Area Network of Drug Users (VANDU), with over 3000 members. WAHRS members participate in weekly meetings, healing circles, and, during at least four months of the year, go out to the University of B.C. farm on Musqueam territory where they have a chance to connect with nature, help during harvest or work in the kitchen. An important part of empowering members is WAHRS' involvement in community protests and advocacy work. WAHRS has worked since 2011 in partnership with researchers from the BC Centre for Excellence in HIV/AIDS (BC-CfE) Urban Health Research Initiative. The research aims to better understand members' experiences with access to healthcare, access to addictions treatment, involvement in research, and HIV/AIDS. It is their culturally appropriate methods and meaningful participation in policy and program development that sets WAHRS and their research apart. The BC-CfE had the pleasure of sitting down with the WAHRS board of directors for an interview recently. BC-CfE – Why do you think this cultural sharing and research is important to do? WAHRS – Our work is important because the research is done by WAHRS members. WAHRS Board Members decide on research questions, collect data, analyze results, and develop recommendations for change, with background help from BC-CfE researchers. WAHRS members all share similar experiences so our research talking circles are a safe, relaxed place where people can share stories that aren't usually heard. The research process was developed using indigenized ways, like the eagle feather and use of talking circles. Part of this process is bringing back findings from the research to our members so they know the results and see the impact of their participation. BC-CfE – What else does WAHRS do that celebrates the organization? WAHRS – We are very active within the community. One of the many ways is by getting involved in protests and advocacy work that deal with Indigenous issues. Idle No More and the DTES Murdered and Missing Women March are examples of efforts we actively support. Our members participate in a number of initiatives such as the Mayor's Mental Health and Addiction Task Force, Aboriginal Healing and Wellness Centre, Sex Workers United Against Violence, and several others. We also write letters of support or recommendation for studies and advocacy initiatives. BC-CfE – What recommendations came from the work done with the BC-CfE Urban Health Research Initiative? WAHRS – Our findings show the huge amount of trauma, grief, pain and basic survival instincts experienced by members. We have developed a regular healing circle to help address this pain among our members. There is also a need for more addictions specialists and healthcare workers trained in addictions since our health needs are not being met by most healthcare professionals. We need healthcare that connects to our culture and the Creator. There still are gaps in the knowledge about HIV in our communities, but this continued research is helping to bridge those gaps. Under all our findings is people just want to be treated with dignity. WAHRS ends their meetings by remembering friends and family they've lost to the war on drugs and war on the poor. Their research is dedicated to forever WAHRS members, including Cliff, Brian and Melwyn. You may want to pause and reflect now. All our relations. "Presentations are an opportunity to break down stereotypes and teach people. Education is key." – WAHRS member. | Forecast Newsletter | Download | |||||||||||||||||||||||
| March, 2016 | Landmark Study Reveals Growth of Hepatitis C Epidemic Peaked around 1950 | Globally, 185 million people are living with hepatitis C virus (HCV). There are 300,000 people living with HCV in Canada and 3.5 million people living with HCV in the United States. The vast majority of adults infected with HCV in North America, as well as some other developed countries, are part of the generational cohort composed of individuals born between 1945 and 1964 (called “the baby boomers”). Previous studies implicated both use of infected blood products (prior to the screening of the blood supply) and injection drug use as major contributors to the epidemic in this demographic group. | Treatment as Prevention¨ | Download | |||||||||||||||||||||||
| March, 2016 | BC-CfE welcomes delegates from the Public Health Agency of Canada |
New Liberal government encourages atmosphere of scientific opennessThe BC Centre for Excellence in HIV/AIDS (BC-CfE) was pleased to welcome delegates from the Public Health Agency of Canada (the Agency) in March 2016. Researchers from the BC-CfE presented an overview of the BC-CfE and discussed opportunities for collaboration. Dr. Julio Montaner, BC-CfE Director, and research team members met with Dr. Gregory Taylor, Canada's Chief Public Health Officer and Krista Outhwaite, President, Agency, joined by Agency colleagues Bill Slater, Manager, Policy, Planning and Inter-governmental Affairs, and Sheena Sargeant, Program Consultant. "It is truly a pleasure for the BC-CfE to share some of our research and innovative work in HIV, addictions, and viral hepatitis," said Dr. Montaner. "We welcome this renewed dialogue and look forward to further collaborating with the Public Health Agency." Led by the Minister of Health, Jane Philpott, the Agency's mission is to promote and protect the health of Canadians through leadership, partnership, innovation and action in public health. The Agency has put in place programs, services and policies that protect and promote the health of all Canadians. In Canada, public health is a responsibility that is shared by all three levels of government in collaboration with the private sector, non-governmental organizations, health professionals and the public. Both Minister Philpott and Prime Minister Justin Trudeau have been open in their support for the UNAIDS 90-90-90 Target. The global target calls for 90% of people living with HIV to know their status, 90% of all those people diagnosed with HIV to be on treatment, and 90% of people on treatment to successfully manage their infection by 2020. The 90-90-90 Target was built on the backbone of the made-in-BC Treatment as Prevention® strategy. Achieving these goals will move the world towards the goal of ending the AIDS epidemic by 2030. "The Public Health Agency of Canada is committed to address HIV in Canada through the Federal Initiative and we look forward to working with Dr. Montaner and his team to achieve the 90-90-90 Target," said Krista Outhwaite. The Federal Initiative provides funding for prevention and support programs reaching key priority populations, as well as research, surveillance, public awareness, and evaluation. The Federal Initiative signals a renewed and strengthened federal role in the Canadian response to HIV/AIDS. The goals of the Federal Initiative are to:
| Treatment as Prevention® | Forecast Newsletter | Download | ||||||||||||||||||||||
| March, 2016 | BC-CfE Drug Treatment Program Monthly Report (December 2015) | Drug Treatment Program | DTP Status Report | Download | |||||||||||||||||||||||
| February, 2016 | HIV Cascade of Care in British Columbia | The HIV Cascade of Care (also known as Care Continuum) provides a framework for service providers and policymakers to measure progress according to steps in the delivery of HIV treatment and care. It allows us to assess development towards HIV prevention and care goals, identifying gaps in sustained patient care. In this volume of HIV Pulse, using data from the Provincial Quarterly Monitoring Reports (from October 2013 to December 2015), we report on findings from the HIV Cascade of Care in British Columbia. | HIV Pulse | Download | |||||||||||||||||||||||
| February, 2016 | HIV Monitoring Quarterly Reports, Fourth Quarter 2015 | STOP HIV/AIDS | Treatment as Prevention¨ | ||||||||||||||||||||||||
| February, 2016 | Federal, Provincial and Territorial Ministers of Health Meet in Vancouver |
Dr. Julio Montaner honoured to be invited to present on Treatment as Prevention®Vancouver recently hosted the conference of the Provincial and Territorial Ministers of Health, joined by federal Health Minister Jane Philpott, who gathered to discuss key health priorities for Canadians. After a decade of silence from the federal government regarding endorsement of Treatment as Prevention (TasP®) as a national strategy and other evidence-based strategies to combat HIV, Dr. Julio Montaner, BC-CfE Director, was honoured to have been invited to present to the Ministers of Health during the conference. The presentation was entitled "Treatment as Prevention: From Research Hypothesis to Global Policy and Beyond." Dr. Montaner demonstrated how the TasP strategy has prevented morbidity, premature mortality, and HIV transmission while proving to be cost-saving. This strategy has opened the door to a new concept of targeted disease elimination based on the selective use of TasP® to markedly reduce the burden of specific infectious diseases (e.g. viral hepatitis, tuberculosis, addictions, etc.) with the aim of enhancing healthcare sustainability. In stark contrast to its predecessor, the new Liberal government publicly endorsed adoption of the global plan to end AIDS. Even before the federal elections took place, the Leader of the Liberal Party of Canada, Justin Trudeau, announced his support in a letter to Dr. Montaner dated October 8, 2015, for the adoption of the global plan to end AIDS, and called on Canada to make a commitment on the world stage. Following the federal elections, Minister Philpott echoed this sentiment in a World AIDS Day statement where she said, "Canada endorses the United Nations Joint Programme on HIV and AIDS (UNAIDS) global HIV treatment targets - known as the 90-90-90 Target. This global target calls for 90% of people living with HIV to know their status, 90% of all those people diagnosed with HIV to be on treatment, and 90% of people on treatment to successfully manage their infection by 2020. Achieving these goals will help get the world on track to end the AIDS epidemic by 2030." In another sign Justin Trudeau's Liberals have a very different approach to illicit drugs than the previous government, prior to the commencement of the conference, Minister Philpott toured Insite, Vancouver's downtown east side supervised-injection site. She called her visit "extremely moving" and gave a heartfelt stamp of approval. Broad agreements on key topicsAlthough a new health accord was not adopted during the conference, the Federal, Provincial and Territorial Ministers of Health did make an announcement on some broad agreements on key topics which included: shared health priorities, funding commitments, care in the community, health innovation, next steps, indigenous health, physician assisted dying, prescription drug abuse, and health promotion and prevention. In an excerpt from the statement, the Ministers of Health wrote: "We agreed that strong, universally accessible, publicly financed health-care systems are an essential foundation for a strong and prosperous Canada. We affirmed our commitment to continue transforming and strengthening health-care systems so that they can provide high-quality, accessible and patient-centered health services in a sustainable way. To this end, we, as Federal, Provincial and Territorial Ministers, agreed to work individually and collectively on the following immediate priorities where efforts will yield the greatest impact:
Read the statement at bit.ly/MinistersOfHealth2015. | Treatment as Prevention® | Forecast Newsletter | Download | ||||||||||||||||||||||
| January, 2016 | BC-CfE Drug Treatment Program Monthly Report (November 2015) | Drug Treatment Program | DTP Status Report | Download | |||||||||||||||||||||||
| December, 2015 | BC-CfE Drug Treatment Program Monthly Report (October 2015) | Drug Treatment Program | DTP Status Report | Download | |||||||||||||||||||||||
| December, 2015 | The BC-CfE welcomes Dr. Jeannie Shoveller, new Director of Epidemiology and Population Health and the Drug Treatment Program |
The BC Centre for Excellence in HIV/AIDS (BC-CfE) is pleased to share the news Dr. Jeannie Shoveller has accepted the position of Director of Epidemiology and Population Health and the Drug Treatment Program, beginning January 4, 2016. Originally from Nova Scotia, Dr. Shoveller has called British Columbia home since 1993. She completed a PhD in Interdisciplinary Studies (1997) and her post-doctoral training (1999) at the University of British Columbia (UBC). She accepted an appointment in the UBC Faculty of Medicine in 1999, where she continues to work as a Professor in the School of Population and Public Health. Her research focuses on the health effects of social inequities — including the effects of unfair distribution of income, barriers to educational attainment, ageism, homophobia, and gender bias on HIV-related outcomes. Dr. Shoveller has served as Principal Investigator on more than 20 studies, published over 100 peer-reviewed manuscripts, and supervised more than 50 graduate students and post-doctoral fellows. She has received awards for her scholarship from prestigious institutions, including the Michael Smith Foundation for Health Research, the Canadian Institutes of Health Research, and the European Union Commission. In 2015, she was inducted into the Canadian Academy of Health Sciences in recognition of her leadership and contributions to health and social equity nationally and internationally. Dr. Shoveller is excited to join the BC-CfE and said, "Throughout my career, I have worked alongside amazing people, including colleagues at the BC-CfE. I am truly honoured to accept this new role. It will allow me to work with people whom I respect greatly and provide opportunities to make new contributions that address the needs of the communities we serve." Raised on the Barteaux family farm in Clarence, Nova Scotia, Dr. Shoveller credits her parents for instilling in her a love of doing meaningful work in an honest, gracious and generous manner. She brings the same level of enthusiasm and discipline to her academic endeavours. Many might be surprised to learn that after launching a new project in Brazil, she challenged herself to learn Portuguese, initially enrolling in evening classes at Langara College. She has spent the past decade improving her Portuguese language proficiency, which has been helpful to her HIV-related research collaborations in Brazil, where she also had been a Visiting Professor at the Federal University of Rio de Janeiro, the State University of Rio de Janeiro, and the Federal University of Rio Grande do Sol. Married for over 25 years to her husband Tim (an English teacher), Dr. Shoveller shares a quote from one of her favourite poets, Elizabeth Bishop (an adopted Nova Scotian): "The armored cars of dreams, contrived to let us do so many a dangerous thing." When asked what this means to her, Dr. Shoveller said, "It's important to think big, as it allows us to do things we might otherwise never have tried." Keeping that sentiment in mind, we are very pleased to welcome Dr. Shoveller to the BC-CfE and look forward to working together for many years to come. | Forecast Newsletter | Download | |||||||||||||||||||||||
| December, 2015 | HIV Monitoring Quarterly Reports, Third Quarter 2015 | STOP HIV/AIDS | Treatment as Prevention¨ | ||||||||||||||||||||||||
| November, 2015 | Getting to Zero: A Call for World AIDS Day |
Ending AIDS as a pandemic is very possible and can be done using our made-in-Canada Treatment as Prevention (TasP) strategy, a disease elimination strategy pioneered by the BC Centre for Excellence in HIV/AIDS (BC-CfE). UNAIDS has embraced the ambitious goal of ending AIDS by 2030, and this has now been formally endorsed within the United Nation's Sustainable Development Goals agenda. On World AIDS Day, UNAIDS will be calling for the world to achieve "Zero new HIV infections. Zero discrimination. Zero AIDS-related deaths." Over the last decade in B.C., with the implementation of TasP and the unwavering support of the provincial government, the number of AIDS-related deaths has dropped by over 80 per cent and the number of new HIV cases has dropped by over 65 per cent. This stands in contrast to the rest of Canada, where HIV and AIDS remain far from controlled. Moreover, investing in a TasP strategy and its related "90-90-90" target will drive better individual outcomes, better public health outcomes, and promote health care sustainability. According to research from the BC-CfE, over the next 25 years the implementation of TasP in B.C. will save over $65 million. Similarly, implementing the strategy in South Africa would save up to 5.5 million lives and US$28.7 billion within forty years. And the return on the investment becomes very attractive, very quickly, as UNAIDS predicts a 15-fold return on the investment over five years. Expanding HIV treatment broadly, including hard-to-reach and often-stigmatized populations such as people who inject drugs, creates a more efficient, less-siloed approach to health care. It also helps to reduce discrimination. A concerted approach to meeting the needs of these hard-to-reach populations has proven markedly effective in reducing the impact of HIV and AIDS in BC. With the use of aggressive harm reduction strategies - including the expansion of needle exchange, opioid substitution therapy, observed therapy programs, peer navigators, medicalized heroin, and supervised injection sites to support the expansion of HIV testing and HAART access in this community - the province has seen a nearly 90 per cent decrease in AIDS morbidity and mortality, and HIV incidence among people who inject drugs. Further, the fundamentals behind TasP as part of a disease elimination strategy can be applied to other infectious diseases, including hepatitis C virus (HCV). Globally, approximately 200 million people (about 3 per cent of the world population) are currently infected with HCV, including about 240,000 in Canada. We need to urgently deploy a widespread HCV testing campaign across Canada and facilitate access to lifesaving therapy. As the HIV TasP strategy demonstrates, the approach of saving money by restricting access to HCV testing and treatment is draconian, short-sighted and counterproductive. With the recent return of a federal Liberal government that supports science and evidence-based policymaking, Canada has a unique opportunity to reclaim the leadership role it relinquished almost a decade ago. Central to this would be to implement TasP and adopt the UN 90-90-90 target as a national HIV/AIDS strategy. Next, the new federal government is expected to endorse and champion the UNAIDS campaign to have this made-in-B.C. strategy adopted throughout Canada and globally. This represents a unique opportunity for our country to take much-deserved credit for a major global health care contribution. However, this is not just about testing or making treatment available to those in need. For almost a decade, Canada has dealt inappropriately with the most at-risk populations. It is time for the laws of this land to be revised in order to work in synergy with, rather than against, public health efforts. We trust this is high on the agenda of the newly installed Trudeau government. This World AIDS Day, we welcome a new era of evidence-based decision-making at the federal level. This will serve to deliver on the promise of ending AIDS within our generation. We have the means, and we have the road map, we just need the political will. The time is now: Canada is back in the business of defeating AIDS domestically, and providing global leadership to end AIDS by 2030. | Treatment as Prevention® | Forecast Newsletter | Download | ||||||||||||||||||||||
| November, 2015 | BC-CfE Drug Treatment Program Monthly Report (September 2015) | Drug Treatment Program | DTP Status Report | Download | |||||||||||||||||||||||
| November, 2015 | CASE STUDY - WITH SUPPORT FROM STOP HIV/AIDS TEAM, CLIENT ABLE TO REACH UNDETECTABLE VIRAL LOAD | BACKGROUNDSeek and Treat for Optimal Prevention of HIV/AIDS (STOP HIV/AIDS), a program conceptualized by the BC Centre for Excellence in HIV/AIDS (BC-CfE), aims to expand access to HIV treatment, care and medications among hard-to-reach and vulnerable populations. The STOP Outreach Team involves collaboration between nurses, health care professionals, social workers and others in order to provide for the broad spectrum of needs of their clients living with HIV. In 2012, based on its success, the BC provincial government announced $19.9 million in funding for the provincial Health Authorities towards the program’s growth. STOP Outreach Team members across the province work with vulnerable populations who have suffered trauma and lack trust in traditional health care systems. Many of their clients are simultaneously facing addiction and homelessness problems, while dealing with access to HIV treatment and care. STOP Outreach Nurses work with approximately 35-40 clients at a time. The success stories from the STOP program show the resilience that exists within vulnerable communities, as well as the importance of holistic support systems to address a broad spectrum of health, social and economic needs. This case study provides an example of a success story. A client, through the services provided by the STOP Outreach Team, was able to achieve stability and improved health. The client’s name has been changed for privacy concerns. CASE STUDY“Ross” met with the STOP Outreach Team in Vancouver while at a STOP Team HIV testing event in March 2012. At intake, the 40-year-old individual’s CD4 counts were alarmingly low at <10 and his viral load measured at over 200,000/mL. Ross struggled with severe opioid and methamphetamine IV addiction, required support with food security and housing, and faced multiple challenges to restarting his HIV antiretroviral medications (ART). The program STOP Outreach Team in Vancouver, under Vancouver Coastal Health, supported Ross in getting into three different residences and placed in several shelters. However, he faced multiple evictions and incarcerations. He was connected to the John Ruedy Immunodeficiency Clinic (IDC) at St. Paul’s Hospital. There, he re-started methadone treatment and became engaged in his medical care. He also became a member of The Dr. Peter’s Centre Day Health Program for meals and additional nursing support. During this time, the client struggled and was on and off methadone. He failed many attempts to restart HIV treatment. He required a significant amount of support to stay on methadone, as he would lose his dosing prescription on the way from the clinic to the pharmacy. He had multiple hospital admissions in relation to AIDS-related illnesses and often left the hospital against medical advice. In addition to these physical health issues, he struggled with suicidal ideation and hopelessness. He required a great deal of support to accomplish day-to-day tasks as his life was very chaotic and he was often intoxicated. A turning point finally came in 2015 when Ross became stabilized at a detox centre, after many failed attempts at detox over the years. He then restarted on ART and was transferred to a treatment centre. He eventually left the treatment centre after facing stigma and abuse due to his HIV status. The STOP staff supported and encouraged Ross to reintegrate into the centre. He returned and completed his treatment program before moving into a recovery house. Ross eventually moved to independent sober housing and began attending appointments independently. His CD4 count increased to 150 and his viral load reached undetectable levels, making likelihood of transmission negligible. At this time, Ross hopes to become a mentor to assist others in facing their addiction and in growing towards wellness. | Download | ||||||||||||||||||||||||
| November, 2015 | SAFETY UPDATE: Drug resistance emerging during therapy with dolutegravir and other integrase inhibitors | November, 2015 -At least three B.C. patients have developed new integrase resistance mutations affecting dolutegravir and/or raltegravir and elvitegravir which emerged during treatment with dolutegravir 50 mg daily plus abacavir-lamivudine. Two of the three patients also developed new resistance to lamivudine and abacavir. One patient was treatment naïve and two were treatment experienced. None had previously documented drug resistance. Two of these patients achieved virologic suppression followed by rebound, while one never achieved a viral load <40 c/mL. Drug resistance emerged within 8-12 months after starting the dolutegravir-based regimen. Incomplete medication adherence appeared to be a contributing factor. | Download | ||||||||||||||||||||||||
| November, 2015 | BC-CfE Drug Treatment Program Monthly Report (August 2015) | Drug Treatment Program | DTP Status Report | Download | |||||||||||||||||||||||
| October, 2015 | Aboriginal youth face higher rates of incarceration, new study finds |
A new study from the Urban Health Research Initiative (UHRI), a program of the BC Centre for Excellence in HIV/AIDS (BC-CfE), is the first to show street-involved Aboriginal youth in Vancouver are significantly more likely to be imprisoned than their non-Aboriginal peers. Past studies have explored risk factors involving adult Aboriginal populations; however, much less is known about incarceration among street-involved Aboriginal youth. A paper describing the study, Aboriginal street-involved youth experience elevated risk of incarceration, was recently published in the journal Public Health. It looked at data collected from 1050 youths between the ages of 14 and 26 years – one quarter identified as Aboriginal – over an eight-year period between September 2005 and May 2013 through the At–Risk Youth Study (ARYS). Over the study period, 36 per cent of participants reported having spent at least one night in detention, prison or jail in the last six months, with significantly higher rates for youth from an Aboriginal background. Researchers took into account drug use, homelessness and other factors that might place youth at greater risk of imprisonment, but still found street-involved Aboriginal youth were more likely to end up incarcerated. Study senior author Dr. Kora DeBeck, Research Scientist at UHRI and Assistant Professor in the School of Public Policy at Simon Fraser University, notes, "One possible explanation is that policing practices disproportionately target Aboriginal youth, resulting in higher rates of incarceration among this group, although further research is needed to confirm this." Aboriginal people make up four per cent of Canada's population, yet a quarter of all inmates in federal and provincial correctional facilities are Aboriginal. The study data confirm Aboriginal youth face disproportionate levels of incarceration and goes a step further in pointing to the need to investigate the possible role of discrimination in policing practices as a potential contributing factor. "Given what we know about the destructive impacts of the imprisonment of youth, in the context of this study, preventing Aboriginal youth from becoming incarcerated is crucial," added Dr. DeBeck. "It appears from our study addressing institutional discrimination may be a critical piece of the puzzle." Study authors also highlight the importance of involving Indigenous communities in addressing this complex issue. "We need solutions driven by the Aboriginal community to prevent incarceration and strengthen the health and wellness of young Aboriginal people," said study lead author, Brittany Barker, researcher with UHRI and a doctoral student at the University of British Columbia. Those working on the front lines agree that more needs to be done to support Aboriginal youth. "The disproportionate incarceration of Aboriginal youth is not new to those of us working here in the Downtown Eastside," said Michelle Fortin, Executive Director of Watari Counselling and Support Services. "It is just one of the many ways the system is not responding effectively to Aboriginal youth and the broader community at large. For example, while Aboriginal adults are overrepresented in traditional streams of the criminal justice system, they are underrepresented in diversionary measures, like community courts and mental health and addiction treatment services." | Forecast Newsletter | Download | |||||||||||||||||||||||
| September, 2015 | BC-CfE Drug Treatment Program Monthly Report (July 2015) | DTP Status Report | Download | ||||||||||||||||||||||||
| August, 2015 | HIV Monitoring Quarterly Reports, Second Quarter 2015 | STOP HIV/AIDS | Treatment as Prevention¨ | ||||||||||||||||||||||||
| August, 2015 | BC-CfE Drug Treatment Program Monthly Report (June 2015) | Drug Treatment Program | DTP Status Report | Download | |||||||||||||||||||||||
| August, 2015 | IAS 2015 shines a light on Vancouver, B.C. |
UN 90-90-90 targets and TasP strategy key to ending HIV and AIDS pandemicNearly 6,000 attendees from the global HIV community — scientists, clinicians, public health experts, community leaders, and media professionals — converged on Vancouver, British Columbia, for the 8th International AIDS Society Conference on HIV Pathogenesis, Treatment and Prevention (IAS 2015) from July 19–22, 2015. IAS 2015 welcomed delegates during a memorable opening ceremony kicked off by Larry Grant, an Elder from the Musqueam First Nation in Vancouver. The conference also welcomed several distinguished guests who included, among others, opening conference keynote speaker, Dr. Nora Volkow, Director of the National Institute on Drug Abuse (read interview on reverse side), Michel Sidibé, UNAIDS Executive Director, Ambassador Deborah Birx, MD, US Global AIDS Coordinator, Reverend Monsignor Robert J. Vitillo, head of Caritas Internationalis, Dr. Fabio Mesquita, director of the Brazilian Ministry of Health's Department of STDs, AIDS and Viral Hepatitis, and Ryan and Julie Lewis, founders of the 30/30 Project. Vancouver played host in 1996 to the International AIDS Conference where Dr. Julio Montaner and his team at the BC Centre for Excellence in HIV/AIDS (BC-CfE) introduced highly active antiretroviral therapy (HAART), ushering in the first truly effective HIV treatment. Nearly twenty years later, it is with great pride that Dr. Montaner co-chaired the IAS 2015 conference alongside IAS President Dr. Chris Beyrer, during which results of two major studies, START and HPTN 052, were unveiled. These studies confirmed what Dr. Montaner and his supporters have always believed: Treatment as Prevention (TasP) works. Starting HIV treatment immediately after diagnosis decreases plasma viral load to undetectable levels and prevents transmission of the virus to others. "Health agencies, funders, supporters, Presidents, Prime Ministers, and governments from around the world are increasingly rallying behind the TasP strategy and the UN 90-90-90 targets as the key to ending the HIV and AIDS pandemic," said Dr. Montaner, BC-CfE director. IAS 2015 saw over 500 researchers, clinicians, and civil society experts, sign the Vancouver Consensus which calls for immediate access to antiretrovirals, pre-exposure prophylaxis for those at high risk of HIV exposure, and urges rapid progress towards the implementation of new scientific evidence. The Vancouver Consensus has been endorsed by leaders of major agencies including the Global Fund to Fight AIDS, Tuberculosis and Malaria, the US President's Emergency Plan for AIDS Relief (PEPFAR) and UNAIDS, and is intended to place pressure on governments to support expanded treatment and prevention. It states in part: "All people living with HIV must have access to antiretroviral treatment upon diagnosis. Barriers to access in law, policy, stigma and bias must be confronted and dismantled. With a unified message that ending AIDS by 2030 is achievable." "Let this be the conference where the question of when to start treatment stops being a scientific question and starts being a question of finance and political will," said Dr. Beyrer. Echoing the sentiment of many in attendance, Dr. Montaner said, "Political leaders of the world, you are either with us or against us. We know the evidence and we know what needs to be done. We now have the unique opportunity to end the pandemic. It's up to you to decide whether you're going to be counted as doing the right thing." IAS 2015 AT A GLANCE
| Treatment as Prevention® | Forecast Newsletter | Download | ||||||||||||||||||||||
| August, 2015 | Dolutegravir-abacavir-lamivudine (Triumeq™) and Darunavir-cobicistat (Prezcobix™) | Formulary Addition | Dear Doctor Letter | Download | |||||||||||||||||||||||
| August, 2015 | BC-CfE Drug Treatment Program Monthly Report (May 2015) | Drug Treatment Program | DTP Status Report | Download | |||||||||||||||||||||||
| July, 2015 | Characteristics of HIV-Positive Youth in BC | Youth represent a growing number of HIV cases in Canada; according to the Public Health Agency of Canada, of 71,300 people living with HIV in Canada, approximately 25% are youth. Many struggle with access to, and retention in, HIV-care due to multiple barriers. In this volume of HIV Pulse, we explore the characteristics of HIV-positive youth in BC using the 2013 BC Centre for Excellence in HIV/AIDS Drug Treatment Program (BC-CfE DTP) data. This will assist clinicians and service providers in developing successful programming and help to guide successful and appropriate HIV-care among youth. | HIV Pulse | Download | |||||||||||||||||||||||
| June, 2015 | BC-CfE Drug Treatment Program Monthly Report (April 2015) | Drug Treatment Program | DTP Status Report | Download | |||||||||||||||||||||||
| June, 2015 | Medical marijuana: Daily cannabis use may lower HIV viral loads |
Daily cannabis use may lower HIV viral loads, suggest remarkable findings from a relatively new field of researchA researcher in the BC Centre for Excellence in HIV/AIDS (BC-CfE)'s Urban Health Research Initiative, Dr. M-J Milloy, will lead a clinical study on the possible therapeutic benefits of cannabis in the treatment of HIV/AIDS. His independent research into HIV and cannabis is supported by a $1-million gift to the University of British Columbia Faculty of Medicine by National Green Biomed Ltd. The clinical study follows previous research led by Dr. Milloy, which identified an association between marijuana use and lower viral loads (the amount of virus in a person's blood) among patients living with HIV. The BC-CfE study High-intensity cannabis use associated with lower plasma human immunodeficiency virus-1 RNA viral load among recently infected people who use injection drugs was published in Drug and Alcohol Review in March 2015 and included interviews from 88 individuals in the year following acquisition of the virus participating in the National Institutes of Health-funded study AIDS Care Cohort to evaluate Exposure to Survival Services (ACCESS). Among the 88 individuals, researchers observed significantly lower viral loads that were independently associated with people reporting at least daily cannabis use in the first year following HIV infection. The results support further investigation of the possible virological and immunological aspects of cannabinoid exposure among HIV-infected people. High levels of cannabis use are often reported by HIV-positive people attempting to ease the side effects of triple-drug therapy regimens, as well as recreationally. However, the scientific evidence-base for cannabinoids is limited, and their effect on HIV disease parameters such as viral load is largely unknown. A similar study was conducted by researchers at Louisiana State University involving chronic exposure to Tetrahydrocannabinol (THC) — the active chemical in cannabis — among rhesus macaques infected with HIV. The monkeys exposed to THC showed lower viral loads, greater retention of body mass, reduced inflammation and lengthened survival compared with those exposed to placebo. It should be noted caution is required when inferring similarities between data generated in primates and human participants. The current findings from the BC-CfE study will be evaluated in light of a growing body of evidence generated from pre-clinical settings on the structure and function of the body's cannabinoid receptor system and its possible role in HIV disease. How does marijuana affect HIV? Cannabinoids, including THC, bind to receptors expressed by cells in the nervous and immune systems. This has been shown to have beneficial immune-suppressive and anti-inflammatory properties and possibly bring down the replication of virus in the bloodstream. One experiment showed a synthetic cannabinoid receptor agonist suppressed replication of HIV in microglia, the major cell type productively infected in the human nervous system. We have long heard from our patients that they perceive health benefits from cannabis use," said Dr. Julio Montaner, BC-CfE director and head of the UBC Division of AIDS. "This gift will allow us to begin to rigorously assess whether these benefits are truly real." | Forecast Newsletter | Download | |||||||||||||||||||||||
| June, 2015 | BC-CfE Drug Treatment Program Monthly Report (March 2015) | Drug Treatment Program | DTP Status Report | Download | |||||||||||||||||||||||
| June, 2015 | HIV Monitoring Quarterly Reports, First Quarter 2015 | STOP HIV/AIDS | Treatment as Prevention¨ | ||||||||||||||||||||||||
| May, 2015 | Women and the Criminalization of HIV Non-Disclosure |
Sensational headlines entice readers but too often tell an incomplete story that only serves to perpetuate negative stereotypes. This is frequently the case when people living with HIV navigate the criminal justice system in HIV non-disclosure cases only to see their faces splashed across media channels, adding to the public fear and stigma associated with HIV/AIDS. Most prosecutions are against men, but for women living with HIV, the very justice system that was set up to protect women by criminalizing HIV non-disclosure is further victimizing them. A new Canadian Institutes for Health Reasearch-funded grant, Women, HIV and the Law Project (Co-PIs: Drs. Krüsi, Shannon) will build on the BC-CfE's Gender & Sexual Health Initiative's work with SHAWNA Project (Sexual Health and HIV/AIDS: Women's Longitudinal Needs Assessment), in partnership with the Positive Women's Network (Lead: Marcie Summers) and the Canadian HIV/AIDS Legal Network (Leads: Alison Symington, Cécile Kazatchkine). The partnership aims to review global evi dence, gaps in policy and practice, and inform research focused on the impacts of the criminalization of HIV on women's lived experiences of disclosing their HIV status in the context of intimate relationships and barriers to accessing care and support services. "There is grave concern that the current criminalization of HIV is having significant negative impacts on the daily lives of women living with HIV," says Dr. Krüsi, postdoctoral fellow with GSHI and UBC. "More empirical evidence is urgently needed, to support community and legal efforts to address this human rights concern." Canada stands out globally in its assertive approach to criminalizing HIV non-disclosure. A recent Supreme Court of Canada ruling in 2012 has resulted in an ever more restrictive legal approach to HIV non-disclosure. Using a condom or having a low or undetectable viral load is not sufficient in itself to exclude criminal liability for not revealing one's HIV status to a sexual partner. This is the case, despite the fact it is clear the risk of HIV transmission, under these circumstances, is extremely low. In the Canadian context, HIV non-disclosure is most commonly prosecuted as aggravated sexual assault. This constitutes one of the most severe charges in the Canadian Criminal Code and carries a maximum sentence of imprisonment for life and mandatory registration as a sexual offender. Melissa Medjuck, a Support Worker and Retreat Coordinator at Positive Women's Network explained, "Criminalization of HIV non-disclosure discourages people from getting tested and knowing their status because of the risk of prosecution. The reality is HIVpositive women face complex biological, economic, political, and social vulnerabilities. Criminalizing HIV non-disclosure does nothing to protect women living with HIV who, for example, are forced to stay in an abusive relationship for fear of a false allegation of HIV non-disclosure or having their status revealed." The Canadian HIV/AIDS Legal Networked further echoed this opinion in a published information sheet Women and the Criminalization of HIV Non-Disclosure writing, "Criminalizing HIV non-disclosure has been criticized as the wrong approach for addressing HIV exposure because it does not contribute to HIV prevention and in fact may undermine some public health initiatives … A gendered analysis of the current use of the criminal law with respect to HIV reveals that criminalization is a blunt, punitive and inflexible approach to HIV prevention that does little to protect women from HIV infection, violence, coercion or sexual objectification." Dramatic advances in HIV Therapy have transformed HIV infection into a chronic manageable condition. However, the criminal justice system doesn't reflect these changes. In an effort to assist those in the criminal justice system to understand and interpret the science regarding HIV, a team of six leading Canadian medical experts on HIV transmission led the development of a consensus statement Canadian Consensus Statement on HIV and its Transmission in the Context of Criminal Law to promote an evidenced-informed application of the law in Canada. The statement was developed out of a "concern that the criminal law is being used in an overly broad fashion against people living with HIV in Canada because of, in part, a poor appreciation of the scientific understanding of HIV and its transmission." | Forecast Newsletter | Download | |||||||||||||||||||||||
| May, 2015 | BC-CfE Recognized with LifeSciences BC Award for Clinical Research Excellence | Dr. Julio Montaner and members of BC-CfE staff honoured during gala event.
The BC Centre for Excellence in HIV/AIDS (BC-CfE) was honoured on April 16, 2015, during the 17th Annual LifeSciences BC Awards, for its accomplishments advancing science to treat and prevent HIV and AIDS in British Columbia and around the world. The LifeSciences event, hosted by Bob McDonald of Quirks and Quarks, celebrated the theme of "Growing Community, Collaboration and Value." "This year's theme of collaboration is fitting in light of the invaluable support the BC-CfE has received throughout the years from community partners and the provincial government," said Dr. Julio Montaner, Director of the BC-CfE. "We are greatly honoured to receive this award and recognition for the advances made in the fight against HIV and AIDS in B.C. As the BC-CfE moves forward in our research on testing, treatment and care, I believe with the continued support of our partners, we can reach an AIDS-free generation here and worldwide." Dr. Montaner was the key driver in the discovery of highly active antiretroviral therapy (HAART), a game changer in the treatment of HIV. Now the gold standard in care around the world, HAART improves St. Paul's Hospital, Vancouver, B.C. health and longevity of those living with HIV while dramatically reducing the likelihood of disease transmission. By advocating for the earlier implementation of HAART in order to curb the spread of HIV, Dr. Montaner also pioneered Treatment as Prevention (TasP). B.C. is the only province to implement the strategy, and the only one to see a consistent decline in new cases of HIV. These advances in B.C. play a major role internationally with UNAIDS aiming to eliminate AIDS by 2030 using a strategy based on principles of TasP. The UNAIDS' 90-90-90 target is 90 per cent of all individuals living with HIV diagnosed, 90 per cent of those diagnosed on sustained treatment, and 90 percent of those on treatment with a suppressed viral load. If this goal is reached, HIV will be transformed from a global epidemic to a low-level endemic disease. LifeSciences BC is a not-for-profit, non-government, industry association that supports and represents the life sciences community of B.C. Some of the Clinical Research undertaken at the BC-CfE:
| Forecast Newsletter | Download | |||||||||||||||||||||||
| April, 2015 | BC-CfE Drug Treatment Program Monthly Report (February 2015) | Drug Treatment Program | DTP Status Report | Download | |||||||||||||||||||||||
| March, 2015 | Dr. Julio Montaner holds discussions with senior Vatican officials regarding Treatment as Prevention | Catholic Church a strong contributor to the fight against HIV and AIDS around the world
Director of the BC Centre for Excellence in HIV/AIDS (BC-CfE), Dr. Julio Montaner, was met with a substantial level of interest as he brought to the Vatican examples of achievements in British Columbia through Treatment as Prevention (TasP). "It's not often that you get a thumbs up from His Holiness Pope Francis," said Dr. Montaner. The concept of TasP was pioneered at the BC-CfE, led by Dr. Montaner. Its implementation in BC, with the strong support of the provincial government, has resulted in dramatically reduced HIV morbidity and mortality, as well as a steep decline in new HIV cases. "It is very promising the Roman Catholic Church is expressing interest in Treatment as Prevention," Dr. Montaner said. "The Church, with all its infrastructure and outreach, would be a fantastic partner to help expand TasP globally." The Catholic Church has previously expressed the need to treat those affected by HIV and AIDS with compassion and dignity. Through its global service and St. Paul's Hospital, Vancouver, B.C. charity arm, Caritas Internationalis, the church aims to provide access to antiretrovirals to those living with HIV worldwide currently not reached by treatment. The Vatican estimates Catholic Church-related organizations provide approximately one quarter of all HIV treatment, care and support throughout the world, particularly in resource limited settings where HIV rates are increasing. On his visit in early March, Dr. Montaner met with a number of senior Vatican officials, including Ghanian Cardinal Peter Turkson, President of the Pontifical Council for Justice and Peace, and his colleague Fr. Michael F. Czerny; and Msgr. Father Jean-Marie Mate Musivi Mupendawatu, Secretary of the Pontifical Council for Pastoral Assistance to Health Care Workers, and his colleague Sister Juliana Resende; as well as Msgr. Guillermo Karcher of the Vatican State Secretariat. Some statistics about the global HIV epidemic:
| Treatment as Prevention® | Forecast Newsletter | Download | ||||||||||||||||||||||
| March, 2015 | BC-CfE Drug Treatment Program Monthly Report (January 2015) | Drug Treatment Program | DTP Status Report | Download | |||||||||||||||||||||||
| March, 2015 | HIV Monitoring Quarterly Reports, Fourth Quarter 2014 | STOP HIV/AIDS | Treatment as Prevention¨ | ||||||||||||||||||||||||
| March, 2015 | BC-CfE Drug Treatment Program Monthly Report (December2014) | Drug Treatment Program | DTP Status Report | Download | |||||||||||||||||||||||
| February, 2015 | The end of AIDS? New BC-CfE study says it's possible | Is talk of "ending AIDS" just hyperbole, or is this a realistic goal for the research and medical communities?
A recent study in The Lancet HIV journal, authored by researchers at the BC Centre for Excellence in HIV/AIDS (BC-CfE), is adding valuable evidence to a concept long-held by researchers in B.C. The research indicates AIDS and related deaths could not only be controlled, but virtually eliminated, through expanded access to highly active antiretroviral therapy (HAART), evidence-based treatment guidelines, and systems to ensure timely HIV diagnosis and HAART initiation. This is an approach that could be applied internationally. The study called AIDS incidence and AIDS-related mortality in British Columbia, Canada, between 1981 and 2013: a retrospective study points to steep declines in rates of AIDS-related mortality in B.C. since the mid 90s with the introduction of HAART. There was a further decline in 2006 when the concept of Treatment as Prevention was pioneered and implemented. At the peak of the epidemic in 1994, 696 cases of AIDS were reported. By 2013, the number had fallen to 84 – nearly an 88 per cent decline! "The research indicates that timely and expanded access to HAART treatment can transform AIDS from an epidemic to an endemic disease," says Dr. Viviane Dias Lima (PhD.), lead author of the study and BC-CfE Research Scientist and Senior Statistician. "Having the study published in The Lancet HIV journal gives further weight to the case for the expansion of HAART treatment and TasP initiatives, both within Canada and worldwide." As Treatments Evolve, Numbers DropThe study analyzed data from individuals living with HIV aged 19 years or older, who have ever accessed HAART in B.C. Researchers saw significant downward trends in AIDS deaths as treatment guidelines evolved towards more immediate and sustained initiation of HAART. Among people living with HIV in British Columbia, the study finds:
Researchers also found, since the introduction of HAART, vertical transmission of HIV – from a mother to an infant –has been virtually eliminated in B.C. In addition, HIV positive individuals are now living longer and healthier lives, and becoming part of an aging population. "They are no longer dying of illnesses due to AIDS, but of heart disease, cancer and respiratory illnesses, just like everyone else," Dr. Lima says in an article published in The Globe and Mail on the study's findings. She continued,"These data warrant further exploration into the other causes of illness and death in individuals living with HIV/AIDS. As these individuals age, we are faced with today's challenge of better understanding how to improve their overall health outcomes." The Role of Treatment as PreventionBC-CfE Director Dr. Julio Montaner considers TasP the key to eliminating the pandemic. "Treatment as Prevention provides a road map for global HIV/AIDS control, and is based on the concept that early diagnosis and antiretroviral treatment improves patient longevity and quality of life, while dramatically decreasing the likelihood of spread of HIV," he says. The proposed UNAIDS 90-90-90 target calls for 90% of people living with HIV knowing their HIV status by 2020, 90% of them receiving sustained HAART, and 90% of them maintaining an undetectable viral load. Meeting the proposed target by 2020 will maximize the effectiveness of existing tools to virtually eliminate progression to AIDS, premature death and HIV transmission, and thereby transform the HIV/AIDS pandemic into a low level sporadic endemic by 2030. The study was co-authored by Lillian Lourenço, Benita Yip, Dr. Robert S. Hogg, Dr. Peter Phillips, and Dr. Julio S.G. Montaner, and appears in the February Edition of The Lancet HIV. | Forecast Newsletter | Download | |||||||||||||||||||||||
| February, 2015 | BC-CfE Drug Treatment Program Monthly Report (November2014) | Drug Treatment Program | DTP Status Report | Download | |||||||||||||||||||||||
| January, 2015 | Characteristics of ARV-Prescribing Physicians in BC | Disparities in access to HIV care and treatment, including access to antiretroviral (ARV)-prescribing physicians, exist in Canada. This HIV Pulse measures the number of ARV-prescribing physicians by region in BC and outlines their characteristics. Profiled here are those who prescribed ARVs between January 1, 2013 – December 31, 2013, based on the data from the BC Centre for Excellence in HIV/AIDS Drug Treatment Program. | HIV Pulse | Download | |||||||||||||||||||||||
| December, 2014 | World AIDS Day letter: Made-in-Canada AIDS strategy a blueprint for targeted disease elimination | Proven model a cost-effective strategy to potentially eliminate other diseases such as hepatitis, writes Dr. Julio Montaner
The national AIDS strategy is nearly a decade old and desperately needs updating. In B.C., our Treatment as Prevention (TasP) strategy has been successful in dramatically decreasing new cases of HIV and morbidity and mortality. It is now providing the road map for global elimination of the HIV pandemic. While this made-in- B.C. strategy is now embraced globally, this is not the case in the rest of Canada. Nearly 20 years ago, the BC Centre for Excellence in HIV/AIDS (BC-CfE) created triple drug therapy, the new highly active antiretroviral therapy (HAART) regimen. HAART turned HIV and AIDS from a death sentence into a chronic manageable condition. A decade later, we pioneered and demonstrated the very same HAART regimen could dramatically reduce the likelihood of HIV transmission – this strategy we named Treatment as Prevention. Simply put: we now have definitive evidence a person infected with HIV with undetectable levels of HIV virus, as a result of HAART use, has little to no chance of developing AIDS and transmitting HIV. In 2006, this led us to advocate for the expansion of HAART coverage, under the banner of Treatment as Prevention, to prevent illness, death and secondarily, new HIV infections. Of note, the TasP strategy not only saves lives, it is cost-averting. The TasP strategy involves widespread HIV testing and immediate facilitated access to HAART for all eligible residents of B.C. In B.C., we have decreased progression to AIDS and related premature deaths by over 95% since we began treating with HAART, and decreased the spread of new HIV infections by over 66%. The strategy has been so successful, the province's dedicated HIV/ AIDS ward – which opened in 1997 at St. Paul's Hospital in Vancouver – was re-purposed earlier this year due to the significant decline in new cases of AIDS in the province. To date, B.C. is the only province in Canada that has seen consistent declines in new infections over the last decade. The rate of new infections in B.C. has gone from the highest per capita to one of the lowest in the country. Sadly, an estimated 77,000 Canadians are currently living with HIV, representing an increase of 5,700 people (8%) since 2011. An estimated 18,500 people living with HIV in Canada remain undiagnosed – and unaware of their HIV status. The burden of HIV is particularly felt within our Aboriginal communities. The end of the HIV/AIDS pandemic is within reach. Countries around the world are rallying behind the made-in-B.C.-and-Canada TasP strategy. We can only hope the rest of Canada will follow suit. Importantly, we are proud our made-in-Canada TasP strategy has provided the foundation for the United Nations' (UN) new global plan to end the AIDS epidemic by 2030. Announced in September, the UN plan, known as the "90-90-90 target" of which I was the architect proposes by 2020:
This plan is ambitious, but achievable. Indeed, a growing number of jurisdictions around the world – both in the north and south – have shown that one or more of the three components of the proposed targets can be achieved. The problem is, it's not always the same player achieving the best performance. Yet, we can learn from each other and succeed in meeting all three components of the target. | Treatment as Prevention® | Forecast Newsletter | Download | ||||||||||||||||||||||
| December, 2014 | Longest supporter of Treatment as Prevention hails strategy for health outcomes and cost-effectiveness | ‘We know by increasing community capacity, we can improve patient care and efficiency for our investments,' says health minister
The government is the longest adopter of the Treatment as Prevention (TasP) strategy and has recognized Dr. Julio Montaner for the success of significantly improving health outcomes and providing a sustainable model for health-care delivery. The B.C. government recognized Dr. Julio Montaner for his pioneering work in developing the TasP strategy at the BC Centre for Excellence in HIV/AIDS. TasP has dramatically reduced rates of new HIV transmission, significantly improved the quality of life for HIV-positive individuals and provided a model that is cost averting. BC-CfE Director, Dr. Julio Montaner accepted his Certificate of Appreciation from provincial Minister of Health, Terry Lake at a special event at the Legislature in Victoria, B.C. Lake commended Dr. Montaner for his lifelong commitment to providing care and treatment to HIV positive individuals, including pioneering Highly Active Antiretroviral Therapy (HAART) and TasP. Minister Lake made the address to sitting members of the Legislative Assembly. In 2009, the B.C. government announced the launching of a four-year pilot project of the made-in- B.C. TasP strategy, called STOP HIV/AIDS. Before the pilot had wrapped up, based on its early success, the government announced in 2013 a province-wide expansion of the STOP HIV/AIDS program. Largely due to universal access to HIV antiretroviral medications as part of TasP, B.C. has seen HIV-related morbidity and mortality decline by over 95% since 1995, and a decrease of greater than 66% of new HIV infections. In a speech, Lake highlighted emerging new data shows TasP will help "to improve the sustainability of our health care system." "Each year, we spend over $100 million to ensure HIV medications are free to all people who wish to be on treatment. We know by increasing community capacity, we can improve patient care and efficiency for our investments," said Lake. "Furthermore, the additional investment aimed to enhance testing, treatment and support will become cost-adverting by 2017 and it is estimated to accrue $48 million in savings by 2035. "It is perhaps not surprising then, that B.C.'s strategy is influencing the international community." The TasP strategy has been adopted by China, France, Brazil, Spain, Panama, Argentina, Swaziland, the Australian state of Queensland, and parts of the United States – to name a few. In September 2014, the United Nations endorsed the TasP model in its launch of the 90-90-90 strategy, a plan for reducing the global AIDS pandemic by at least 90% of its 2010 rate by 2030. By 2020, UNAIDS' goals are that 90% of all people living with HIV will know their status, 90% of all people diagnosed with HIV infection will receive sustained antiretroviral therapy, and 90% of all people receiving antiretroviral therapy will have viral suppression. Dr. Montaner, as UNAIDS Special Advisor on HIV Therapeutics, is the architect of the 90-90-90 strategy. "It is an honour to be recognized by our B.C. government but much work remains," said Dr. Montaner. "In particular, B.C. is the only province in Canada consistently seeing a decline in new HIV infections while HIV infections continue to increase nationally." "It is important to recognize the distance we still have to go in order to reach the end of HIV and AIDS. We must continue to build and strengthen accessible pathways to treatment, prevention, care and support for all. While other nations are striding forward based on the strategy pioneered by B.C., Canada is without a national strategy. Further, we need to reflect on the lessons learned in the fight against HIV/AIDS and expand the strategy to other contagious diseases as a means to promote targeted disease elimination and thus contribute to the sustainability of our health care." | Forecast Newsletter | Download | |||||||||||||||||||||||
| November, 2014 | HIV Monitoring Quarterly Reports, Third Quarter 2014 | STOP HIV/AIDS | Treatment as Prevention¨ | ||||||||||||||||||||||||
| November, 2014 | Dr. Montaner to be inducted into Canadian Medical Hall of Fame for international leadership in combatting HIV/AIDS | One of Canada's ‘medical heroes' for his contribution to health in Canada and the world, says organization's chair
BC-CfE director Dr. Julio Montaner is to be inducted into the Canadian Medical Hall of Fame for his international leadership and clinical advancements in combatting HIV/AIDS. The Canadian Medical Hall of Fame is dedicated to "celebrating the accomplishments of medical heroes." Dr. Montaner, Director of the BC-CfE and past president of the International AIDS Society, will join the company of notable Canadians who have made their mark in improving global health outcomes, including Drs. Fred Banting, Norman Bethune, Charles Best and Michael Smith. "The Canadian Medical Hall of Fame is proud to count Dr. Julio Montaner among Canada's illustrious medical heroes," says Dr. Jean Gray, chair of The Canadian Medical Hall of Fame. "His contribution to health in Canada and the world is well documented and a wonderful example of the kind of passion, diligence and innovative thinking displayed by our laureates." The Canadian Medical Hall of Fame laureates are individuals whose outstanding contributions to medicine and the health sciences have led to extraordinary improvements in human health. Laureates are considered pioneers in their field, role models to young Canadians to pursue careers in health science, as well as a source of inspiration for all Canadians for their important contribution to global health. Of special note, Dr. Montaner joins one of his mentors as a laureate, the namesake of The James Hogg Research Centre at St. Paul's Hospital. Then director of UBC-St. Paul's Pulmonary Research Laboratory, Dr. Hogg spoke at a medical conference that Dr. Montaner was attending in Uruguay in 1979. Dr. Hogg offered the young Argentinian student a fellowship at St. Paul's Hospital in Vancouver. Dr. Montaner was in B.C. by the summer of 1981, became the hospital's chief resident in 1984, and took the position of director of AIDS research in 1985. Dr. Montaner was recognized for a career dedicated to the care and management of HIV infected individuals and those at risk of HIV, creating advancements in the treatment and prevention of HIV and AIDS. "I am very honoured and humbled to be chosen for this award," says Dr. Montaner. "I am convinced with the help of my colleagues, our government and the public, we can bring this epidemic to its knees, not just in B.C. but worldwide. Indeed, we are on our way in B.C. and our strategy is the model the rest of the world is adopting. I share this acknowledgment with my colleagues at the BC Centre for Excellence in HIV/AIDS, whose contributions helped to create and refine new approaches to HIV and AIDS treatment. Our success in reducing new HIV infections, reducing morbidity and mortality would not be possible without them, and the support of our BC government, the University of British Columbia, Providence Health Care Research Institute, and Providence Health Care. All are partners in the fight against HIV and AIDS." In 1996, Dr. Montaner led the research team that reported the success of triple drug therapy at the International AIDS Conference in Vancouver. Triple drug therapy (also known as highly active antiretroviral therapy - HAART) and viral load monitoring became the new international standard of care. The New York Times called triple drug therapy a "clear watershed in the treatment of AIDS." A decade later, Dr. Montaner's presentation of HAART as a means to not only treat a patient but to prevent transmission made headlines at the 2006 International AIDS Conference in Toronto. The successful implementation of the Treatment as Prevention strategy (TasP) in B.C. was heralded as the "scientific breakthrough of the year" by Science (2011); one of the top breakthroughs by Time (2011) and Reader's Digest (2012). | Forecast Newsletter | Download | |||||||||||||||||||||||
| October, 2014 | Made-in-B.C. treatment strategy adopted by United Nations to combat HIV/AIDS internationally | UN General Assembly told 90-90-90 plan can end AIDS as an epidemic by 2030 if ‘achievable' targets met
The United Nations (UN) unveiled an ambitious new global plan to end the AIDS epidemic by 2030. The plan embraces the made-in-BC Treatment as Prevention (TasP) strategy pioneered by Dr. Julio Montaner and the BC Centre for Excellence in HIV/AIDS (BC-CfE). The plan was announced on September 25 by Jan Eliasson, Deputy Secretary-General of the UN, to the UN General Assembly in New York and is supported by UNAIDS Executive Director and UN Under-Secretary-General Michel Sidibé. The UNAIDS plan is based on modelling that demonstrates that achieving new targets by 2020 will spell the end of AIDS as an epidemic by 2030. A key pillar of the plan embraces HIV treatment as a means to prevent new infections. One of the most influential medical journals and a former UNAIDS special envoy both credit Dr. Julio Montaner for his contributions in authoring the TasP strategy that is the backbone of the global plan. The UNAIDS plan, titled "Ambitious treatment targets: Writing the final chapter of the AIDS epidemic" is based on three targets:
"As these new targets reflect, efforts will be needed to explain to individuals and communities that antiretroviral therapy not only keeps people alive, but also prevents further transmission of the virus to sexual partners of people living with HIV and from mother to child," says the plan, popularly dubbed "90-90-90." Dr. Montaner formally introduced TasP in 2006 at the International AIDS Society conference in Toronto. The TasP strategy involves widespread HIV testing and immediate offer of highly active antiretroviral therapy (HAART) to medically eligible individuals. Early engagement and sustained treatment has been shown to virtually eliminate progression of HIV disease to AIDS and premature death, and at the same time tstop transmission of the virus. B.C. has virtually eliminated AIDS and markedly decreased the spread of new HIV infections. The B.C. strategy has been so successful that the province's dedicated HIV/AIDS Ward -- which opened in 1997 at St. Paul's Hospital in Vancouver -- was recently re-purposed because of the significant decline in new cases of AIDS in the province. In making the global case for HIV treatment preventing new infections, the UNAIDS proposal cites BC-CfE research in the B.C. setting. "These findings are similar to those reported in the Canadian province of British Columbia, where every 1% increase in the number of people with suppressed virus has been associated with a 1.2% reduction in estimated HIV incidence." Dr. Montaner was the lead author of the new UNAIDS plan, which was first proposed at the 20th International AIDS Conference in Melbourne, Australia. Montaner, Sidibé, and the late Dr. Joep Lange fine-tuned the plan's final details in Geneva days before the conference. "This plan is realistic and all the targets are achievable. We found a growing number of countries – both in northern and southern hemispheres – that are either on track to achieve 90–90–90 or have approached, met or exceeded one or more of these targets," says Montaner. "The problem is, it's not always the same player achieving the best performance. However, we can learn from each other. This plan sends a clear signal we need to invest in the best possible treatment for all." In his remarks to the UN General Assembly, U.S. Secretary of State John Kerry commended those who have shown "the commitment to helping to write a new chapter in this fight against AIDS." Stephen Lewis, the former UN secretary general's special envoy for HIV/AIDS, praised Dr. Montaner for TasP, which has increasingly been adopted by governments and non-profit agencies around the world. China, Brazil, Spain, France, Panama, Australia's State of Queensland – as well as the U.S. cities of New York, San Francisco and Washington D.C. – have already adopted TasP. "I don't think Canadians understand the impact of what Julio has done," Lewis said in Georgia Straight, a Vancouver weekly newspaper. In an editorial on the milestone announcement of 90-90-90 in Melbourne, The Lancet makes first mention of Dr. Montaner's groundbreaking work. In "Ending the AIDS Epidemic," editor-in-chief Richard Horton writes there are papers The Lancet is "immensely grateful" to have published. "One such Lancet paper is Julio Montaner's truly landmark 2006 viewpoint entitled, rather modestly now looking back, ‘The case for expanding access to HAART to curb the growth of the HIV epidemic.' The idea of treatment as prevention was born," writes Horton. Based on the consolidated guidelines recently put forward by the World Health Organization (WHO) to initiate HIV treatment sooner in order to save more lives and prevent more infections, 90-90-90 replaces Treatment 2015, the UNAIDS campaign aimed at reaching 15 million people with HAART by 2015.Global efforts to increase the number of people getting access to life-saving HAART have advanced quickly, with 12.9 million people now receiving HIV treatment compared with 5.2 million in 2009, according to UNAIDS data. "We're almost there in reaching the 2015 goal," says Montaner. "In conversations about ‘what next,' we convinced ourselves that we needed not only a very aggressive new target, but a better one. We wanted a target that was comprehensive and no longer uni-dimensional. We wanted to incorporate a cascade of care and virological suppression so we ensure people get durable, sustainable and best-available treatment for their benefit, and ultimately transform the HIV/AIDS pandemic into a low endemic sporadic disease by 2030." Health Ministers for both South Africa and Brazil, two countries with high HIV rates, have already endorsed the UNAIDS plan. | Forecast Newsletter | Download | |||||||||||||||||||||||
| September, 2014 | Australian state joins growing list of international jurisdictions embracing made-in-BC model | Queensland signs Memorandum of Understanding to adopt Treatment as Prevention as strategy to combat HIV/AIDS
The BC Centre for Excellence in HIV/AIDS (BC-CfE) has signed a Memorandum of Understanding (MOU) that will see Queensland, Australia, embrace the made-in-B.C. HIV Treatment as Prevention (TasP) strategy. BC-CfE, the Government of Queensland and HIV Foundation Queensland (HIVFQ) signed the agreement at the 20th International AIDS Conference in Melbourne. The partnership formalizes a collaboration aimed at supporting HIV positive individuals and at-risk populations in Queensland and B.C. The Australian state will formally adopt TasP, a strategy pioneered by the BC-CfE. "We are very excited to be collaborating with Queensland in implementing the Treatment as Prevention strategy," says Dr. Julio Montaner, director, BC-CfE. "This model is based on scientific evidence. We know from the success we've had with this strategy that it holds the promise of eliminating HIV and AIDS in our lifetime." Queensland is the latest international jurisdiction to implement TasP. Panama, China, France, Spain and Brazil – as well as the U.S. cities of New York, San Francisco and Washington D.C. – have already adopted TasP. The TasP strategy involves widespread HIV testing and immediate offer of highly active antiretroviral therapy (HAART) to medically eligible individuals. Early engagement and sustained treatment has been shown to virtually eliminate progression of the disease to AIDS and premature death, and simultaneously stop transmission of the virus. Dr. Montaner formally introduced TasP in 2006 at the Toronto International AIDS Society conference. B.C. has virtually eliminated AIDS and markedly decreased the spread of new HIV infections. The B.C. strategy has been so successful, the province's dedicated HIV/AIDS Ward -- which opened in 1997 at St. Paul's hospital in Vancouver -- was recently re-profiled because new cases of AIDS have declined significantly. Queensland Minister for Health, Lawrence Springborg, said the partnership signified a milestone for HIV in Queensland that would deliver many positive outcomes. "Queensland is the first Australian jurisdiction to enter into such a partnership to develop an HIV Treatment as Prevention strategy with leading international experts," said Sprinborg. "This provides Queensland with the opportunity to lead the development, implementation and evaluation of TasP in Australia. We believe this will have significant impacts on national and international efforts working towards the virtual elimination of HIV." HIVFQ chair Dr. Darren Russell stressed the strategy allows for HAART to be offered immediately to people living with HIV who are eligible and want to commence treatment. "Getting people onto HIV treatment early also decreases HIV transmission and new cases of HIV," Russell said in an interview with Australian newspaper Star Observer. "As part of the strategy, we are committed to achieving increased treatment uptake. We are aiming for 90% of people living with HIV to be on treatment. The foundation is also really keen to work with partners and key stakeholders to promote the TasP strategy in Queensland to ensure we achieve the best possible outcomes." The BC-CfE and its Queensland partners will work jointly to respectively improve the health of British Columbians and Queenslanders through sharing cost-effective research, therapeutic protocols and tools, and programs for the treatment of HIV and AIDS. The partnership aims to protect and improve the health of people by eliminating HIV/AIDS through science, policy, partnership, and evidence-based public health action. | Forecast Newsletter | Download | |||||||||||||||||||||||
| August, 2014 | HIV Monitoring Quarterly Reports, Second Quarter 2014 | STOP HIV/AIDS | Treatment as Prevention¨ | ||||||||||||||||||||||||
| July, 2014 | New federal legislation will threaten health and safety of sex workers: research findings | Study reveals continued policing of clients recreates the same harms as Canada's current criminalized model
New legislation introduced by the federal government earlier this month threatens the health and safety of sex workers, according to researchers at the BC Centre for Excellence in HIV/AIDS (BC-CfE). Federal Justice Minister Peter MacKay tabled the Conservative government's new prostitution legislation, The Protection of Communities and Exploited Persons Act, which proposes criminalizing the purchase of sex, communicating for the purpose of selling sex, gaining material benefit from sex work, and advertising sexual services. The proposed legislation was announced shortly after a new study was published by researchers of BC-CfE's Gender and Sexual Health Initiative (GSHI). The study, published in BMJ Open, one of the top peer-reviewed global health journals, found criminalizing clients endangers the health and safety of the most marginalized sex workers. Sex workers were very clear, says Andrea Krusi, lead author of the BMJ Open paper and senior doctoral trainee. "Where clients continue to be targets of police, sex workers' ability to protect themselves from violence and abuse or access police protections is severely limited," says Krusi Researchers conducted in-depth interviews with 31 street-based sex workers in Vancouver between January and November 2013 to examine sex workers' experiences and negotiation of safety and health following the implementation of new Vancouver Police Department (VPD) enforcement guidelines introduced in January 2013. The new VPD policy prioritizes sex workers' safety over arrest, while continuing to focus enforcement on clients and third parties. The approach of criminalizing clients, but not sex workers, is often referred to as the "Swedish" or "Nordic" model, and is similar to the approach proposed in the new federal legislation. "The findings clearly show that criminalization of clients in Canada risks recreating the same devastating harms to the health, safety and human rights of sex workers as the last two decades of missing and murdered women," says Dr. Kate Shannon, senior author of the BMJ Open report and GSHI director. Following the new VPD enforcement policy, sex work-related arrests in Vancouver increased from 47 in 2012 to 71 in 2013. Despite the expressed commitment to sex workers' safety, the research suggests there was no decrease in rates of work-related physical or sexual violence after policy implementation, with 24% of 275 street-based sex workers in 2012 experiencing violence compared to 25% of 236 in 2013. Despite the new VPD policy shift to clients, sex workers in the study describe how the continued policing of clients recreated the same harms as the current criminalized model in Canada by severely limiting sex workers' control over their health and safety. "Harassing the clients is exactly the same as harassing the women," said Jasmine, a sex worker, in the BMJ Open report. "You harass the clients and you are in exactly the same spot you were before. I'm staying on the streets. I'm in jeopardy of getting raped, hurt." A second report and legal analysis of the BMJ Open research was also published by GSHI, Pivot Legal Society and Sex Workers United Against Violence (SWUAV). The report provides a legal analysis of the evidence from the BMJ Open research, as well as from Sweden and Norway, regarding the impacts of criminalization of clients on sex workers' safety. The research concludes that given the harms created by this model of criminalization and the reasoning from court decision Canada v. Bedford, there is a strong case to be made that a law prohibiting the purchase of sexual services would violate sex workers' constitutional right to security of the person and should be struck down. | Sex Work | Forecast Newsletter | Download | ||||||||||||||||||||||
| June, 2014 | B.C. Premier Christy Clark and Dr. Julio Montaner, director for the BC Centre for Excellence in HIV/AIDS, at historic announcement | Global landmark: Vancouver first city in the world to repurpose its AIDS wardSignificant decrease in AIDS cases at St. Paul's Hospital leads to shift in health care priorities.
The dramatic decline in the number of cases of AIDS, the most serious outcome of untreated HIV infection, has prompted St. Paul's Hospital to repurpose its AIDS ward, making Vancouver the first city in the world to achieve this distinction. A packed room of community members and hospital staff gathered on May 27 as B.C. Premier Christy Clark – along with Michel Sidibé, United Nations (UN) undersecretary and executive director for the Joint UN Programme on HIV/AIDS (UNAIDS), Dr. Julio Montaner, director for the BC Centre for Excellence in HIV/AIDS (BC-CfE), B.C. Health Minister Terry Lake and Vancouver artist Tiko Kerr– announced ward 10C at St. Paul's Hospital will no longer be used as a dedicated AIDS ward. "This is a proud day for British Columbians as we mark another milestone in our leadership in the fight against HIV/AIDS," said Premier Clark. "Thanks to the dedicated efforts of the community, those at the BC Centre for Excellence in HIV/AIDS and health professionals across the province, a ward that once served those dying from AIDS, now supports those living with HIV." Ward 10C at St. Paul's Hospital in downtown Vancouver was originally opened as an AIDS ward in February 1997 during the peak of the HIV and AIDS epidemic in the city, when approximately one person was dying of AIDS every day. In B.C. earlier diagnosis of HIV, along with advances in treatment and care, has resulted in a significant decrease in cases of AIDS. "There was a time when there weren't enough beds to care for the numbers of people living with HIV," said Sidibé. "The pioneering work of Dr. Montaner and the leadership of British Columbia have helped to ensure that people living with HIV live longer, healthier lives and as a result the AIDS ward in B.C. is being refocused. This is an important milestone towards ending the AIDS epidemic," he added. British Columbia is recognized as a world-leader in the fight against HIV/AIDS. The Treatment as Prevention strategy, pioneered by the BC-CfE, has been adopted by China, France, Brazil, Spain, and Panama. It has been endorsed by UNAIDS and implemented in numerous cities in the United States. The province has taken an aggressive approach to addressing the HIV epidemic through programs such as the Seek and Treat for Optimal Prevention of HIV/AIDS (STOP HIV/AIDS) pilot. Beginning last year, the B.C. government provided $19.9 million in annual funding to expand this program across the province. "British Columbia's dedication to the fight against HIV/AIDS has meant that we have reduced AIDS cases in Vancouver by over 80% since 1996," said Lake. "With continued focus on providing care, treatment and support for those living with HIV and related diseases, more British Columbians will live longer, healthier lives." Sidibé praised Premier Clark for her government's HIV and AIDS response in B.C. and internationally. And he reminded the audience that nearly 18 million people in low- and middle-income countries still do not have access to antiretroviral treatment. "Only with global solidarity, can we ensure that no-one is left behind," said Sidibé. Patients living with HIV will continue to receive world-leading treatment and care at St. Paul's Hospital and at other clinics throughout the province. The focus of the ward will include treatment related to addictions such as various bacterial and viral infections like chronic hepatitis. "It was not that long ago that HIV/AIDS was a death sentence and those who came to this ward at St. Paul's were here to die," said Dr. Montaner. "Today, ward 10C will provide treatment, support and care for those living with HIV-related issues. We have worked hard to make this day happen and I commend everyone who has supported our efforts." | Forecast Newsletter | Download | |||||||||||||||||||||||
| June, 2014 | Drug Treatment Program Enrolment and Prescription Request Forms | Notice of Change to Forms | Dear Doctor Letter | Download | |||||||||||||||||||||||
| June, 2014 | The Case against Criminalizing the Purchase of Sex in Canada | On December 20, 2013, the Supreme Court of Canada rendered a landmark decision that substantially reshaped Canada’s legal framework regarding adult prostitution. The case of Bedford v. Canada resulted in the striking down of three provisions of the Criminal Code: the communication, bawdy-house and living on the avails laws. The Court found that these three provisions violate section 7 of the Charter of Rights and Freedoms (the “Charter”) given their negative impact on sex workers’ security of the person. The declaration of invalidity of the laws did not, however, take effect immediately. The Court gave the government one year to contemplate whether new prostitution laws should be enacted. | Download | ||||||||||||||||||||||||
| May, 2014 | HIV Monitoring Quarterly Reports, First Quarter 2014 | STOP HIV/AIDS | Treatment as Prevention¨ | ||||||||||||||||||||||||
| May, 2014 | Roundtable talk focuses on improving HIV treatment access among vulnerable populations | Research at International HIV Treatment as Prevention Workshop highlights need to target key affected populations and address stigma
Hundreds of leading HIV scientists from around the world gathered in Vancouver this April to share the results of their latest research on HIV prevention at the 4th International HIV Treatment as Prevention Workshop. Previous workshops have focused on whether expanding treatment access is the most effective strategy to fight the global epidemic of HIV and AIDS. At this year's workshop, researchers were ready to discuss best approaches to implementing the strategy. "Finally there is a consensus emerging that the science clearly demonstrates treatment is highly effective in stopping transmission in all contexts," said Dr. Julio Montaner, director of the BC Centre for Excellence in HIV/AIDS (BC-CfE) and co-chair of the workshop. He argued for being more efficient by identifying who should be treated and when. Specifically, vulnerable populations such as women, children, and men who have sex with men remain at-risk as a result of ongoing discrimination in many countries, limiting their access to life-saving treatment and care. "Progress is very uneven," said Dr. Luiz Loures, UNAIDS Deputy Executive Director. "The likelihood of access to treatment and prevention is much lower for certain key minorities such as LGBTI [lesbian, gay, bisexual, transgender, and intersex], prisoners, migrants, sex workers, persons who injects drugs, and young women in Sub-Saharan Africa today." Dr. Loures' remarks were made during the opening session of the four-day workshop. The roundtable session gathered high-level delegates from across the globe with the intention of bringing together key national decision-makers and pivotal international partners to explore the importance of new HIV treatment strategies and targets. The session, co-hosted by UNAIDS and the BC-CfE, comprised representatives from the three key groups influencing HIV strategy—politicians, scientists and community—and set the agenda for the rest of the workshop. "We should be setting one goal, and one goal only: to end HIV as an epidemic," said Dr. Mark Dybul, Executive Director of the Global Fund to Fight AIDS, Tuberculosis & Malaria. During his presentation, he spoke of the need to move away from generalized targets and instead focus HIV treatment and prevention efforts on key affected populations, the people most marginalized and made vulnerable as a result of societal determinants. "We have to bring the epidemic under control within all of these affected populations," Dr. Dybul said. "If we don't, we will continue to leave people behind." Evidence presented at the workshop supported his argument. In Vietnam, for example, hot spotting—targeting those regions where the HIV epidemic is most concentrated—has proven effective in reducing HIV transmission, according to research presented by Dr. Brian Williams of the South African Centre for Epidemiological Modelling and Analysis (SACEMA). Efficiency, he said, dictates HIV testing where the prevalence is highest. Promising research results suggested the end of AIDS is within reach. However, conference delegates were cautioned that success is not guaranteed, and ending AIDS will demand new ways of operating. Eliminating stigma and discrimination—and engaging and giving voice to communities—may be the only way forward to ending the HIV epidemic. Reaching those who are being missed by current treatment efforts is in opposition to punitive legal and policy frameworks that deter individuals from seeking the services they need. During the opening session, it was noted that 77 countries criminalize same-sex relationships, and that children are substantially less likely than adults to receive HIV treatment when they are eligible. "We need to understand and act on local epidemics," said Dr. Loures. "We need to understand how they operate and understand how we can respond to them. This is much easier to do if you are bringing services closer to communities and to people." | Forecast Newsletter | Download | |||||||||||||||||||||||
| April, 2014 | Support base grows for advancing Treatment as Prevention as the global strategy | Vatican, Panama and formalized UNAIDS agreement add further momentum to saving lives, preventing infections and saving money
Several recent international endorsements and agreements underline the growing universal acceptance of the made-in-BC Treatment as Prevention Strategy. Support from the Vatican, formalization of an agreement with the Joint United Nations Programme on HIV/AIDS (UNAIDS), and a Memorandum of Understanding (MOU) signed by Panama highlight the growing support base for the strategy pioneered by BC Centre for Excellence in HIV/AIDS (BC-CfE). At the opening of a Caritas Internationalis and UNAIDS co-organized consultation at the Vatican in Rome last month, Archbishop Zygmunt Zimowski favoured expanding access to HIV treatment worldwide. Speaking to an audience of international HIV/AIDS researchers and policymakers, the archbishop called for the implementation of Treatment 2015, the framework developed by UNAIDS to expand access to life-saving HIV treatment to 15 million people living with the disease. "In all cases, (we must) place at the centre of all our health care interventions with the people (living with HIV), their dignity, their needs and rights," said Zimowski, who also serves as president of the Vatican's Pontifical Council for Health Pastoral Care. He later repeated the appeal made by Pope Francis on World AIDS Day 2013, hoping that "every patient, without exception, has access to the care he needs." Churches and other faith-based organizations are the largest single group providing health care services for people living with HIV—contributing an estimated 50% of facility-based and community care in some countries. Dr. Julio Montaner, director of the BC-CfE, presented at the consultation and applauded the Archbishop and the Vatican for speaking in support of expanding treatment. Treatment as Prevention, a strategy pioneered by the BC-CfE, has been incorporated in the UNAIDS Treatment 2015 framework as well the new Global HIV Treatment Guidelines from the World Health Organization (WHO). The WHO guidelines call for widespread HIV testing and immediate offer of highly active antiretroviral therapy (HAART) to people living with HIV. "The momentum continues to build to implement the Treatment as Prevention strategy to save lives, prevent infections, and, in the long-term, save money," said Dr. Montaner. The Vatican meeting followed an announcement that the BC-CfE and Geneva-based UNAIDS had formalized their partnership to support efforts to bring HIV treatment to all eligible people. Under the new partnership, the BC-CfE will support scientific modelling and activities to highlight the need for immediate investments in life-saving HIV treatment programs. "Julio Montaner and his colleagues at the BC Centre for Excellence in HIV/AIDS are globally recognized for their work on HIV treatment and we are happy to continue this long partnership," said UNAIDS executive director Michel Sidibé. That global recognition was further emphasized when Panama announced in February it had become the latest country to adopt the reatment as Prevention strategy. Panama and the BC-CfE signed a MOU establishing a collaboration to develop new research and HIV programs, and create an HIV fellowship program that will allow Panamanian HIV scientists to come to Vancouver to work with BC-CfE researchers and clinicians. The BC-CfE will provide science and support in the development and evaluation of Panama's Treatment as Prevention program. "British Columbia has been an international leader in developing a strategy proven to combat HIV and AIDS," said Dr. Javier Díaz, Panama Minister of Health. "This partnership will assist us in promoting and collaborating on health priorities affecting the citizens of Panama and the global community in relation to HIV and AIDS." Panama joins China, France, Brazil, and Spain in adopting the strategy as their national HIV/AIDS policy. The strategy has also been implemented by cities in the United States, including San Francisco, New York City, and Washington, D.C. | CHIWOS | Treatment as Prevention® | Forecast Newsletter | Download | |||||||||||||||||||||
| April, 2014 | Dolutegravir (Tivicay™) | Formulary Addition | Dear Doctor Letter | Download | |||||||||||||||||||||||
| March, 2014 | BC-CfE strengthens delivery of HIV education to province's health care practitioners | New condensed offering of preceptorship program now extended to family physicians and nurse practitioners in other health authorities It's lunchtime, but Dr. Silvia Guillemi isn't on break. Instead, she's leading a learning session for a small group of health care providers at St. Paul's Hospital. It's not unusual for Dr. Guillemi to participate in these types of sessions. In fact, as clinical education and training director for the BC Centre for Excellence in HIV/ AIDS (BC-CfE), her time is often divided between treating patients living with HIV and sharing her experience and expertise with health care practitioners interested in HIV care. Since its inception over a decade ago, the BC-CfE's Clinical Education and Training Program has played a pivotal role in improving HIV/AIDS clinical care and treatment through personalized learning programs.
"The BC-CfE's educational activities are adapted to the specific needs of HIV patients and their health care providers," explained Dr. Guillemi, who is also the Assistant Medical Director of the John Ruedy Immunodeficiency Clinic (IDC) at St. Paul's Hospital. "We have tailored our programs to educate health care providers towards the goal of increasing awareness of the importance of testing and treatment, in line with the BC-CfE's Treatment as Prevention strategy." Health care professionals, frontline community workers, and students across B.C. participate in initiatives offered by the Clinical Education and Training Program. Education initiatives include AIDS Care Rounds, Forefront Lectures, HIV Updates, the IDC Journal Club, clinical training, online courses and educational webinars, many of which are accessible on the BC-CfE website. One of the Clinical Education and Training Program's features is the Preceptorship Program. The program is offered in collaboration with the R3 Enhanced Skills Program in the Department of Family Practice at the University of B.C. Traditionally a three-month program, it is available to primary care physicians and family practice residents who want to enhance their skills in the management and treatment of patients with HIV/AIDS. More recently, the BC-CfE offered a shorter version of the Preceptorship Program, in collaboration with Vancouver Coastal Health as part of the STOP HIV/AIDS initiative, for family physicians and nurse practitioners. This initiative has now been extended to B.C.'s Interior Health and Vancouver Island Health Authorities. "Some of the primary objectives of this comprehensive program are to give participants knowledge and experience in the diagnosis, management, and treatment of HIV-positive patients," said Helen Kang, BC-CfE clinical educator. "Beyond the immediate training, the participants establish a working relationship with the BC-CfE for ongoing support and continuing professional development in the HIV field." Successful applicants attend the IDC under the supervision of an HIV-experienced primary care physician, and take part in elective HIV Specialist Clinics, Outpatient Pharmacy, the AIDS ward, and other specialty clinics. The participants obtain knowledge in the initiation of antiretroviral therapies and assessment of co-morbidities, and the ability to recognize, diagnose and appropriately refer patients with HIV-related treatment failure or other complications. Mark Schultz, Family Nurse Practitioner at the Comox Valley Nursing Centre in B.C., completed the Intensive Preceptorship Program in the spring of 2013. "The course was extremely useful and well-organized, providing me with a proper framework for my HIV knowledge base," he said. "I walked away feeling more confident and competent with a stronger understanding of the use of HAART (highly active antiretroviral therapy) and monitoring parameters. More importantly, I feel that it has allowed me to understand and serve my patients better." For more information about the Intensive Preceptorship Program, contact Helen Kang at (604) 682-2344 ext. 63219, or email education@cfenet.ubc.ca. | Forecast Newsletter | Download | |||||||||||||||||||||||
| February, 2014 | HIV Monitoring Quarterly Reports, Fourth Quarter 2013 | STOP HIV/AIDS | Treatment as Prevention¨ | ||||||||||||||||||||||||
| February, 2014 | Supreme Court of Canada strikes down sex work laws in landmark decision | BC-CfE acted as intervener in case that is a critical step towards promoting health and safety, improving HIV prevention The Supreme Court of Canada has struck down the country's anti-prostitution laws in a unanimous decision delivered on Dec. 20. The case of Canada (Attorney General) v. Bedford was initiated in 2007 by three Ontario sex workers: Terri Jean Bedford, Amy Lebovitch, and Valerie Scott. While the exchange of sex for money or goods is not illegal in Canada, the court's decision struck down three key provisions in the Criminal Code that make communicating for the purposes of prostitution, bawdy houses, and living off the avails of prostitute all illegal. The decision upholds sex workers' human rights to work and to health by acknowledging the ways in which criminalization contributes to unsafe working conditions for sex workers. "The prohibitions at issue do not merely impose conditions on how prostitutes operate," wrote Chief Justice Beverley McLachlin in the decion. "They go a critical step further, by imposing dangerous conditions on prostitution; they prevent people engaged in a risky—but legal—activity from taking steps to protect themselves from the risk." Last June, the court heard from a coalition comprising the BC Centre for Excellence in HIV/AIDS (BC-CfE), Canadian HIV/AIDS Legal Network (Legal Network), and the HIV & AIDS Legal Clinic Ontario (HALCO). The co-interveners contributed evidence drawn from years of research and dozens of peer-reviewed publications that resulted largely from two major research projects led by the BC-CfE's Gender and Sexual Health Initiative (GSHI): AESHA (An Evaluation of Sex Workers Health Access), a longitudinal cohort of street and off-street sex workers, and the Ethnographic-Qualitative Project of the HIV Risk Environment, which studies the physical, social and policy features of the work environment. The intervention focused on evidence-based, sex-work policy reform aimed at promoting the health and safety of sex workers, and improving HIV prevention. "We know from our research the law is not only failing to protect, it's actually causing harms," said Dr. Kate Shannon, GSHI director. "The Supreme Court decision striking down these criminal sanctions is a landmark ruling and one that will be a critical evidence-based step towards promoting health and safety in the sex industry." Sandra Ka Hon Chu, co-director of research and advocacy with the Legal Network, says the current approach "has been shown to increase sex workers' risks of, and experiences of, violence as well as to decrease sex workers' negotiating power for safer sex practices." "A new legal framework that respects the human rights of sex workers does not criminalize clients, third parties in sex work or sex workers themselves," said Chu In an op-ed published in the National Post, Dr. Shannon and Chu wrote: "The science is unequivocal: criminalization of sex work in Canada, and globally, has been an abject failure in protecting sex workers from violence, predation and murder, and has exacerbated vulnerability to HIV and other health inequities among sex workers. "Evidence has consistently shown these (current) criminal laws engender stigma, force sex workers to work in isolated and hidden spaces, and prevent access to basic health and support services, including legal and social protections." With this decision, Parliament must ensure any new laws governing sex work do not replicate the harms caused by the unconstitutional provisions. The co-interveners have called for the decriminalization of sex work in Canada. Renée Lang, staff lawyer with HALCO, cites the case of New Zealand as the best model for Canada's government to follow. "Only the decriminalization of sex work—as is the case in New Zealand—truly addresses the stigma, discrimination, and violence faced by sex workers," she said. "There, the sky has not fallen, there has been no substantiated evidence of trafficking, and sex workers are better protected from violence and exploitation." "To reverse the advance of HIV we must ramp up and fully roll out Treatment as Prevention everywhere, something not possible unless we work in coordination to ensure those most in need of treatment and care are able to receive it." - Dr. Julio Montaner, director of the BC-CfE, at World Bank meeting to discuss the Millennium Development Goals this January in Washington, D.C. | Forecast Newsletter | Download | |||||||||||||||||||||||
| January, 2014 | Sexually Transmitted Infections in Adolescents and Adults – British Columbia Treatment Guidelines – 2014 | PEP | Download | ||||||||||||||||||||||||
| January, 2014 | Canada's offer to the Global Fund to Fight HIV/AIDS falls short of international peers |
Dr. Julio Montaner urges federal government to match key donors and deliver on the promise of an HIV- and AIDS-free generation in our lifetime. Following World AIDS Day on December 1, the Global Fund to Fight AIDS, Tuberculosis and Malaria convened leaders from around the world in Washington, D.C. to make funding pledges to end HIV and AIDS. What follows is Dr. Julio Montaner's address of Canada's pledge, which fell short of other nations. In December, the government of Canada announced $650 million in new funding over three years for the Global Fund to Fight HIV/AIDS, Tuberculosis and Malaria. This is the good news. The dollars contributed to the Global Fund, go directly towards helping people living with HIV in developing nations access life-saving treatment. In 2013, UNAIDS reported the scale-up of treatment has enabled nearly 10 million people to gain access to these life-saving medicines. These successes have been in large part due to the efforts of the Global Fund. Evidence has proven treatment can eliminate progression of HIV infection to AIDS and premature death, and dramatically decrease HIV transmission. The made-in-Canada Treatment as Prevention strategy, pioneered by the BC Centre for Excellence in HIV/AIDS, calls for widespread HIV testing and immediate provision of these HIV medicines. It's a strategy that's been proven to work, here in B.C. (the only province to formally implement this strategy), and around the world, where it has been adopted as the national strategy in China, US, France, Brazil and others. In July 2013, the World Health Organization (WHO) incorporated Treatment as Prevention as the new cornerstone of the global HIV guidelines. This has expanded the eligibility for HIV treatment from 15 million to over 25 million people in low- and middle-income countries. While this imposes a tall order in the short term, it has the potential of radically changing the course of the epidemic. Recent analyses demonstrate the full implementation of the 2013 WHO guidelines could avert over three million AIDS deaths and four million new HIV infections by the year 2025. The Global Fund has set a target of $15 billion in funding. We cannot afford to miss this target. Given these circumstances, Canada's newly announced contributions are not nearly enough, especially when compared to our international peers. This newest pledge is equal to approximately $6 per Canadian per year, far less than the nearly $8 per UK citizen and $10 per Nordic citizen. This is all part of an ongoing trend by our federal government to marginalize people living with HIV and AIDS. Ottawa will rightly pride itself about its investments in research aimed to develop a cure or possibly a vaccine for HIV. However, what good would it do to support research if we are not going to implement the results? Insite and HIV Treatment as Prevention are just two examples of Canadian successes that are simply not palatable to the federal government. In Canada, lack of a renewed National AIDS Strategy has led to a rising number of new HIV infections, particularly in Saskatchewan, Manitoba, Newfoundland, and Ottawa. The federal government is failing to address the rapid rise in HIV cases among First Nations communities, an area of their direct responsibility. And now globally, Canada has failed to match the contributions of key donors in the fight against HIV/AIDS. Every year, 3,300 men and women in Canada are diagnosed with HIV. An estimated 71,300 Canadians are now living with HIV, a number that could double within the next 15 years if the current rate of new infections continues and treatment is not expanded across Canada. The federal government has a unique opportunity to turn around the HIV epidemic at all levels of Canadian society, if it implements Treatment as Prevention as a national strategy. We estimate Canada can realize a decrease in new HIV infections by at least 90 per cent in just five years if we fully implement this strategy. The Canadian government's leadership in the fight against HIV/AIDS is long overdue. I urge the Harper government to fully embrace the made-in-Canada HIV Treatment as Prevention strategy nationally and match our peers' contributions to the Global Fund. We have an opportunity to deliver on the promise of an HIV- and AIDS-free generation in our lifetime. The only piece missing now is the political will to make it happen. "The federal government has a unique opportunity to turn around the HIV epidemic at all levels of Canadian society if it implements Treatment as Prevention as a national strategy." | Forecast Newsletter | Download | |||||||||||||||||||||||
| December, 2013 | HIV Monitoring Quarterly Reports, Second Quarter 2013 | * Notice that this is an updated version of a previous report posted on the website. Indicator 8, Figure 8 on page 26 has been updated to correct a technical error. Please discard any previous version and use the updated version instead. This update does not apply to the Northern Health report. If you have any questions please contact Irene Day at iday@cfenet.ubc.ca. | STOP HIV/AIDS | Treatment as Prevention¨ | |||||||||||||||||||||||
| December, 2013 | HIV Monitoring Quarterly Reports, Third Quarter 2013 | STOP HIV/AIDS | Treatment as Prevention¨ | ||||||||||||||||||||||||
| December, 2013 | Memorandum of understanding cements relationship between China and B.C. |
Partnership affirms province's commitment to showcase BC-CfE's world-leading expertise in HIV/AIDS, says Premier China and British Columbia are partnering to advance the global fight against HIV/AIDS. A memorandum of understanding (MOU) was signed by delegates from the BC Centre for Excellence in HIV/AIDS (BC-CfE) and the National Centre for AIDS/STD Control / Prevention and Chinese Centre for Disease Control and Prevention (NCAIDS/China CDC). The MOU cements the relationship between China and the BC-CfE, which first began in 2011 when China announced its implementation of the BC-CfE pioneered Treatment as Prevention strategy. The MOU was signed on November 26 in a ceremony in Beijing, China, and witnessed by B.C. Premier Christy Clark as part of the provincial government's jobs and trade mission in Asia. "This partnership affirms our government's commitment to showcase and share the world-leading expertise of the BC Centre for Excellence in HIV/AIDS," said Premier Clark. "We're pleased British Columbia's innovation and research is being recognized internationally, especially here in China. This exchange will allow us to mutually promote and collaborate on health priorities affecting China, British Columbia, and the global community in relation to HIV/AIDS." The MOU formalizes a collaboration on the implementation of Treatment as Prevention in China and the development of new research and HIV programs both in B.C. and in China, where the Joint United Nations Progamme on HIV/AIDS (UNAIDS) estimates there are more than 780,000 people living with HIV/AIDS and approximately 26,000 people are newly diagnosed each year. The organizations will work jointly to improve the health of British Columbians and Chinese citizens and to enhance capacity to deliver HIV/AIDS education and training to health professionals. The partnership aims to protect and improve the health of people by eliminating HIV/AIDS through science, policy, partnership, and evidence-based public health action. China was the first country to adopt the BC-CfE's Treatment as Prevention model as their national HIV/AIDS policy. The strategy involves widespread HIV testing and immediate offer of highly active antiretroviral therapy (HAART) to people living with HIV. Treatment has been shown to virtually eliminate progression of the disease to AIDS and premature death, and simultaneously stop transmission of HIV. Since implementing Treatment as Prevention in 2011, China has surpassed their HIV detection and treatment goals. "Following the lead of British Columbia and China, the momentum is building to implement Treatment as Prevention to save lives, prevent infections, and, in the long term, save money," said Dr. Julio Montaner, director of the BC-CfE. "I look forward to working with China to ensure Treatment as Prevention is implemented globally based on the best available scientific evidence. The global adoption of Treatment as Prevention holds the promise of ending HIV and AIDS in our lifetime." In 2012, the United States identified Treatment as prevention as a key strategy to achieve an AIDS-free generation, in July 2013, the World Health Organization fully incorporated Treatment as Prevention in their new Global HIV Treatment Guidelines and more recently France and Brazil both announced plans to adopt Treatment as Prevention as their national policies. The China and Bc-CfE MOU will also established a three-year HIV Treatment as Prevention Fellowship program that will allow top Chinese scientists to come to Vancouver to work with researchers and clinicians at the BC-CfE. The Fellowship program will be offered for up to six Chinese scientists over three years. Funding for the Fellowship is supported by Genome BC, Rennie Marketing Systems and St. Paul's Hospital Foundation. "British Columbia has been an international leader in developing a model of the Test and Treat strategy, also referred to as Treatment as Prevention, to combat HIV/AIDS," said Dr. Zunyou Wu, Director of the China CDC. "This agreement deepens the working relationship between China and B.C. "We believe this agreement will provide an opportunity for our researchers to work with and share expertise to best help both B.C. and China meet our goal of bringing HIV and AIDS under control." | Treatment as Prevention® | Forecast Newsletter | Download | ||||||||||||||||||||||
| November, 2013 | Momentum builds globally as France and Brazil adopt Treatment as Prevention | Add Brazil to the growing list of countries to officially embrace the HIV Treatment as Prevention (TasP) strategy.In October, Brazil joined France as the second country in less than a month to announce plans to adopt the made-in-B.C. concept as their national policy to combat HIV/AIDS. "The momentum is increasing to implement this strategy, proven to save lives and prevent HIV transmission," said Dr. Julio Montaner, director of the BC Centre for Excellence in HIV/AIDS (BC-CfE). "We applaud Brazil's leadership, and eagerly await similar announcements from other countries. The global adoption of Treatment as Prevention holds the promise of ending HIV and AIDS in our lifetime." TasP calls for widespread HIV testing and immediate offer of highly active antiretroviral therapy (HAART) to people living with HIV. Evidence has demonstrated treatment can virtually eliminate progression of HIV infection to AIDS and premature death, and simultaneously stop transmission of the virus. The strategy was first introduced by the BC-CfE in 2006, and endorsed by the Joint United Nations Programme on HIV/AIDS (UNAIDS) in 2010. China became the first nation to embrace the strategy in 2011. The next year, the United States identified TasP as a key strategy to achieve an AIDS-free generation. In July 2013, the World Health Organization fully incorporated TasP in their new Global HIV Treatment Guidelines. With the support of the provincial government, B.C. was the first jurisdiction to implement TasP. Together with simultaneous scale-up of harm reduction measures – including needle distribution, opioid substitution treatment, and supervised injection services – B.C. has seen HIV-related morbidity and mortality decline by over 90 per cent since 1995. Over the same time period, the number of new HIV diagnoses has fallen from more than 800 per year in 1995 to 238 in 2012. B.C. remains the only province in Canada to implement TasP and to demonstrate a consistent decline in new cases of HIV. "We're pleased this groundbreaking, made-in-B.C. strategy developed by Dr. Montaner and his team, and implemented here in British Columbia, is being embraced around the world," said Terry Lake, B.C.'s Minister of Health. "Our government is committed to reducing the spread of HIV and improving the lives of those living with HIV. That other governments share our vision for an AIDS-free generation is a testament to the success of TasP." In Brazil, the country's Ministry of Health expects the expansion of treatment will lead to at least 100,000 new people living with HIV gaining access to HAART. Currently, there are 313,000 people receiving HIV treatment in Brazil. "Implementing Treatment as Prevention is critical to our ability to control the HIV and AIDS pandemic in Brazil," said Fábio Mesquita, director of the Sexually Transmitted Diseases (STD), AIDS and HIV Department of Brazil's Ministry of Health. "We believe this strategy is the model for care and prevention that will best help bring this disease to its knees." Despite the international community embracing this HIV elimination strategy, Canada has yet to adopt TasP. "We have a plan, it's been proven to work, yet Ottawa continues to ignore the evidence," said Dr. Montaner. "Too many lives are at stake for us not to act now. We need to urgently renew the National AIDS Strategy, and embrace TasP to free the next generation of the burden of HIV/AIDS." Every year, 3,300 men and women in Canada are diagnosed with HIV. An estimated 71,300 Canadians are now living with HIV, a number that could double within the next 15 years if the current rate of new infections continues and treatment is not expanded across Canada. "Federal Health Minister Rona Ambrose is medically, morally and ethically wrong. This again falls into a pattern on the part of the federal government of acting based on ideology, while ignoring the science." | Forecast Newsletter | Download | |||||||||||||||||||||||
| October, 2013 | Treatment as Prevention leads to B.C. having largest decline in rate of new HIV diagnoses | Policymakers need to adopt Treatment as Prevention as a national strategy to fight HIV/AIDS, urges researchers at the BC Centre for Excellence in HIV/AIDS (BC-CfE) in an article published this month in HIV Medicine. New HIV diagnoses in British Columbia are continuing to decline at a rate faster than in other Canadian regions, report researchers after analyzing Health Canada data from 1995 to 2011. "British Columbia, of all Canadian jurisdictions, has had the largest decline in the rate of new HIV diagnoses and in lifetime costs averted over the study period," write the authors, who include Dr. Julio Montaner, director of the BC-CfE, and Dr. Robert Hogg, director of the Epidemiology and Population Health Program at the BC-CfE. "Further efforts are needed to optimize the potential impact of Treatment as Prevention in the whole of Canada." B.C., where the Treatment as Prevention strategy was pioneered and implemented, is the only province to promote widespread and fully government-supported access to HIV testing and highly active antiretroviral therapy (HAART). As a result, B.C. has seen HIV-related morbidity and mortality decline by approximately 90 per cent since the early 1990s, and the number of new HIV diagnoses has fallen from approximately 800 per year prior in 1996 to 238 in 2012. "The consistent and sustained decrease in new HIV diagnoses in B.C. reinforces Treatment as Prevention as a highly effective approach in the fight against HIV/AIDS," said Dr. Montaner. "The evidence should be absolutely clear: Treatment as Prevention is the best way to achieve an HIV- and AIDS-free generation. It's time for Canada's leaders to emulate the government of B.C. and adopt this as the national strategy to stop HIV/AIDS." In Canada, there are an estimated 71,300 individuals living with HIV. While annual rates of new HIV diagnoses declined slightly in Ontario, Quebec and the Atlantic provinces, B.C. demonstrated the most significant decline between 1995 and 2011, from 18.05 to 6.49 per 100,000 population. In comparison, rates in Saskatchewan increased from 2.76 to 16.17 per 100,000 population, and in Manitoba they increased from 4.52 to 6.53 per 100,000 population. Rates of new HIV diagnoses in Alberta and in the Territories remained constant over the study period, demonstrating neither an increase nor a decrease. It is estimated that B.C. has averted $3.06 million per 100,000 population in lifetime costs for averted cases of HIV infection since 1996, compared to $1.38 million and $432,000, respectively, for Ontario and Quebec. In contrast, it is estimated Saskatchewan and Manitoba have incurred an additional cost of $2.06 million and $956,000, respectively, per 100,000 population for the increase in new cases since 1996. "The evidence we reviewed really demonstrates further efforts are needed to optimize the potential impact of Treatment as Prevention in the whole of Canada," said Dr. Hogg. "We should look at what has been accomplished in British Columbia and apply those lessons to other jurisdictions without further delay." The World Health Organization and the Joint United Nations Programme on HIV/AIDS (UNAIDS) have adopted the Treatment as Prevention strategy, as have other jurisdictions throughout the world, including China and, most recently, France. In addition, the U.S. has identified Treatment as Prevention as a key strategy to achieve an AIDS-free generation. | Treatment as Prevention® | Forecast Newsletter | Download | ||||||||||||||||||||||
| August, 2013 | UNAIDS urges rapid expansion of access to HIV antiretroviral medicines |
BC-CfE champions approach to scale up antiretroviral treatment to 15 million people worldwide by 2015The BC Centre for Excellence in HIV/AIDS (BC-CfE) applauds the Joint United Nations Programme on HIV/AIDS (UNAIDS) for launching a new framework to accelerate action towards the aim of reaching 15 million people with antiretroviral treatment by 2015. UNAIDS based the new framework on the consolidated guidelines recently put forward by the World Health Organization (WHO) to initiate HIV treatment sooner in order to save more lives and prevent more infections. In B.C., this approach has been implemented for several years via the BC-CfE-developed Treatment as Prevention strategy, which calls for widespread HIV testing and earlier access to treatment for all medically eligible individuals. As part of the strategy, the Seek and Treat for Optimal Prevention of HIV/AIDS (STOP HIV/AIDS) initiative, designed to expand access to HIV/AIDS medications among hard-to-reach and vulnerable populations, was expanded province-wide in April 2013.. "The end of AIDS is within our grasp, and expanding treatment as prevention, as recommended by the 2013 WHO guidelines, will bring this epidemic to its knees," said Dr. Julio Montaner, director of the BC-CfE. "Together, we can stop AIDS, and move towards realizing the vision of an HIV and AIDS-free generation. We should rally behind UNAIDS to make the most of this extraordinary opportunity." UNAIDS' framework, entitled Treatment 2015, provides countries with methods to rapidly scale up HIV treatment access to reach this goal initially set by United Nations Member States in 2011, and furthering this target to nearly 26 million people on antiretroviral therapy as soon as possible thereafter. "Reaching the 2015 target will be a critical milestone," said Michel Sidibé, Executive Director of UNAIDS. "Countries and partners need to urgently and strategically invest resources and efforts to ensure that everyone has access to HIV prevention and treatment services." Treatment 2015 was developed in partnership with the Global Fund to Fight AIDS, Tuberculosis and Malaria and the U.S. President's Emergency Plan for AIDS Relief (PEPFAR), as well as with the African Union and other key stakeholders, to maximize the impact of HIV treatment on the prevention of morbidity, mortality, and HIV transmission. The framework emphasizes the importance of HIV testing and counseling as gateways to expanding access to antiretroviral therapy and that further efforts are required to normalize HIV testing. UNAIDS' framework follows guidelines put forward by the WHO at the 7th International AIDS Society (IAS) Conference on HIV Pathogenesis, Treatment and Prevention in Kuala Lumpur, Malaysia. Treatment 2015 outlines three fundamental pillars essential to reaching the 2015 target: increasing demand for HIV testing and treatment services; mobilizing resources and improving the efficiency and effectiveness of spending; and ensuring more people have access to antiretroviral therapy. UNAIDS notes just 30 countries account for nine out of 10 people who are eligible for antiretroviral therapy, but who do not have access. Intense focus on scaling up HIV services in these 30 countries would have a significant impact on the trajectory of the global AIDS epidemic. The framework also calls for all countries to use the best available data to identify key geographical settings and populations with high HIV prevalence and disproportionate unmet need for antiretroviral therapy. In B.C., since 1996, the number of HIV-positive individuals receiving treatment has increased from 837 to more than 7,000 in 2012, and HIV-related morbidity and mortality have both declined by approximately 90 per cent since the early 1990s. The number of new HIV diagnoses fell from approximately 900 per year prior to 1996 to 238 in 2012. {photo caption: Michel Sidibé, Executive Director of UNAIDS} "Scaling up access to antiretroviral treatment is critical to achieving an AIDS-free generation." | Forecast Newsletter | Download | |||||||||||||||||||||||
| June, 2013 | Research shows war on drugs failing to limit drug use in Vancouver | Researchers from the BC Centre for Excellence in HIV/AIDS (BC-CfE) released this month a comprehensive report on the drug situation in Vancouver at an event at the Carnegie Community Centre in the city's Downtown Eastside. The Drug Situation in Vancouver report, published by the BC-CfE Urban Health Research Initiative (UHRI), compiled 15 years of data examining the ongoing public and individual health-related harms resulting from illicit drug use, including HIV and hepatitis C transmission. It is the second edition of the report, the first was released in 2009. Community members filled the auditorium to hear the latest findings, which demonstrated health-focused policies have been more effective than federal law enforcement measures at reducing illicit drug use and improving public health and safety. Dr. Thomas Kerr, report co-author and UHRI co-director, presented detailed research on drug use trends, drug availability, HIV rates, and behaviours among some of the city's most vulnerable people who use illicit drugs. The research found fewer people using injection drugs, significant decreases in syringe sharing and related HIV and hepatitis C transmissions, an increase in drug cessation, and improved access to addiction treatment. These positive trends were seen despite the unchanged ease of access to and affordability of illicit drugs. "Drug trends in Vancouver are shifting, with fewer people injecting drugs and more people ceasing their use, a result of the innovative harm reduction and addiction treatment programs implemented," said Dr. Kerr. "It's important [that] policymakers at all levels of government take note of this evidence and focus efforts on approaches proven to be effective. Continuing to invest in failed policies like the war on drugs does little to reduce health and social harms." Included among the harm reduction approaches implemented are the supervised injection facility InSite, free safer smoking kits for crack users, and syringe exchange programs. The result of these combined approaches has been a significant decrease in the number of people newly infected with HIV and hepatitis C over the past 15 years. In addition, access to methadone maintenance treatment among people who use drugs increased from 11.7 per cent in 1996 to 54.5 per cent in 2008, remaining stable since. Furthermore, reports of difficulty accessing addiction treatment dropped from 19.9 per cent in 1996 to as low as 3.2 per cent in 2006, and have remained below 1996 levels. There was a corresponding upward trend of injection drug use cessation during a similar period, with a rate of just 0.4 per cent in 1996 compared to 46.6 per cent in 2011. Conversely, researchers found that between 2000 and 2011 illicit drugs remained easily accessible and prices were stable. Based on these findings, the report recommends continued support for harm reduction and addiction and HIV/AIDS treatment programs to improve the health of people who use drugs. Treatment as Prevention initiatives should be embraced and brought to scale to prevent mortality among people living with HIV and limit further HIV transmission. "Needle exchanges and the supervised injection facility have [been] proven to save lives, but drug use trends are changing and policies and programs should reflect these changes," said Lorna Bird, a drug user and member of the Western Aboriginal Harm Reduction Society who also spoke at the Carnegie event. "We need more harm reduction interventions, like safer crack smoking kits, supervised consumption facilities for people who smoke illicit drugs, and programs focused on at-risk youth." | Forecast Newsletter | Download | |||||||||||||||||||||||
| May, 2013 | Drug Treatment Program Registry - Program Information Sheet | Click here to link to the Drug Treatment Program Participant Information Sheet | Notice to prescribers and clients | Dear Doctor Letter | Download | ||||||||||||||||||||||
| May, 2013 | Elvitegravir-cobicistat-emtricitabine-tenofovir DF (Stribild™) | Formulary Addition | Dear Doctor Letter | Download | |||||||||||||||||||||||
| May, 2013 | 'Global responsibility is in front of us' to implement guidelines, urges multi-disciplinary panel | 'Global responsibility is in front of us' to implement guidelines, urges multi-disciplinary panelInternational HIV Treatment as Prevention Workshop opens with call for immediate scale-up of access to treatmentThis past April, hundreds of leading international HIV experts gathered in Vancouver for the 3rd International HIV Treatment as Prevention Workshop.
Douglas spoke of the potential impact of Treatment as Prevention™, which involves widespread HIV testing and treatment to medically eligible people who are found to be HIV positive. "Using Treatment as Prevention™, in combination with other interventions, the Caribbean countries can end AIDS and HIV", he said. An estimated 6.8 million people worldwide are eligible for treatment but unable to access it. Mr. Sidibé called for the urgent scale up of access to treatment. "If we have the evidence that antiretroviral therapy canhelp someone living with HIV to stay alive and protect their sexual partners from infection by up to 96%, then we have a moral obligation to make it available," said Sidibé. "Providing HIV treatment as soon as possible is ethically and morally correct, economically and programmatically feasible and consistent with what we have learnt about clinical best practice over the last decade." It was a viewpoint shared by the others on the panel. Goosby argued an AIDS-free generation is in sight if the political will is present to share the responsibility. "The global responsibility is in front of us," he said. Throughout the workshop, researchers and policy makers shared data, protocols and findings, and participated in discussions to identify how best to move forward on implementing Treatment as Prevention™. The World Health Organization presented international guidelines, which provide clinical, operational and programmatic guidance for scaling up HIV programs in low- and middle-income countries following a public health approach. As in the opening roundtable session, many of the discussions focused on the need for political will to implement these guidelines. | Forecast Newsletter | Download | |||||||||||||||||||||||
| April, 2013 | Apr-13 | Provincial government eyes Treatment as Prevention to fight viral hepatitisApplication of BC-CfE's HIV model could deliver a hepatitis-free generation to our province and be applied to other high burden diseasesThe Treatment as Prevention approach to fighting HIV has been so successful in British Columbia, the provincial government plans to implement a similar approach to combatting viral hepatitis.
Viral hepatitis affects thousands of British Columbians, many of whom are unaware they even have the disease. The BC Centre for Disease Control estimates that 80,000 British Columbians are living with hepatitis C, and 60,000 are living with hepatitis B. "We are committed to working to improve the health of all British Columbians and their families who may be affected by viral hepatitis," said Minister MacDiarmid. "While treatment and disease management of hepatitis B and hepatitis C is important, it is also critical to improve awareness, education and knowledge about the disease and how it can spread, particularly among our more vulnerable groups." In applying the successful HIV Treatment as Prevention model, work will focus on: determining vulnerable individuals; identifying the best ways to prevent new infections; how to engage those at risk or living with the diseases in testing, treatment and support; and, assess how improved reach and effectiveness of new antiviral treatments could impact those living with the viruses, and ultimately change the course of the hepatitis epidemics. "With the support of the B.C. government, we have led the way in the fight against HIV/AIDS. Now, we hope to do the same with viral hepatitis," said Dr. Julio Montaner, Director of the BC-CfE. "What we have done for HIV can and should be done for other high burden diseases like hepatitis. We can take the infrastructure we have developed under STOP HIV/AIDS and apply it so we can deliver a hepatitis-free generation to our province." Both hepatitis B and C are viruses that infect the liver and can lead to permanent liver damage, including liver cancer and liver failure. Hepatitis B and C are often referred to as "silent" diseases because often no symptoms appear until the infected person's liver is severely damaged – a process that can sometimes take decades. Hepatitis B is primarily spread through intimate contact with an infected person. Most adults who get hepatitis B recover. However, it can become a long-term, chronic disease that can damage a person's liver over time. Chronic illness is especially common among those who were exposed to the hepatitis B virus at birth and did not receive a vaccine. There are treatments available for hepatitis B that can reduce the amount of virus circulating in the body and decrease the damage to the liver. Regular check-ups are key to determine which individuals will benefit the most from treatment. Hepatitis C is primarily spread through direct contact with an infected person's blood. There is no vaccine for hepatitis C. Some people who are infected completely recover from the virus after a short-term, acute illness. However, many become chronically infected and their liver can be damaged, as with hepatitis B. There are treatments available that can cure many who are chronically infected. This project will be funded through the St. Paul's Hospital Foundation. The province also provided an additional $400,000 grant to the S.U.C.C.E.S.S. Society will help improve awareness of hepatitis B, and provide prevention, treatment and self-management education among immigrant communities. | Forecast Newsletter | Download | |||||||||||||||||||||||
| March, 2013 | Mar-13 | Thai drug user study calls for greater investment in evidence-based healthcareLatest research from BC-CfE's international program highlights failure of "war on drugs"A new study from researchers at the BC Centre for Excellence in HIV/AIDS (BC-CfE) adds to the growing mountain of evidence pointing to the international war on drugs as a failed policy.
The study, soon to be published in the peer-reviewed journal Drug and Alcohol Dependence, calls for greater investment in evidence-based healthcare and harm-reduction initiatives for injection drug users (IDU) in Thailand, both to save lives and prevent HIV infections. "Drug addiction is a chronic, relapsing health condition and research shows that it is best addressed through evidence-based drug treatment," said Dr. Thomas Kerr, senior author of the study and co-director of the Urban Health Research Initiative, a program of the BC-CfE. "The findings of this study and various prior reports provide significant evidence that simply incarcerating people who use drugs will not help achieve the objective of reducing the demand and supply of illegal drugs. "In fact, this approach has led to unintended negative consequences such as strengthening the link between users and drug dealers, and health risks such as HIV/HCV transmission." The study is the latest research to come MSCRP. For decades, Thailand had experienced high rates of illicit drug use and HIV/AIDS among IDU. However, as highlighted in the study, the Thai government's response has been to rely on criminal justice approaches such as policing, incarceration and compulsory drug detention centres. MSCRP was launched in 2008 under the leadership of Dr. Kerr with the goal of reducing these drug-related harms. MSCRP is a collaboration among the BC-CfE, the Thai AIDS Treatment Action Group, the Mitsampan Harm Reduction Center and Chulalongkorn University in Bangkok. The project has since published 18 peer-reviewed studies that have provided insight on previously undocumented social and structural vulnerabilities to HIV/AIDS and other drug-related harm among IDUs in Bangkok. The work has also garnered broad media attention in Thailand, including stories in some of the country's highest circulation daily newspapers. The new study was covered in publications across Thailand. However, the outreach goes beyond media coverage. The project has been successful in developing important relationships with community groups, local politicians and public health officials. "Our project has been favourably received by local IDU communities, as well as other civil society organizations engaged in harm reduction programs in Thailand," said Kanna Hayashi, research coordinator for MSCRP. In September 2011, MSCRP published a research summary report that included a series of recommendations for the Royal Thai Government and United Nations (UN). Following its publication, they assembled a panel of high-level officials from various Thai authorities and UN agencies to present the recommendations, which included exploring models for the decriminalization of illicit drug use, providing evidence-based harm reduction services and phasing out compulsory drug detention centres. The message has been received. "For far too long, we have focused on compulsory drug detention as a way to address the rampant issue of illicit drug use, but this study and reports before it have showed that this approach has failed," said former Thai senator Jon Ungphakorn following the publication of the MSCRP's recent research. "The time has come to move away from incarcerating people who use drugs and instead invest in proven addiction treatment and harm reduction programs to meaningfully address their treatment and care needs." | Forecast Newsletter | Download | |||||||||||||||||||||||
| February, 2013 | Feb-13 | The time is now to invest in Treatment as Prevention in the fight against HIV/AIDSDr. Julio Montaner shows B.C. business leaders and the community the urgency to implement Treatment as Prevention to achieve an AIDS-free generation
Dr. Montaner, Director of the BC Centre for Excellence in HIV/AIDS (BC-CfE), was the featured speaker at this year's St. Paul's Health Forum, presented by the St. Paul's Hospital Foundation. His presentation, Treatment as Prevention: The key to an AIDS-free generation, highlighted the latest progress in the battle to stop HIV/AIDS and the steps necessary to end the disease. The St. Paul's Health Forum was launched as a venue to allow the public to hear directly from the hospital's world-leading experts. This year's forum served as an opportunity for the call to implement Treatment as Prevention to reach an audience that included community members and business leaders — those who have the most personally invested in the research and those most able to financially invest and support its advancement" David Poole, Senior Vice-President of Scotiabank, BC & Yukon, and chair of the St. Paul's Hospital Foundation Board of Directors, said Dr. Montaner made a solid business case. "We organized this HIV Forum to give the public an opportunity to hear Dr. Montaner discuss the incredible work he and the BC-CfE are conducting at St. Paul's," said Poole. "The evidence is clear: We can eliminate HIV and reduce undue burden on our strained health care system by supporting Treatment as Prevention. We can prevent new diagnoses while at the same time improving the lives of those diagnosed." Dr. Montaner underlined the urgency for action. "To curb HIV and reach the promise of an AIDS-free generation, we must ramp up and fully roll out Treatment as Prevention in Canada and around the world," Dr. Montaner said. "You can deliver on an AIDS-free generation. All you need to do is implement what we already know." Treatment as Prevention combines the latest in testing, treatment, care and support. The ground-breaking strategy, pioneered by the BC-CfE, involves widespread HIV testing and access to highly active antiretroviral therapy to those medically eligible. It has led to a marked decrease in morbidity, mortality and HIV transmission. At the height of the epidemic in the early 1990s, one person in B.C. was dying every day of AIDS. In 2012, the number of new HIV diagnoses had dropped to 289. As the only province to implement the Treatment as Prevention strategy, B.C. stands alone as the sole province to show a consistent decline in new HIV diagnoses. Of those whose lives have been improved is Barbara Lieske, a patient of Dr. Montaner's since she was first diagnosed with HIV in 2000. Lieske also spoke at the Health Forum, delivering a deeply personal account of when she was diagnosed and how treatment saved her life. "When I was released from the hospital in January of 2000 my CD4 count was seven and my viral load was in the millions," Lieske told the audience. "Thanks to Dr. Montaner, my CD4 count hovers around 950 and my viral load is undetectable. My life is not over. I have not stopped living." B.C. continues to support Treatment as Prevention. Last November, the B.C. government announced the provincial roll-out of the STOP HIV/AIDS pilot project, committing $19.9-million in annual funding to the program that provides widespread HIV testing and treatment. For more information about the St. Paul's Forum on HIV/AIDS, visit www.helpstpauls.com. | Forecast Newsletter | Download | |||||||||||||||||||||||
| January, 2013 | Jan-13 | Homelessness and childhood sexual abuse lead youth to injection drug useTwo first-of-a-kind studies from the BC Centre for Excellence in HIV/AIDS reinforce need for addiction treatment and prevention for homeless youth
According to a pair of new studies from researchers at the BC Centre for Excellence in HIV/AIDS (BC-CfE) and the University of British Columbia (UBC), homelessness and a history of childhood sexual abuse place Vancouver street-involved youth at great risk of intravenous injection drug use and potential transmission of HIV and hepatitis C. The landmark studies, funded by the US National Institute on Drug Abuse and the Canadian Institutes of Health Research, were aimed at identifying why some high-risk youth initiate injection drug use while others do not. Results published in the peer-reviewed Journal of Adolescent Health showed that youth who were homeless were almost twice as likely to start injecting drugs as youth who were not homeless. In a separate study published in the peer-reviewed journal Preventive Medicine, researchers found that youth reporting childhood sexual abuse were more than two-and-a-half times as likely to start injecting drugs as those who had no history of such abuse. "There are serious medical harms associated with injection drug use, including the transmission of HIV and hepatitis C," said Dr. Kora DeBeck, lead author of the Journal of Adolescent Health study and a post-doctoral fellow at BC-CfE and UBC. "While overall rates of injection drug use are down in Vancouver, there is increasing evidence that expanding addiction treatment interventions and providing other tools like supportive housing can intervene to further reduce rates of injection drug use among street youth." Dr. Scott Hadland, lead author of the Preventive Medicine study and chief resident in pediatrics at Harvard University-affiliated Boston Children's Hospital, added: "The high prevalence of childhood sexual abuse and subsequent injection drug use among homeless and street youth highlights the need to develop addiction and treatment strategies based on the traumatic situations they often face." Data for both studies was derived from the BC-CfE's At-Risk Youth Study (ARYS), a prospective cohort of street-involved youth in Vancouver aged 14 to 26 years old, in an effort to untangle the mystery of why some youth choose to begin injecting drugs while others do not. Investigators for the Journal of Adolescent Health study interviewed 422 street-involved youth between September 2005 and November 2011. For Preventive Medicine, researchers studied 395 street-involved youth from October 2005 to November 2010. As part of their research, they also identified key risk factors that can be targeted for implementing treatment and prevention programs. "These are among the first studies to identify early life experiences and subsequent environments that clearly contribute to initiation of injecting drug use," said Dr. Evan Wood, Canada Research Chair in Inner City Medicine at UBC and senior author of both studies. "This research underscores the urgent need for evidence-based interventions to address homelessness and child abuse, as well as the immediate expansion of evidence-based addiction treatment services for high-risk youth." The BC-CfE is actively working to support expanded addiction treatment in B.C. | Forecast Newsletter | Download | |||||||||||||||||||||||
| December, 2012 | STOP HIV/AIDS Pilot Project Indicators Report - Q1 2012 (PDF) | STOP HIV/AIDS | Download | ||||||||||||||||||||||||
| December, 2012 | STOP HIV/AIDS Pilot Project Indicators Report - Q2 2012 (PDF) | STOP HIV/AIDS | Download | ||||||||||||||||||||||||
| December, 2012 | Dec-12 | B.C. government announces provincial expansion of landmark STOP HIV/AIDS pilot programHealth Minister Margaret MacDiarmid committed annual funding of $19.9 million to health authorities to help fulfill the Province's vision for an AIDS-free generation
Since 2009, Seek and Treat for Optimal Prevention of HIV/AIDS (STOP HIV/AIDS) has been implemented in Vancouver and Prince George, and has been successful in dramatically reducing HIV transmission by ensuring HIV-positive individuals have access to the best possible care and treatment. At a news conference on November 30 at St. Paul's Hospital, Health Minister Margaret MacDiarmid and Minister of State for Seniors Ralph Sultan joined BC Centre for Excellence in HIV/AIDS' (BC-CfE) director Dr. Julio Montaner to announce the expansion of the pilot program across B.C. "An AIDS-free generation is now in our sights," said Minister MacDiarmid. "I am pleased to announce the provincial expansion of the STOP HIV/AIDS program. By reaching and engaging more British Columbians at risk for or living with HIV/AIDS, not only will better care be provided, the treatment will also significantly reduce the spread of the virus." Beginning April 1, 2013, the STOP HIV/AIDS program will allow health professionals and community partners to better engage the broader community and specific at-risk groups in HIV testing, reach more people with HIV/AIDS, and enable more British Columbians to be treated. Expansion will be carried out by the province's health authorities with support and leadership from the BC-CfE, which pioneered the concept of Treatment as Prevention under Dr. Montaner's guidance. The BC-CfE will also continue to monitor and evaluate the progress of the program. Dr. Montaner thanked the B.C. government for their ongoing support of this program to eliminate HIV/AIDS in the province. "B.C. is years ahead of the rest of the world in treating HIV/AIDS," said Dr. Montaner at the news conference. "We have a revolutionary new development in health care, right here. The results we have achieved are quite compelling, and the world is beginning to move [towards our approach]. The times are right." B.C. is leading the way in its efforts to combat the epidemic. BC-CfE researchers recently published a new study, which found that B.C. is the only province in Canada showing a consistent decline in new HIV diagnoses, in part due to the widespread availability of free antiretroviral treatment in the province. The study found that new HIV diagnoses in B.C. have dropped from 900 new cases each year in the mid-1990s, to 289 new cases in 2011. B.C. resident Walter Hiebert can attest to the benefits of treatment. He was diagnosed in 1988 – a time when an HIV diagnosis amounted to a death sentence. In the mid-1990s he was put on highly active antiretroviral therapy (HAART) by Dr. Montaner. He spoke in support of the government's announcement at the news conference. "I watched a lot of friends die. If it wasn't for Dr. Montaner, I wouldn't be alive today. We live in a province that believes in evidence-based science," an emotional Hiebert told the audience. The initial four-year, $48-million STOP HIV/AIDS pilot has allowed health professionals in the pilot areas to identify more people who have HIV/AIDS and enabled more people to be treated with HAART. In contrast, in non-pilot health authorities, there has been an overall decline in the number of people being diagnosed with HIV and the number of people accessing treatment.
| Forecast Newsletter | Download | |||||||||||||||||||||||
| November, 2012 | Nov-12 | Landmark study reinforces benefits of antiretroviral treatmentBC-CfE researchers call for national implementation of made-in-Canada Treatment as Prevention strategy to save lives and curb the spread of HIV
A new study from the BC Centre for Excellence in HIV/AIDS (BC-CfE) showed that highly active antiretroviral therapy (HAART) reduces new HIV diagnoses, deaths and HIV prevalence, suggesting that the made-in-Canada Treatment as Prevention strategy should be implemented across the country. The study, published in the peer-reviewed journal PLOS ONE, investigated patterns of new HIV diagnoses, HIV-related mortality and HAART use in Canada from 1995 to 2008. Analysis showed that for each 10 per cent increment in HAART coverage, the rate of new HIV diagnoses decreased by eight per cent in B.C., Ontario and Quebec — the three provinces with the largest epidemics. In British Columbia, the B.C.-pioneered Treatment as Prevention strategy has led to the widespread expansion of HAART coverage. The total number of new HIV diagnoses in the province dropped during the period of the study from 682 in 1995 to 348 in 2008, and the decline continues, with 289 new HIV diagnoses in 2011 despite an increasing number of tests being done. "The dramatic and sustained decrease in AIDS-related morbidity and mortality and new HIV infections in British Columbia reinforces Treatment as Prevention as a highly effective approach in the fight against HIV/AIDS," said Dr. Julio Montaner, senior author of the study and director of the BC-CfE. "The evidence is clear: the time is now for Canada's leaders to take action and implement Treatment as Prevention as the national strategy in the fight against HIV/AIDS. To do anything less would be a failure in their duty to protect the health of all Canadians." The study found that B.C. has also averted more cases of HIV than Ontario and Quebec combined, in part because B.C. is the only province to offer completely free HAART to virtually all HIV-infected individuals. Findings showed that in 2008, the province averted 10.33 cases of HIV per 100,000 population compared to 3.40 and 0.33 averted cases for Ontario and Quebec respectively. In other provinces, HAART coverage is more limited and the number of new HIV diagnoses per year has remained relatively unchanged, even increasing in some jurisdictions. For instance, the Prairies showed a four-fold increase in rates of new diagnoses over the course of the study period, driven by new infections in Saskatchewan, where each year on average, 200 people are newly diagnosed with HIV infection. "This study provides compelling evidence that expanded HAART coverage can markedly curb the impact of HIV," said Dr. Robert Hogg, lead author of the study and director of the Epidemiology and Population Health Program at the BC-CfE. "Immediate access to free HAART should be considered a clinical imperative and a human rights priority." Every year, 3,300 men and women in Canada are diagnosed with HIV infection and it is estimated that 65,000 Canadians are now living with HIV. Study findings show that this number could double within the next 15 years if the current rate of new infections continues and treatment is not expanded across Canada.
| Forecast Newsletter | Download | |||||||||||||||||||||||
| October, 2012 | Oct-12 | HIV leaders unveil Declaration to End HIV/AIDS in AmericaTreatment as Prevention is a key component in the historic document that outlines the values and principles that will guide work to end the epidemicDr. Julio Montaner chaired a blue ribbon panel of more than 80 HIV/AIDS activists and advocates from across the United States who, in conjunction with the National Minority AIDS Council, developed the Declaration.
At first glance, it's an unlikely setting for a gathering of public health officials. But amidst the glitter and glamour that is often associated with the city, more than 2,000 clinicians, care providers, activists, and advocates gathered to discuss the latest trends, groundbreaking interventions, and cutting-edge strategies at the 16th United States Conference on AIDS (USCA). The conference was preceded by the unveiling of the Declaration to End HIV/AIDS in America in a signing ceremony at the first ever Summit to End HIV/AIDS in America. The Declaration represents a written oath to end the HIV/AIDS epidemic that will require a commitment of money, in-kind donations and human resources. The document focuses on four main points: the promotion of leadership by People Living with HIV/AIDS (PLWHA) in efforts to increase health care engagement and treatment; the elimination of new HIV infections; reducing the stigma, discrimination, and social injustices which increase HIV vulnerability and health disparities; and the maintenance of a strong commitment to finding a vaccine and a cure. "It is possible to realistically envision an end to HIV/AIDS. We've seen the evidence in British Columbia, where the implementation of Treatment as Prevention has dramatically decreased AIDS-related morbidity and mortality and new HIV infections," said Dr. Julio Montaner, director of the BC Centre for Excellence in HIV/AIDS. "But we won't achieve it overnight. It will take ongoing commitment, courage and vision. The signing of the Declaration from leaders across North America represents a compelling first step in making this dream a reality." The Treatment as Prevention strategy advocates for increased testing and immediate treatment of those who are found to be HIV-positive and medically eligible. Pioneered by Dr. Montaner, it has been heralded internationally by organizations such as the Joint United Nations Programme on HIV/AIDS (UNAIDS) and the World Health Organization (WHO) as the way forward in the fight against the epidemic. Implementation of this strategy in B.C. has made the province the only one in Canada to show a consistent decline in new HIV infections. Kali Lindsey, director of Legislative & Public Affairs at the National Minority AIDS Council, underscored critical scientific developments such as Treatment as Prevention that will greatly impact the fight against the disease. He echoed Dr. Montaner's comments that for the first time in 30 years, we have the tools to end HIV/AIDS, however a steadfast commitment will be needed to reach the goal of an AIDS-free generation. The Declaration was opened for public signatures following the conference and had added more than 400 signatures in less than 24 hours, including those of basketball star and HIV activist Magic Johnson and television personality Wendy Williams. | Forecast Newsletter | Download | |||||||||||||||||||||||
| September, 2012 | SAFETY UPDATE: Nevirapine 400 mg XR (Viramune XR™) tablet remnants in feces | September 17, 2012 - The Pharmacovigilance Program at the BC Centre for Excellence in HIV/AIDS has received reports of patients seeing nevirapine 400 mg XR (extended release) tablets or tablet fragments in their feces (stools). In BC, approximately 4% of patients treated with nevirapine XR have reported seeing tablet remnants in their stool. Nevirapine 400 mg XR tablets are formulated in a non-digestible cellulose-based matrix, with the drug dispersed throughout the matrix. When tablets are swallowed, nevirapine is released into the gastrointestinal tract and absorbed into the body and the inactive tablet matrix is eliminated in the feces. Softened tablet remnants may sometimes resemble "whole" tablets, but laboratory testing has shown that the remnants are primarily inactive ingredients – the nevirapine dose has been released. The manufacturer acknowledges that reports of nevirapine XR tablet remnants in the feces have been documented among clinical trial participants and during post-marketing monitoring in other countries. To date, there have been NO known cases of treatment failure associated with the observation of nevirapine XR tablet remnants in feces (including "whole" tablets) either in British Columbia or in the manufacturer's global database. Quality control tests of tablet samples have confirmed that nevirapine XR tablets meet all the product specifications for dissolution performance. There is currently no safety concern associated with the observation of nevirapine XR tablets or tablet fragments in the stool under normal physiological conditions. Nevirapine 400 mg XR tablets are available to treatment-eligible patients through the BC-CfE Drug Treatment Program. | Pharmacovigilance Initiative, Quality and Safety | HIV Clinical Care | Download | ||||||||||||||||||||||
| September, 2012 | Sep-12 | BC-CfE, St. Paul's and UBC to lead new addiction medicine fellowship programGoldcorp donation will be used to help establish an addiction training program – the first of its kind in the world
The announcement was made on September 21 at the newly renamed Goldcorp Centre for Mental Health on East Hastings. With the largest concentration of injection drug users in the country, the Downtown Eastside suffers from high rates of infectious diseases, including HIV and hepatitis C, and overdose deaths stemming largely from high rates of untreated drug and alcohol addiction. Making matters worse, residents are commonly unable to access drug and alcohol treatment, in large part because of the limited number of specialized addiction medicine physicians. Three million dollars from Goldcorp's gift will be used to address this shortfall through the establishment of the Goldcorp Fellowship in Addiction Medicine at St. Paul's Hospital, which will be Canada's only addiction medicine training program west of Ontario. The remaining $2 million will be used to support the Assertive Community Treatment program (ACT), an intensive, voluntary outreach mental health service operated by Vancouver Coastal Health. It supports people in the Downtown Eastside who have severe, persistent mental illness and addiction. "We want to help create a healthier future for the Downtown Eastside," said Chuck Jeannes, president and CEO of Goldcorp. "We're pleased that our donation will enable health care experts to leverage one another's work, and produce a transformational and lasting impact in the lives of Vancouver's most vulnerable residents." The Fellowship in Addiction Medicine will be led by Dr. Evan Wood, co-director of the Urban Health Research Initiative at the BC Centre for Excellence in HIV/AIDS (BC-CfE). It will address a critical lack of skilled addiction medicine specialists in the province and provide training in addiction medicine to 20 post-doctoral fellows over five years. "Addictions treatment in B.C. falls so far short of the need," said Dr. Wood. "A very limited number of physicians in this province are appropriately trained in addiction medicine, making it difficult for vulnerable populations to access much-needed drug and alcohol treatment. "Goldcorp's generous funding for this Fellowship will create the capacity to increase care and create a critical mass of addiction medicine physicians to help make BC a world leader in this area." Dr. Julio Montaner, director of the BC-CfE, noted that the implementation of the BC-CfE-pioneered Treatment as Prevention strategy has been extremely successful in decreasing AIDS-related deaths and disease progression and preventing new HIV infections in the province. In fact, B.C. is the only province in Canada that has shown a consistent decline in new HIV cases. However, he also noted that more needs to be done in the critical area of addiction treatment to continue the fight against HIV and AIDS in this province. "We are very appreciative of Goldcorp's commitment and support for expanded addiction treatment," said Dr. Julio Montaner, director of the BC-CfE. "There is an urgent need for the expansion of evidence-based addiction treatment, especially given the severe social and medical costs stemming from untreated alcohol and drug addiction." | Forecast Newsletter | Download | |||||||||||||||||||||||
| August, 2012 | Rilpivirine-emtricitabine-tenofovir DF (Complera™) & Rilpivirine (Edurant™) | Formulary Addition | Dear Doctor Letter | Download | |||||||||||||||||||||||
| June, 2012 | Jun-12 | STOP HIV/AIDS project links high-risk populations to HIV testing and careBathhouse testing pilot project aims to increase testing and treatment services for men who have sex with men
It's late on a Thursday night, but the sign on the closed door reads, "The nurse is in." A man wearing nothing more than a bath towel wrapped around his waist patiently waits his turn to enter. Techno music throbs unceasingly through the speakers in the dimly lit space. This is Steamworks, a gay bathhouse in Vancouver. It's also where Steven Lofton, an HIV outreach nurse, works. "It's an odd setting, but clients here have often not been connected to care previously," says the Vancouver Coastal Health (VCH) nurse. "These are men who, for a lot of reasons, have traditionally not been getting tested [for HIV] and there's many complications with them accessing health care." Bathhouses are uniquely high-risk settings. Research from the BC Centre for Excellence in HIV/AIDS (BC-CfE) and VCH shows clients are four times more likely to have unprotected sex with an unknown or different status partner than in other populations. And as men who have sex with men represent a disproportionate number of new HIV infections in Vancouver (accounting for over 60 per cent in 2011), it's clear how critical HIV education and testing for this population has become. Lofton led the launch of the Vancouver Bathhouse Testing pilot in 2011 as part of Seek and Treat for Optimal Prevention of HIV/AIDS (STOP HIV/AIDS). STOP HIV/AIDS, a BC-CfE-pioneered concept, is a B.C. government funded, $48-million four-year pilot project. It aims to expand HIV testing and treatment as part of the Treatment as Prevention strategy, to curb the spread of HIV and AIDS. The STOP HIV/AIDS pilot project targets higher risk populations in Vancouver and Prince George, and the Bathhouse Testing pilot has been key in increasing testing and treatment services for men who have sex with men. Lofton notes that bathhouses have played an important role in gay culture for centuries. More recently, they have provided a venue for gay men and other men who have sex with men to share information, socialize, build community and access important health information. Before the pilot launched, however, HIV testing in bathhouses was available, but not always taken advantage of. "The STOP HIV/AIDS pilot project has provided us with the opportunity and resources to carefully examine our HIV testing practices and improve coverage," Lofton explains. Lofton has worked closely with the operators of three bathhouses located in downtown Vancouver to implement clinics for testing and linking newly diagnosed men to care with an eye on creating a space that is visible, welcoming and safe. The bathhouse testing team now provides comprehensive HIV blood work, screening for sexually transmitted infections, referrals and follow-up, treatment, and counselling in a fully set-up clinic embedded in each bathhouse. The success of the Bathhouse Testing pilot is evident: a total of 367 HIV tests were conducted from March 2011 to April 2012, including 18 per cent administered to men who had never before been tested for HIV. Over that same period, 11 new HIV diagnoses were identified (a three per cent positivity rate that exceeds the 0.01 per cent threshold for cost-effectiveness). The upcoming International AIDS 2012 Conference in Washington, D.C. in July will provide an opportunity to present the effectiveness of STOP HIV/AIDS projects under Treatment as Prevention to an international audience. The lesson from STOP HIV/AIDS projects like the Bathhouse Testing pilot is that the projects are targeted, effective and welcomed. | Forecast Newsletter | Download | |||||||||||||||||||||||
| May, 2012 | May-12 | International workshop highlights B.C.'s pioneering role in the fight against HIV/AIDS
B.C. leads in the implementation of Treatment as Prevention to significantly decrease death, disease progression, and new HIV diagnoses in the provinceHundreds of leading international HIV scientists from around the world congregated in Vancouver last month to hear the latest research on HIV prevention at the 2nd International HIV Treatment as Prevention Workshop. HIV researchers and clinicians from Zimbabwe, Kenya, Europe, and Argentina rubbed elbows with representatives from international organizations including the Joint United Nations Programme on HIV/AIDS (UNAIDS), the World Health Organization (WHO), the International AIDS Society (IAS), President's Emergency Plan For AIDS Relief (PEPFAR), and the National Institutes of Health (NIH) during the four-day workshop from April 22-25. In his presentation, Dr. Julio Montaner, director of the BC Centre for Excellence in HIV/AIDS (BC-CfE), told attendees that in British Columbia, progression to AIDS and death, as well as new HIV diagnoses, have decreased significantly as a result of the province's innovative Treatment as Prevention strategy. "The consistent decrease in AIDS-related morbidity and mortality, coupled with the consistent decrease in new HIV diagnoses in B.C., reinforces the effectiveness of Treatment as Prevention," said Dr. Montaner, co-chair of the workshop. He noted new province-wide HIV diagnoses fell again in 2011, to 289 from 301 in 2010, from approximately 900 cases per year in the early 1990s. Treatment as Prevention involves widespread HIV testing and treatment to medically eligible people who are found to be HIV positive. In recognition of the overwhelming evidence that Treatment as Prevention works, the focus of the discussion at the BC-CfE-led workshop was not on the efficacy of the strategy, but rather on how to best put it into action. "The United States government has embraced treatment as a powerful [and] essential tool in prevention and the achievement of an AIDS-free generation," Ambassador Eric Goosby, United States Global AIDS Coordinator, told the audience in his keynote address. "Today, we are privileged to sit at the intersection where the worlds of science and implementation combine to produce significant public health impact." Workshop attendees debated the most cost-effective ways to implement Treatment as Prevention. However, they all agreed that, as the only province in Canada to implement the strategy and see a consistent decline in new HIV cases, B.C. provides a successful model for other Canadian cities and countries across the world. "By developing ground-breaking policies such as Treatment as Prevention, B.C. is making significant inroads against HIV and AIDS and providing best practices to implement in Canada and the rest of the world," said Elly Katabira, president of the IAS and co-chair of the workshop. "We look forward to the day when the battle against HIV and AIDS is finally won." In B.C., the Seek and Treat for Optimal Prevention of HIV/AIDS (STOP HIV/AIDS) pilot project is based on BC-CfE's HIV Treatment as Prevention strategy. In 2010, the B.C. government invested $48 million over four years in the BC-CfE-led STOP HIV/AIDS pilot to expand HIV testing and treatment in Vancouver's inner city and Prince George. Treatment as Prevention has been endorsed by U.S. President Barack Obama and Secretary of State Hillary Clinton as an effective strategy in the fight against HIV/AIDS. They have added their names to a growing list of supporters that includes UNAIDS, WHO, the Clinton Foundation, and the Stephen Lewis Foundation. | Forecast Newsletter | Download | |||||||||||||||||||||||
| April, 2012 | STOP HIV/AIDS Pilot Project Indicators Report - Q4 2011 (PDF) | STOP HIV/AIDS | Download | ||||||||||||||||||||||||
| April, 2012 | Nevirapine Immediate Release (Viramune™ IR) and Nevirapine Extended Release (Viramune™ XR) Tablets | Formulary Addition | Dear Doctor Letter | Download | |||||||||||||||||||||||
| April, 2012 | Apr-12 | BC-CfE, chief provincial medical health officers call for marijuana regulationTop doctors from British Columbia and Nova Scotia urge policy-makers to rethink failed war-on-drugs approach to improve community health and safety
Drs. Kendall and Strang, along with Dr. Evan Wood, co-director of the Urban Health Research Initiative at the BC Centre for Excellence in HIV/AIDS (BC-CfE), published a review paper recently in Open Medicine, a peer-reviewed medical journal. The authors conclude: "In light of the persistently widespread availability and relative safety of cannabis in comparison to existing legal drugs, as well as the crime and violence that exist secondary to prohibition of this drug, there is a need for discussion about the optimal regulatory strategy to reduce the harms of cannabis use while also reducing unintended policy-attributable consequences (e.g., the organized crime that has emerged under prohibition)." Given the overwhelming evidence showing that marijuana prohibition has been a costly 30-year failure, the authors recommend that governments re-evaluate strategies, including mandatory minimum sentences for minor drug offences. Mandatory minimums have proven costly and ineffective in other nations, and the authors note their implementation is "a complete departure from evidence-based policy-making." "The so-called war on drugs has not achieved its stated objective of reducing rates of drug use. Marijuana is universally available in B.C. and the supply is controlled largely by criminal enterprise," said Kendall. "As with tobacco and alcohol, we could devise regulatory frameworks to limit access and harms." Strang cautioned that continuing with the status quo will further increase unintended consequences, such as HIV outbreaks among incarcerated drug users, violence, deaths, broken families and wasted taxpayer dollars. ``If our objective is to minimize drug use, minimize health and social impacts from drug use, we need to be open to having policy and public discussions that look at all aspects and all potential ways to approach this, not just our current ideologically single approach,'' Strang said to Halifax's The Chronicle Herald. Kendall and Strang are adding their voices to a larger public health community in Canada that has called for evidence-based drug policies. Coinciding with the Open Medicine paper, the Urban Public Health Network, which comprises the chief medical health officers of the 18 largest municipalities in Canada, endorsed the Vienna Declaration, a global consensus statement calling for the incorporation of scientific evidence into illicit drug use policies. The Vienna Declaration was initiated by the BC-CfE and unveiled as the official declaration of the 2010 International AIDS Conference in Vienna, Austria. It has since been signed by more than 23,000 people. In recent months, under the Stop the Violence BC campaign, a range of high-profile authorities in B.C. have spoken out in favour of marijuana taxation and regulation including former Vancouver mayors, premiers and provincial attorneys general. | Forecast Newsletter | Download | |||||||||||||||||||||||
| March, 2012 | Mar-12 | BC Centre for Excellence in HIV/AIDS marks two decades of path-breaking research in the fight to end HIV and AIDSBC-CfE celebrates 20 years of success
The event recognized the BC-CfE's incredible medical advancements, which allow people with HIV and AIDS to now lead longer and more fulfilling lives. It also honoured the memories of friends, family members and all British Columbians lost to AIDS. "Through the support of the Government of British Columbia, UBC and Providence Health Care, we have been able to attract committed and qualified individuals who have worked tirelessly to save and improve the lives of people living with HIV and AIDS," said Dr. Julio Montaner, director of the BC-CfE. "This anniversary and the many advancements we have pioneered at the BC-CfE belong not just to the BC-CfE staff, but to all the HIV-positive individuals, the families of the deceased, our community partners and all who have contributed over the years." In a video address, Christy Clark, the Premier of B.C., noted that HIV and AIDS have touched the lives of many people around the world. "In the 1990s, I lost a dear friend of complications from HIV/AIDS, so the advances that B.C. researchers have made in treating this disease mean an awful lot to me," said the Premier. She added that due to the work of the BC-CfE, B.C. is the only province in Canada seeing a consistent decline in new HIV diagnoses. "Tonight I would like to thank Dr. Julio Montaner for his leadership," she said. "He and his dedicated staff have worked incredibly hard and have been recognized around the world as leaders in HIV prevention." As part of the celebrations, his Excellency Werner Brandstetter, Austrian Ambassador to Canada, presented his country's Grand Decoration of Honour to Dr. Montaner for work that has made a significant contribution to combat HIV/AIDS in Austria. The award is a national honour that is conferred by the president of Austria upon individuals who have provided outstanding services or public benefit to the country. At the event, Dr. Montaner recognized long-serving members of the BC-CfE staff for their innovation and dedication to fighting HIV, and helping turn what was once a deadly disease into a chronic, manageable condition. The early days The history of AIDS in B.C. began a decade before the BC-CfE was formed. In 1982, the first patients with AIDS symptoms began showing up at the doors of Vancouver's St. Paul's Hospital. While some hospitals were sending AIDS patients away, St. Paul's threw open its doors to the growing number of people who needed help and brought together a group of committed health care professionals who formed the AIDS Care Team. Despite the establishment of the AIDS Care Team, within a decade of the appearance of the first case of HIV, a British Columbian was dying of the disease almost every day. With little effective treatment to offer, for most the virus was a death sentence. In response, the BC Ministry of Health established the BC-CfE. "When I started in 1984, we had described the virus but we had no treatments. If a person received a diagnosis, it was bad news," recalls Dr. Michael O'Shaughnessy, founding director of the BC-CfE. Under Dr. O'Shaughnessy's leadership, the BC-CfE established the HIV/AIDS Drug Treatment Program, a research and treatment program designed to ensure that all medically eligible persons living with HIV in British Columbia have access to free antiretroviral therapy. The year everything changed In 1996, the concept of combination therapy, known as highly active antiretroviral therapy (HAART), was introduced. Its release coincided with the opening of the 1996 International AIDS Society (IAS) conference in Vancouver. There, new evidence supporting HAART was presented. "In Vancouver, we stood up at the podium to say that this is what the new data showed, that this was the new way forward, that this was the new way to treat HIV," said Dr. Montaner. "It transformed the outcome of this epidemic." Evidence presented at the conference would lead to the immediate introduction of the B.C.-developed HAART as a therapeutic strategy for HIV. Treatment as Prevention Dr. Montaner first introduced the groundbreaking concept of Treatment as Prevention at the Toronto 2006 IAS conference. The strategy called for expanding HIV testing and increased access to HAART to curb the spread of HIV/AIDS. The government of B.C., the first in Canada to support the concept of Treatment as Prevention, announced a $48 million pilot project called Seek and Treat for Optimal Prevention of HIV/AIDS (STOP HIV/AIDS) in 2010. The pilot is aimed at expanding access to treatment among vulnerable and hard-to-reach populations. The Treatment as Prevention strategy to control HIV has gained the support of key international organizations including the Stephen Lewis Foundation, the Clinton Foundation, the World Health Organization (WHO) and the Joint United Nations Program on HIV/AIDS (UNAIDS) "We are blessed to have people of the talent of Julio Montaner and those at the BC-CfE," said Professor Stephen Toope, president of UBC. "People who are passionate, people who are extraordinarily talented and, frankly, people who are courageous in what they choose to undertake in their life's work." Dr. Montaner echoed the sentiments. "I look back with great pride and satisfaction at the far reaching impact our work has had on this devastating disease. However, I know that our work is not yet done." | Sex Work | Forecast Newsletter | Download | ||||||||||||||||||||||
| February, 2012 | Feb-12 | Global gathering for special session of BC-CfE's HIV/Antiretroviral Update Researchers from St. Paul's Hospital and as far away as China meet in Vancouver to discuss HIV strategies
In February 2011, China announced plans to combat HIV and AIDS by implementing a country-wide Treatment as Prevention strategy modelled on the pioneering work of the BC Centre for Excellence in HIV/AIDS (BC-CfE). At the most recent session of the HIV/Antiretroviral Update, a full-day educational event sponsored by the BC-CfE and accredited by the College of Family Physicians of Canada, attendees were able to hear about the progress made since that announcement and the plans now in place to further the nation's fight against HIV/AIDS. In China, it is estimated that 780,000 people are infected with HIV and nearly 154,000 people have AIDS. The country has experienced a rapid rise in both HIV and AIDS from a regional epidemic to a national one in less than a decade. Most troubling, Dr. Yiming Shao explained, is how the reported cases of HIV infection, AIDS and AIDS deaths continue to trend upwards. "More aggressive testing, treatment and intervention programs have been implemented at the moment," Dr. Shao told the audience. "But there remain many challenges." While China has committed to Treatment as Prevention as a cornerstone strategy for the nation, Dr. Shao outlined the unique challenges that the country faces in rolling out the strategy nation-wide. Huge mobile populations (over 220 million), poor health infrastructure in rural areas and unprepared doctors have created a gap between implementing and executing policy. "More than two-thirds of current patients are treated in rural areas, and their doctors have very limited medical and laboratory facilities to support their work," he said. "Mostly these are ‘barefoot' doctors who have difficulty understanding drug-resistance and lack experiences and tools to deal with the side effects." Based on their effective STD (sexually transmitted disease) eradication campaign first introduced in the 1950s, China has recently launched a pilot trial of a holistic approach targeted in their Lianshan prefecture, a remote mountain region with the highest HIV prevalence in the country. At the centre of the plan, called the Rural Economic Enterprise (REE), is providing unemployed HIV-positive people and unemployed drug users with jobs, where they can connect these individuals with treatment on a daily basis. The hope is this will increase adherence to both antiretroviral therapy and other intervention strategies and improve cost-effectiveness of a centralized AIDS program in the region. "Within five years the rate of new infections can be knocked down 50 per cent, and to baseline rates within 10 years with 75 per cent participation," Dr. Shao explained. It was a hopeful outlook on the progress made in China, and one that echoed the positive news delivered by Dr. Julio Montaner, director of the BC-CfE and session chair. Dr. Montaner told the audience that as a result of Treatment as Prevention, AIDS-related morbidity, mortality, and new HIV infections have continued to trend downwards in B.C. "We are impressed with the success in B.C. [in the fight against HIV/AIDS]," Dr. Shao said. "And I think we have many things to learn from you." | Forecast Newsletter | Download | |||||||||||||||||||||||
| January, 2012 | Jan-12 | International acclaim marks breakthrough year for Treatment as PreventionScience and Time among top media to recognize HIV strategy
The December 2011 issue of Science highlighted the 96 per cent prevention of HIV transmission described by the HPTN 052 as the rationale for naming HIV Treatment as Prevention the breakthrough of the year. The study results were reported by Dr. Myron Cohen at the International AIDS Conference in Rome last summer The announcements were made as newly released statistics showed a reduction of nearly 65 per cent in new HIV diagnoses in B.C. in 2010—to 301 cases, down from the 850 cases diagnosed annually prior to 1996. A January 2012 New York Times article noted that as a result of the implementation of the Treatment as Prevention strategy, by the BC Centre for Excellence in HIV/AIDS (BC-CfE), B.C. is showing decreasing trends in AIDS diagnoses and HIV/AIDS mortality. The article also noted that Treatment as Prevention has resulted in B.C. being the only province in Canada to show a decreasing rate of new HIV diagnoses. "B.C. is exceedingly proud of its role in developing, implementing and proving the Treatment as Prevention strategy, and we hope the advancements made and recognition received in 2011 will be a springboard to worldwide implementation," said B.C. Health Minister Michael de Jong. The Treatment as Prevention strategy advocates rapid testing and administration of highly active antiretroviral therapy (HAART) for people who are found to be HIV-positive and medically eligible. HAART reduces HIV in the blood and sexual fluids to undetectable levels. This prevents HIV from progressing to AIDS and reduces the likelihood of HIV transmission by more than 96 per cent. Dr. Myron Cohen led an international team of researchers on the HPTN 052 clinical trial, which was recognized as the breakthrough of 2011 by Science. The trial involved more than 1,700 couples on four continents. Antiretroviral drugs were administered to half of the HIV-positive people and treatment was delayed to the other half. Science described the results of early treatment as "dramatic" in lowering the rate at which the HIV-free partners become infected, while also improving outcomes for the infected partner. "The HPTN 052 trial provides elegant and definitive proof that HAART is the most effective means of preventing HIV transmission", said Dr. Julio Montaner, director of the BC-CfE and one of the pioneers of the Treatment as Prevention strategy. "In addition, HAART allows for the immunity to recover and thereby prevents progression to AIDS and premature death, so that HIV-infected persons are able to lead a near-normal life." Dianne Doyle, president and CEO of Providence Health Care (PHC), applauded the impact that B.C.'s research and advocacy of Treatment as Prevention has had on the lives of patients. "As home to the BC-CfE, PHC is very pleased that our research is contributing to set new standards in the fight against HIV and AIDS globally," said Doyle. Stephen Toope, president and vice-chancellor of the University of British Columbia (UBC) and BC-CfE partner joined Doyle in crediting Treatment as Prevention for revolutionizing HIV patient care in the province of B.C. "An HIV diagnosis in B.C. is no longer a death sentence," said Toope. While Dr. Montaner applauded the global recognition of Treatment as Prevention, he also signaled the need for strong political will to further expand this proven model and win the fight against HIV/AIDS. "The results here in B.C. show that it is possible to bring HIV and AIDS under control using Treatment as Prevention as the cornerstone of our strategy," said Dr. Montaner. "The opportunity is now for us to further this strategy in the rest of Canada and abroad. But it will take leadership and vision from our political leaders to bring about an AIDS-free generation." | Forecast Newsletter | Download | |||||||||||||||||||||||
| December, 2011 | Dec-11 | BC-CfE Treatment as Prevention campaign promotes routine testing in HIVNew ‘Share the Pledge, Take the Test' social media initiative to help end HIV
The campaign calls for sexually active people to ‘Share the Pledge, Take the Test' by pledging to take a voluntary, confidential HIV test and if they choose, share their pledge with their friends. The campaign promotes the BC-CfE-pioneered Treatment as Prevention strategy as the way towards an AIDS-free generation. The launch includes an interactive website, www.treatmentasprevention.ca, where visitors can pledge to take the HIV test, share their pledge if they wish with friends through Facebook and Twitter, and learn about Treatment as Prevention, HIV and AIDS. "The Treatment as Prevention campaign is about creating a social movement to stop the spread of HIV," said Dr. Julio Montaner, director, BC-CfE. "We want to engage people in a dialogue about HIV/AIDS, and provide a venue for them to share their experiences and normalize testing. Testing for HIV is a critical first step to help people stay healthy and prevent further HIV infections in our community and, in the process, help defeat HIV and AIDS." The Treatment as Prevention strategy involves widespread HIV testing and administering anti-HIV drugs known as Highly Active Antiretroviral Therapy (HAART) to medically eligible individuals who are HIV positive. The benefits of HAART are twofold: it reduces the level of HIV in the blood to undetectable levels, improving the health of people with HIV, while also decreasing the level of HIV in sexual fluids to undetectable levels, reducing the likelihood of HIV transmission by more than 95 per cent. Montaner marked the launch of the testing campaign by meeting with the community and providing updates on the Treatment as Prevention strategy at local events and through national media interviews. Speaking at the Dr. Peter Centre to a packed house alongside BC Premier Christy Clark and Dr. Peter AIDS Foundation Executive Director Maxine Davis, Montaner noted the key role played by the BC government in generously funding HIV research and care. He added that Vancouver and BC are now at the forefront of HIV/AIDS innovation, and Treatment as Prevention is endorsed by leading organizations such as the Joint United Nations Programme on HIV/AIDS (UNAIDS) and the Clinton Foundation. "Treatment as Prevention is the new way forward," he said. "We need to do it for the good of our children and we can do it." Clark agreed. "When you think about the savings for those families whose loved ones are now alive today or who are no longer struggling the way that they did before, it's incalculable," she said. Voluntary, confidential testing for HIV will identify and help people with HIV receive the treatment they require. An approximate 2,500 people in British Columbia from all walks of life, have HIV and are not aware of their status. It is critical that testing be implemented province-wide. Vancouver Coastal Health and Providence Health Care have also recently launched a comprehensive social marketing campaign called "It's Different Now" (www.itsdifferentnow.org). The It's Different Now and Treatment as Prevention campaigns are leading efforts in BC to move HIV testing beyond what are considered at-risk groups and into the mainstream. Only through comprehensive programs that normalize HIV testing for all British Columbians will BC optimize efforts and resources to defeat HIV and reach the goal of an AIDS-free generation. | Forecast Newsletter | Download | |||||||||||||||||||||||
| November, 2011 | Nov-11 | Hillary Clinton Endorses BC-CfE's Treatment as Prevention StrategyB.C. Premier Christy Clark lauds call for AIDS-free generation
Secretary Clinton, speaking on November 8 to a global Internet audience, highlighted Treatment as Prevention as part of a combination approach aimed at creating an "AIDS-free generation," in which virtually no children are born with the virus, the risks of becoming infected are dramatically reduced, and people with HIV have access to treatment that prevents them from developing AIDS and passing on the virus to others. "Treating people will not only save lives, it will generate considerable economic returns as well," said Clinton in her speech at the US National Institutes of Health in Washington, D.C., noting that highly active antiretroviral therapy (HAART) allows people with HIV to work, support their families, and contribute to the community. The Treatment as Prevention strategy was developed, modelled and proven by the BC-CfE and publicly introduced by its director, Dr. Julio Montaner, at the International AIDS Society conference in 2006. The strategy advocates for widespread HIV testing and access to free HAART for all medically eligible HIV-positive individuals. HAART decreases the level of HIV in blood and sexual fluids to undetectable levels, improving the health of individuals with HIV and reducing the likelihood of HIV transmission by more than 95 per cent. B.C. Premier Christy Clark lauded Clinton's call for a scaled up Treatment as Prevention strategy based on the BC-CfE's model. "It was British Columbia under the leadership of Dr. Julio Montaner and the BC Centre for Excellence in HIV/AIDS that put the pieces of the puzzle together to realize that expanded treatment could prevent the spread of HIV/AIDS," said Premier Clark. "We are proud to be able to share this effective treatment against the spread of HIV/AIDS with Canada and the world, and look forward to its increased implementation globally resulting from Hillary Clinton's announcement this morning." Montaner provided full support to Hillary Clinton's impassioned call for increased funding to the Global Fund to Fight AIDS, Tuberculosis and Malaria to enable a faster rollout of Treatment as Prevention and other measures to combat HIV globally. "Some emerging powers and nations that are rich in natural resources can afford to give, but choose not to. To sit on the sidelines now would be devastating. It would cost lives," said Clinton. Montaner agreed, and pointed to Canada as a global laggard in funding programs to improve access to HIV therapies in Canada and around the world. "Canada's contributions to the Global Fund remain below the country's stated commitments and far below its ability to pay," Montaner noted. "As a wealthy country with extensive resources, it is time that Canada stepped up to the plate and met its obligations." | Forecast Newsletter | Download | |||||||||||||||||||||||
| October, 2011 | Oct-11 | Supreme Court of Canada rules Insite will remain openLandmark decision heralded as a victory for public health
The unanimous verdict, handed down in Ottawa and relayed quickly to hundreds of people standing outside Insite, ordered the federal health minister to extend an immediate exemption to Insite from federal drug laws and stated that closing Insite would be a violation of the Charter of Rights and Freedoms. "This is a victory for public health over ideology," said Dr. Julio Montaner, director of the BC Centre for Excellence in HIV/AIDS (BC-CfE) and one of the leading researchers of Insite. "It sends a very clear message to Stephen Harper that the time has come for him to abandon his ideology regarding addiction, HIV and other related matters and move on with the evidence." Liz Evans, the executive director of the Portland Hotel Society Community Services, echoed Dr. Montaner. She called the ruling "a giant victory for all of us" during the news conference following the ruling's announcement. "It's been a long journey since we launched the court case," Evans said. "A long journey during which we've been trying to explain to people who don't know or don't know how to care, that there are better ways to embrace people living in our society with addictions than to cast them aside and tell them they are better off dead. Today is a testimony to the remarkable abilities of many people from many sectors coming together to make a significant difference." The ruling noted that the health and safety of Insite's users and the community outweighed any benefit provided by anti-drug laws. "During its eight years of operation, Insite has been proven to save lives with no discernible negative impact on the public safety and health objectives of Canada," the Supreme Court said. "The effect of denying the services of Insite to the population it serves and the correlative increase in the risk of death and disease to injection drug users is grossly disproportionate to any benefit that Canada might derive from presenting a uniform stance on the possession of narcotics." Since the facility opened in 2003, the BC-CfE has conducted significant research into Insite and published several peer-reviewed studies in prestigious international journals. The research shows that Insite delivers many life-saving benefits such as reduced needle-sharing and HIV transmission rates, increased uptake into addiction treatment, and improved public order. In April this year, in a study published in The Lancet, BC-CfE researchers found a 35 per cent reduction in overdose deaths in the immediate vicinity of Insite following its opening. "There is no doubt Insite saves lives," said Dr. Thomas Kerr, co-director of the Addiction and Urban Health Research Initiative, a program of the BC-CfE. As one of the leading researchers of Insite, he noted that there have been about 1,500 overdoses since the facility opened but no one has ever died at Insite. Dr. Evan Wood, co-director of the Addiction and Urban Health Research Initiative, expressed relief with the decision and hoped that the province and federal government can now begin to work together to solve the problems of addiction and HIV infection. "Clearly, Insite is saving tax dollars by helping to reduce the spread of HIV and has the added bonus of channelling people into addiction treatment. With the unanimous Supreme Court decision behind us, hopefully all Canadians will see the benefit of this program and put the legal disagreements behind us." Dr. Patricia Daly – chief medical health officer at Vancouver Coastal Health, which operates Insite in partnership with Portland Hotel Society Community Services – was also on hand to celebrate the top court's ruling. She told The Vancouver Sun that chief medical officers from Canada's 18 largest cities believe in the evidence behind the effectiveness of Insite. Montaner pointed out that that this ruling could open the doors for similar facilities in interested cities across Canada and North America such as Toronto, Montreal and San Francisco. "Insite is a successful example of harm reduction and a key way to implement the BC-CfE-pioneered Treatment as Prevention strategy," said Montaner. "When you create opportunities for people to be tested for HIV and access treatment, you are not only helping them get better, but also ensuring that they become dramatically less likely to transmit the virus, thus protecting the community as well." B.C.'s provincial government has supported Insite and other innovative harm reduction initiatives to effectively address the harms associated with illicit drug use and combat HIV infection and transmission. Last year, the B.C. Liberals announced the expenditure of $48 million to seek out and reach people in marginalized populations, such as injection drug users, to test them for HIV and enroll those infected in treatment. The pilot Seek and Treat for Optimal Prevention of HIV/AIDS (STOP HIV/AIDS) is currently underway in Vancouver's inner city and Prince George.
| Forecast Newsletter | Download | |||||||||||||||||||||||
| September, 2011 | STOP HIV/AIDS Pilot Project Indicators Report - Q3 2011 (PDF) | Seek and Treat, STOP HIV/AIDS | Download | ||||||||||||||||||||||||
| September, 2011 | VCH-PHC STOP HIV/AIDS Funding | Seek and Treat, STOP HIV/AIDS | Download | ||||||||||||||||||||||||
| September, 2011 | BC-CfE STOP HIV/AIDS¨ Funding | Seek and Treat, STOP HIV/AIDS | Download | ||||||||||||||||||||||||
| September, 2011 | Northern Health Authority STOP HIV/AIDS Funding | Seek and Treat, STOP HIV/AIDS | Download | ||||||||||||||||||||||||
| September, 2011 | PHSA STOP HIV/AIDS Funding | Seek and Treat, STOP HIV/AIDS | Download | ||||||||||||||||||||||||
| September, 2011 | Sep-11 | BC-CfE-led STOP HIV/AIDS pilot transforms approach to HIV testingRoutine HIV testing will help find those unaware of their infection
Chris Buchner, regional director of prevention at Vancouver Coastal Health (VCH) explained that for many years we have focused almost exclusively on targeted testing of high-risk populations. While successful in diagnosing some, the status quo approach also has some important limitations, including too many late diagnoses, and thus, inferior health outcomes and potentially less impact on curbing transmission. "STOP has provided us with an opportunity to significantly re-evaluate the way we approach HIV testing," said Buchner. "What is needed is to make HIV testing a routine part of health care." Provincial recommendations for HIV testing were modified last year to recommend an annual HIV test for all sexually active adults. Building on this recommendation, VCH and Providence Health Care (PHC) have launched several initiatives to increase opportunities for testing. Among them, in October this year, they will launch an acute care testing pilot in Vancouver hospitals where patients will be offered an HIV test upon admission to key programs. VCH and PHC have also escalated efforts to increase access to HIV testing for high-risk populations. Among them, nurses are collaborating with community partners on the introduction of a HIV testing pilot involving peers in the Downtown Eastside. And HIV testing has been increased for Aboriginal people at the Vancouver Native Health Society. As a result of these efforts, there were 7,482 HIV tests conducted in Vancouver in August 2011. That is the highest monthly total in many years, according to statistics from the BC Centre for Disease Control (BCCDC). Northern Health (NH), VCH and PHC manage the regional implementation of the pilot with support from the Provincial Health Services Authority (PHSA), including the BCCDC and BC Women's Hospital, under the leadership of the BC Centre for Excellence in HIV/AIDS (BC-CfE). Dr. Susan MacDonald, Northern Interior Medical Director of NH, provided highlights of the progress made by NH in implementing the STOP HIV/AIDS pilot. She said NH has appointed an HIV-dedicated pharmacist to provide education about highly active antiretroviral therapy (HAART) to HIV-positive individuals in person or by telehealth (audio and video conferencing) for those living outside Prince George. In partnership with the Northern Aboriginal HIV/AIDS Task Force and Public Health, NH has conducted discussions over the past year with the leadership of the First Nations communities in the north to gain valuable information about community readiness and ways to offer culturally sensitive HIV testing and care. PHSA has also been delivering on key STOP HIV/AIDS goals. Dr. Gina Ogilvie, medical director of clinical prevention services at BCCDC said that PHSA is currently providing point of care HIV testing directly at BCCDC-operated clinics treating sexually transmitted infections and is delivering test kits to other community sites throughout B.C. STOP HIV/AIDS is a four-year, $48-million pilot project that was launched by the B.C. government in 2009. It is currently underway in Vancouver's inner city and Prince George, expanding rapid testing and access to HAART to hard-to-reach populations such as injection drug users and sex trade workers. The pilot is based on the BC-CfE-pioneered groundbreaking Treatment as Prevention strategy, which advocates for increased testing and expansion of HAART, both to prevent HIV from progressing to AIDS in individuals and to dramatically reduce new HIV diagnoses in the community. | STOP HIV/AIDS | Forecast Newsletter | Download | ||||||||||||||||||||||
| August, 2011 | STOP HIV/AIDS Pilot Project Indicators Report - Q2 2011 (PDF) | Seek and Treat, STOP HIV/AIDS | Download | ||||||||||||||||||||||||
| August, 2011 | July/August 2011 | HIV Leaders Advance Treatment as Prevention at IAS 2011BC-CfE-pioneered treatment strategy gathers momentum at global conference
The convention – which attracted more than 7,000 of the world's foremost HIV researchers, scientists and doctors to Rome, Italy from July 17-20 – saw leading figures in the global fight against HIV endorse Treatment as Prevention and recognize the central role that the BC Centre for Excellence in HIV/AIDS and its director, Dr. Julio Montaner, have taken in developing the strategy. "Julio has been talking about Treatment as Prevention for a very long period of time," said Dr. Anthony Fauci, MD and director, the U.S. National Institute of Allergy and Infectious Diseases (NIAID). "Now we have absolute confirmed data that he was right all along … " "The idea of the tension between Treatment and Prevention, we should just forget about it … because Treatment is Prevention." The Treatment as Prevention strategy advocates for widespread HIV testing and facilitated access to free HIV treatment for all medically eligible HIV-positive individuals. Current HIV treatment reduces the amount of HIV in the blood to undetectable levels, thus improving the health of HIV-positive individuals. At the same time, the treatment decreases the amount of HIV in sexual fluids to undetectable levels, thereby reducing the likelihood of HIV transmission by over 90 per cent. Immediately prior to the conference, The Lancet, a leading global medical journal, published an editorial comment by Dr. Montaner that emphasizes the critical role of expanding access to HIV treatment under a global Treatment as Prevention strategy to stop the HIV pandemic. Based on the effectiveness of highly active antiretroviral therapy (HAART) in reducing transmission of HIV, Dr. Montaner called on the international community to support an immediate and expanded roll-out of HAART. "The evidence is clear: treatment conclusively prevents morbidity, mortality and transmission," wrote Dr. Montaner. "The challenge remains to optimize the impact of this valuable intervention. Failure to do so is not an option." Support for Dr. Montaner's message was immediate and encouraging. "Treatment as Prevention is one of the most important and promising additions to the range of prevention strategies available to us today," said Dr. Elly Katabira, president of the IAS and Chair of IAS 2011. "Dr. Montaner's column is a rallying call for the universal endorsement and funding of this approach for the benefit of our future generations." A recent study by the U.S. National Institutes of Health (NIH) reported that immediate use of HAART led to a 96 per cent decrease in the risk of HIV transmission among heterosexual couples where one partner is HIV positive. "These results are a real scientific breakthrough and a game changer in the response to HIV," said Michel Sidibé, executive director of the Joint United Nations Programme on HIV/AIDS (UNAIDS). "We must embrace Treatment as Prevention as part of a combination prevention strategy to achieve our collective vision of zero new infections and zero AIDS-related deaths." | International Program, STOP HIV/AIDS | Treatment as Prevention® | Forecast Newsletter | Download | |||||||||||||||||||||
| July, 2011 | STOP HIV/AIDS Update (Spring/Summer 2011) | Seek and Treat for Optimal Prevention of HIV/AIDS (STOP HIV/AIDS) will will expand access to HIV/AIDS medications among hard-to-reach and vulnerable populations in Vancouver’s inner city and Prince George. For more information on STOP HIV/AIDS, including updates on progress, please refer to our quarterly bulletin. The third edition is now available for download in PDF format. | Seek and Treat, STOP HIV/AIDS | Treatment as Prevention¨ | Download | ||||||||||||||||||||||
| July, 2011 | Drug Treatment Program Update (May 2011) | A key component of the Centre’s mandate is to monitor the impact of HIV/AIDS on British Columbia. The BC-CfE provides essential information to local health authorities, treating physicians and the community-at-large on an ongoing basis. The Drug Treatment Program Update is one example of the Centre’s commitment to improving health outcomes for HIV-positive individuals living in B.C. In B.C., all anti-HIV medications are distributed at no cost to eligible HIV-infected individuals through the Centre’s Drug Treatment Program (DTP). The DTP Update provides an important overview of available anti-HIV drugs, common drug combinations and distribution of active DTP participants throughout the province. DTP participants are typically followed at three-monthly intervals at which time routine blood sampling is performed. Information from all recipients is entered into a database, providing data for clinical and virological outcome studies of patients receiving antiretroviral therapy. These studies form the basis of ongoing revisions to the Centre’s treatment guidelines. | Drug Treatment Program | Download | |||||||||||||||||||||||
| June, 2011 | SAFETY ALERT: DARUNAVIR (PREZISTA TM) | June 6, 2011 - The Pharmacovigilance Program at the BC Centre for Excellence in HIV/AIDS has reviewed the following incident: On May 11, 2011, Janssen Inc. issued an advisory that some bottles of darunavir (Prezista TM) 600 mg tablets in Lot # ALZ0J00 might have an uncharacteristic "musty" or "mouldy" odour caused by trace quantities of the wood preservative by-product 2,4,6,tribromoanisole (TBA). Health Canada has advised the manufacturer that a product recall is NOT REQUIRED because there is no known safety risk associated with the odour-causing agent. Persons who take darunavir should continue to take their medication. Based on available information, the affected batch of darunavir tablets is safe for consumption and there is no requirement to return product or recall patients for clinical assessment. As a precautionary measure, darunavir tablets from Lot # ALZ0J00, or any darunavir tablets with an uncharacteristic odour that were dispensed in BC may be voluntarily returned to St Paul’s Hospital Ambulatory Pharmacy and exchanged for new product. | Pharmacovigilance Initiative, Quality and Safety | HIV Clinical Care | Download | ||||||||||||||||||||||
| June, 2011 | Jun-11 | World leaders identify key targets in battle against HIV/AIDSDeclaration calls on UN member states to achieve universal access by 2015
"I congratulate the UN on making this much-needed contribution to combating the HIV and AIDS pandemic around the world, and setting measurable near-term targets that can and must be met," said Dr. Montaner. "This declaration provides strong momentum for universal access to HIV treatment, which will help those suffering from HIV lead fulfilling lives and dramatically reduce further transmission of the virus." | Forecast Newsletter | Download | |||||||||||||||||||||||
| May, 2011 | Drug Treatment Program Update (April 2011) | A key component of the Centre’s mandate is to monitor the impact of HIV/AIDS on British Columbia. The BC-CfE provides essential information to local health authorities, treating physicians and the community-at-large on an ongoing basis. The Drug Treatment Program Update is one example of the Centre’s commitment. In B.C., all anti-HIV medications are distributed at no cost to eligible HIV-infected individuals through the Centre’s Drug Treatment Program (DTP). The DTP Update provides an important overview of available anti-HIV drugs, common drug combinations and distribution of active DTP participants throughout the province. DTP participants are typically followed at three-monthly intervals at which time routine blood sampling is performed. Information from all recipients is entered into a database, providing data for clinical and virological outcome studies of patients receiving antiretroviral therapy. These studies form the basis of ongoing revisions to the Centre’s treatment guidelines. | Drug Treatment Program | HIV Clinical Care | Download | ||||||||||||||||||||||
| May, 2011 | May-11 | International workshop highlights made-in-B.C. prevention strategyWorld's top researchers review evidence for Treatment as Prevention
| Forecast Newsletter | Download | |||||||||||||||||||||||
| April, 2011 | Drug Treatment Program Update (March 2011) | A key component of the Centre’s mandate is to monitor the impact of HIV/AIDS on British Columbia. The BC-CfE provides essential information to local health authorities, treating physicians and the community-at-large on an ongoing basis. The Drug Treatment Program Update is one example of the Centre’s commitment. In B.C., all anti-HIV medications are distributed at no cost to eligible HIV-infected individuals through the Centre’s Drug Treatment Program (DTP). The DTP Update provides an important overview of available anti-HIV drugs, common drug combinations and distribution of active DTP participants throughout the province. DTP participants are typically followed at three-monthly intervals at which time routine blood sampling is performed. Information from all recipients is entered into a database, providing data for clinical and virological outcome studies of patients receiving antiretroviral therapy. These studies form the basis of ongoing revisions to the Centre’s treatment guidelines. | Drug Treatment Program | Download | |||||||||||||||||||||||
| April, 2011 | Drug Treatment Program Update (February 2011) | A key component of the Centre’s mandate is to monitor the impact of HIV/AIDS on British Columbia. The BC-CfE provides essential information to local health authorities, treating physicians and the community-at-large on an ongoing basis. The Drug Treatment Program Update is one example of the Centre’s commitment. In B.C., all anti-HIV medications are distributed at no cost to eligible HIV-infected individuals through the Centre’s Drug Treatment Program (DTP). The DTP Update provides an important overview of available anti-HIV drugs, common drug combinations and distribution of active DTP participants throughout the province. DTP participants are typically followed at three-monthly intervals at which time routine blood sampling is performed. Information from all recipients is entered into a database, providing data for clinical and virological outcome studies of patients receiving antiretroviral therapy. These studies form the basis of ongoing revisions to the Centre’s treatment guidelines. | Drug Treatment Program | Download | |||||||||||||||||||||||
| April, 2011 | STOP HIV/AIDS Pilot Project Indicators Report - Q1 2011 (PDF) | Seek and Treat, STOP HIV/AIDS | Treatment as Prevention¨ | Download | |||||||||||||||||||||||
| April, 2011 | Apr-11 | UN recommends made-in-BC strategy to reshape global AIDS responseSecretary-General's report calls for linkage of treatment and prevention
The report, released last month by Secretary-General Ban Ki-moon, outlines recommendations to help countries achieve universal access to HIV services and reach the goals of zero new HIV infections, discrimination, and AIDS-related deaths. Among its recommendations, the report calls for further integration of HIV prevention and treatment to effectively curb transmission. "Emerging evidence of the important prevention benefits of antiretroviral therapy, which lowers viral load and thereby reduces the infectiousness of people living with HIV, merely underscores the need to link prevention and treatment efforts," the report states. A compelling body of evidence assembled by BC-CfE director Dr. Julio Montaner and colleagues has demonstrated that dramatic decreases in HIV transmission are achieved by expanding access to highly active antiretroviral therapy (HAART) as part of a comprehensive approach to HIV prevention. Drawing on this evidence, the UN report calls for the expansion of HIV treatment to 13 million people among six global targets for 2015. The report also targets:
"The evidence is clear: HIV treatment is HIV prevention," said Dr. Montaner. "If we are to arrest the global spread of HIV and AIDS, we must fully commit ourselves to ensuring universal access to treatment for the millions in need. The recommendations contained in this report represent a vital step towards achieving this critical milestone." The report, submitted in advance of the upcoming UN General Assembly High Level Meeting on AIDS, represents an important opportunity to evaluate achievements and gaps in the global AIDS response. "Thirty years into the epidemic, it is imperative for us to re-energize the response today for success in the years ahead by embracing bold new approaches to HIV prevention," said Michel Sidibé, executive director of UNAIDS. Treatment as Prevention has been endorsed previously by a broad range of international policy leaders, including the World Health Organization, the International AIDS Society, and UNAIDS. In addition to its role in the global response to HIV, the Treatment as Prevention model has been instrumental in reducing new infections in B.C. A recent report by Provincial Health Officer Dr. Perry Kendall, based on key research findings by the BC-CfE, showed that new HIV infections fell by 52 per cent among injection drug users between 1996 and 2009 in response to a significant increase in HAART coverage. | Harm Reduction, Treatment as Prevention® | Forecast Newsletter | Download | ||||||||||||||||||||||
| March, 2011 | Drug Treatment Program Update (January 2011) | A key component of the Centre’s mandate is to monitor the impact of HIV/AIDS on British Columbia. The BC-CfE provides essential information to local health authorities, treating physicians and the community-at-large on an ongoing basis. The Drug Treatment Program Update is one example of the Centre’s commitment. In B.C., all anti-HIV medications are distributed at no cost to eligible HIV-infected individuals through the Centre’s Drug Treatment Program (DTP). The DTP Update provides an important overview of available anti-HIV drugs, common drug combinations and distribution of active DTP participants throughout the province. DTP participants are typically followed at three-monthly intervals at which time routine blood sampling is performed. Information from all recipients is entered into a database, providing data for clinical and virological outcome studies of patients receiving antiretroviral therapy. These studies form the basis of ongoing revisions to the Centre’s treatment guidelines. | Drug Treatment Program | Download | |||||||||||||||||||||||
| March, 2011 | Mar-11 | China chooses made-in-BC approach to combat HIV and AIDS worldwideWorld's most populous nation embraces treatment as prevention
"We believe that treatment as prevention is the model of care and containment that will best help China meet its goal of bringing HIV and AIDS under control by 2015," said Dr. Zunyou Wu, director, National Center for AIDS/ STD Control and Prevention, Chinese Center for Disease Control and Prevention. The new policy will call for widespread HIV testing and treatment for all medically eligible individuals to address the significant HIV/AIDS epidemic in China. The program is based on the results of BC-CfE's research published last summer in The Lancet. Research results showed that administering highly active antiretroviral therapy (HAART) to HIV-positive individuals not only extends their life expectancy, but also makes them dramatically less likely to transmit HIV to others in the community and reduces healthcare costs in the long term. "This would be the first time that an initiative of this nature is undertaken at the national level by a country that certainly has significant challenges regarding the size of the problem [HIV/AIDS] and other social and cultural complexities," said Dr. Julio Montaner, director of the BC-CfE and pioneer of the treatment as prevention strategy. This strategy has been endorsed internationally by WHO and UNAIDS. Montaner noted that with this announcement, the Chinese government has sent a clear message that treatment as prevention makes sense for a crosssection of people all over the world. In China, a reported 740,000 people are infected with HIV and nearly 110,000 people have AIDS. Montaner was first introduced to Wu's tremendous work on the expansion of medical programs in China by Dr. Nora Volkow, director of the National Institute on Drug Abuse. This was followed by discussions at last summer's International AIDS Conference in Vienna, which eventually led to a visit by a Chinese delegation headed by Wu to the BC-CfE last year. During the two-day workshop, the BC-CfE introduced the delegation to the different components of the treatment as prevention model, how it has worked in B.C. and helped develop potential protocols that could be used in the implementation of a similar program in China. The workshop was also attended by former Premier Gordon Campbell to provide support from the B.C. government to the BC-CfE in their efforts to help China combat HIV in their country. B.C. is the first jurisdiction to implement treatment as prevention. In 2010, the B.C. government announced it would invest $48 million over four years in the BC-CfE-led Seek and Treat pilot project to expand HIV testing and treatment to hard-to-reach individuals in Vancouver's Downtown Eastside and Prince George. | Harm Reduction, Treatment as Prevention® | Forecast Newsletter | Download | ||||||||||||||||||||||
| February, 2011 | PowerPoint Slides: October 26, 2010 HIV Diagnosis and Management Update | The first BC-CfE HIV Diagnosis and Management Update took place on October 26, 2010. This educational event is part of a series of initiatives that the BC-CfE is conducting to support primary care providers who wish to improve their skills in the management of HIV-positive individuals. Please click on the presentations below to download slides.
| Clinical Education & Training | ||||||||||||||||||||||||
| February, 2011 | Drug Treatment Program Update (December 2010) | A key component of the Centre’s mandate is to monitor the impact of HIV/AIDS on British Columbia. The BC-CfE provides essential information to local health authorities, treating physicians and the community-at-large on an ongoing basis. The Drug Treatment Program Update is one example of the Centre’s commitment. In B.C., all anti-HIV medications are distributed at no cost to eligible HIV-infected individuals through the Centre’s Drug Treatment Program (DTP). The DTP Update provides an important overview of available anti-HIV drugs, common drug combinations and distribution of active DTP participants throughout the province. DTP participants are typically followed at three-monthly intervals at which time routine blood sampling is performed. Information from all recipients is entered into a database, providing data for clinical and virological outcome studies of patients receiving antiretroviral therapy. These studies form the basis of ongoing revisions to the Centre’s treatment guidelines. | Drug Treatment Program | Download | |||||||||||||||||||||||
| January, 2011 | PowerPoint Presentation: Home is where the HAART is: Factors affecting neighbourhood perception for people living with HIV/AIDS | "Home is where the HAART is: An examination of the factors affecting neighbourhood perception for people living with HIV/AIDS" (PowerPoint Presentation) Author: Drug Treatment Program BC Centre for Excellence in HIV/AIDS
Objectives:
| Drug Treatment Program, LISA | ||||||||||||||||||||||||
| January, 2011 | PowerPoint Presentation: Patient Comprehension of Antiretroviral Drug Resistance: Implications for Treatment and Clinical Practice |
"Patient Comprehension of Antiretroviral Drug Resistance: Implications for Treatment and Clinical Practice" (PowerPoint Presentation) Author: Catherine Sarai Racey Objective: To determine the current level of Knowledge of HIV drug resistance in a cohort of HIV+ people on HAART
| Drug Treatment Program, LISA | ||||||||||||||||||||||||
| January, 2011 | Poster: Prevalence and Correlates of Food Insecurity in Individuals Receiving ART | Background:Food insecurity is defined as having “uncertain or limited availability of nutritionally adequate or safe food or the inability to procure food in socially acceptable ways”(1). An increasing number of studies suggest that high number of people living with HIV/AIDS are food insecure in North America (2-4). Studies conducted in San Francisco in the United States, and in British Columbia in Canada, suggest that food insecure individuals receiving highly active antiretroviral therapy (HAART) have reduced body mass index (BMI), lowered CD4 cell counts, decreased rates of virological suppression and higher case fatality. Authors: A Anema, E Druyts, SD Weiser, KA Fernandes, EK Brandson, JSG Montaner, RS Hogg. | Drug Treatment Program, Epidemiology and Population Health, LISA | ||||||||||||||||||||||||
| January, 2011 | Poster: The Role of Stable Housing and Food Security in Treatment Success Among People on HAART | Background:The HIV epidemic in Canada is increasingly affecting marginalised groups. While highly active antiretroviral therapy (HAART) is freely available to those eligible, socioeconomic barriers too frequently prevent marginalised individuals from accessing therapy. There are known links between the physical and social attributes of neighbourhoods, perception of neighbourhood attributes, health status and health-related risk behaviours. The objective of this study was to determine the impact of stable housing, food security -- two critical neighbourhood issues in British Columbia along with other sociodemographic and clinical variables, on perception of neighbourhood among people receiving HAART. Authors: K Vasarhelyi, EK Brandson, AK Palmer, K Fernandes, W Zhang, E Druyts, JS Montaner, RS Hogg | Drug Treatment Program, Epidemiology and Population Health, LISA | Download | |||||||||||||||||||||||
| January, 2011 | Research Summary: Factors Related to Neighborhood Perceptions Among People Taking Treatment for HIV | Download the Research Summary (PDF) Download the PowerPoint Presentation
| Drug Treatment Program, LISA | ||||||||||||||||||||||||
| January, 2011 | Research Summary: Food Insecurity Common Among People Receiving Treatment for HIV in British Columbia | Download the Research Summary (PDF)
| Drug Treatment Program, LISA | ||||||||||||||||||||||||
| January, 2011 | Drug Treatment Program Update (November 2010) | A key component of the Centre’s mandate is to monitor the impact of HIV/AIDS on British Columbia. The BC-CfE provides essential information to local health authorities, treating physicians and the community-at-large on an ongoing basis. The Drug Treatment Program Update is one example of the Centre’s commitment. In B.C., all anti-HIV medications are distributed at no cost to eligible HIV-infected individuals through the Centre’s Drug Treatment Program (DTP). The DTP Update provides an important overview of available anti-HIV drugs, common drug combinations and distribution of active DTP participants throughout the province. DTP participants are typically followed at three-monthly intervals at which time routine blood sampling is performed. Information from all recipients is entered into a database, providing data for clinical and virological outcome studies of patients receiving antiretroviral therapy. These studies form the basis of ongoing revisions to the Centre’s treatment guidelines. | Drug Treatment Program | Download | |||||||||||||||||||||||
| January, 2011 | Jan-11 | Gordon Campbell honoured for commitment to HIV and AIDS researchPremier's personal and financial support leads to key advances Speaking to an appreciative audience at the Fall 2010 HIV/Antiretroviral (ARV) Update, hosted by the BC Centre for Excellence in HIV/AIDS (BC-CfE), Premier Gordon Campbell lauded the benefits of expanding HIV treatment and thanked hundreds of people in attendance for leading the fight against HIV and AIDS. Premier Campbell told the researchers, healthcare professionals, doctors and community members gathered in the Sheraton Wall Centre Hotel on December 3 that saving lives and improving health are the core reasons behind his support for Seek and Treat, a $48-million, four-year pilot program to expand highly active antiretroviral therapy (HAART) in Prince George and Vancouver's inner city. "I believe that this is a life-saving treatment that will be used in jurisdictions around the world in the years ahead," said Campbell. "It will increase access to HIV testing and help link patients to community-based support services, which are critically important in terms of the quality of life and the health of the individuals we're seeking to serve. And it will save hundreds of millions of dollars in averted health care costs." Campbell said that he and his colleagues in the B.C. government are grateful for the BC-CfE's treatment advances and the work done by community members helping those with HIV and AIDS. "Let me say a big thank you to all of you who are part of the leading edge of our fight against HIV/AIDS, who work day-in and day-out," said Campbell. "I can tell you the voices that we hear from across the province, and the voices we hear from around the world, are saying that British Columbia is on the leading edge of dealing with this issue. We all take great pride in what you're doing." Dr. Julio Montaner, Director, BC-CfE, thanked the Premier for his important role in funding and personally supporting the BC-CfE and many of the advances in treatment that have been achieved so far. "If it were not for the Premier's support over the last decade, we would not be in the position that we are, so he deserves a lot of credit for knowing how to listen and ultimately how to lead," said Dr. Montaner. Dr. Montaner noted a list of new initiatives undertaken in the province and supported by the Province of B.C.: enhanced new testing guidelines, implementation steps to support the Seek and Treat pilot, and expansion of a 1-800 line to help physicians, primary care providers and other caregivers access support and services. He also noted the Premier's leadership on health, finances, Aboriginal relations and climate change. Dr. Montaner presented the Premier with a gift that emphasized the BC-CfE's appreciation for the Premier's personal and financial support in the fight against HIV and AIDS – an iconic Tiko Kerr painting of St. Paul's Hospital. | Forecast Newsletter | Download | |||||||||||||||||||||||
| December, 2010 | STOP HIV/AIDS Pilot Project Indicators Report - Q4 2010 (PDF) | STOP HIV/AIDS | Treatment as Prevention¨ | Download | |||||||||||||||||||||||
| November, 2010 | Drug Treatment Program Update (October 2010) | A key component of the Centre’s mandate is to monitor the impact of HIV/AIDS on British Columbia. The BC-CfE provides essential information to local health authorities, treating physicians and the community-at-large on an ongoing basis. The Drug Treatment Program Update is one example of the Centre’s commitment. In B.C., all anti-HIV medications are distributed at no cost to eligible HIV-infected individuals through the Centre’s Drug Treatment Program (DTP). The DTP Update provides an important overview of available anti-HIV drugs, common drug combinations and distribution of active DTP participants throughout the province. DTP participants are typically followed at three-monthly intervals at which time routine blood sampling is performed. Information from all recipients is entered into a database, providing data for clinical and virological outcome studies of patients receiving antiretroviral therapy. These studies form the basis of ongoing revisions to the Centre’s treatment guidelines. | Drug Treatment Program | Download | |||||||||||||||||||||||
| November, 2010 | STOP HIV/AIDS Update (Fall 2010) | Seek and Treat for Optimal Prevention of HIV/AIDS (STOP HIV/AIDS) will will expand access to HIV/AIDS medications among hard-to-reach and vulnerable populations in Vancouver’s inner city and Prince George. For more information on STOP HIV/AIDS, including updates on progress, please refer to our quarterly bulletin. The second edition is now available for download in PDF format. | Seek and Treat, STOP HIV/AIDS | Treatment as Prevention¨ | Download | ||||||||||||||||||||||
| November, 2010 | Nov-10 | Dr. Julio Montaner honoured for leadership and success fighting HIV/AIDS
The recognitions he has received are provincial, national, and international in scope, including the Order of British Columbia, the highest honour the province of B.C. can bestow on individuals in the province. On October 13, Providence Health Care (PHC) and St. Paul's Hospital Foundation co-hosted a special event in honour of Dr. Montaner to celebrate his decades of leadership, life-saving contributions and global vision in the fight against HIV/AIDS. Guests including friends, colleagues, government leaders, community partners and people living with HIV/AIDS gathered in the Conway Room at Vancouver's Shangri-La Hotel to thank Dr. Montaner for his years of service. "I'm proud you are doing this today for Julio," said Health Services Minister Kevin Falcon in his speech at the event. "For nearly three decades, Julio has stood at the forefront of HIV/AIDS treatment and he has impacted millions around the world in that role." Minister Falcon recalled his first introduction to Dr. Montaner, one of the first meetings he had as Health Services Minister. "He was very compelling in terms of the great work that's being done in British Columbia, and that's why we decided to add $48 million for the Seek and Treat program to ensure that the hard-to-reach populations get the care and treatment they need for HIV/AIDS." Dianne Doyle, president and CEO of PHC, has seen Dr. Montaner grow from his days as a young clinician at St. Paul's Hospital 30 years ago to his leading international role today. "Early in the 1980s, when the HIV/AIDS epidemic was first hitting the city of Vancouver, no one really understood the disease, its transmission, or the significant impact it would have on the health of the population of British Columbia. Julio and his colleagues were early to step up to the plate to lend their expertise to the investigation of this disease and the treatment of it," said Doyle. Dr. Montaner expressed his gratitude and emphasized the support that he and the BC-CfE have received from their peers and the provincial government. "I will forever cherish and be humbled by this recognition," said Dr. Montaner. "But I could not have done this alone. Throughout my career, I have had the good fortune to work with passionate, dedicated and talented people at the BC-CfE, within the health and research community, and the provincial government who have fought against all odds to improve the lives of people living with HIV/AIDS." Among his many accomplishments, Dr. Montaner, with his team of researchers at the BC-CfE played a key role in pioneering highly active antiretroviral therapy (HAART), which has been adopted as the gold standard treatment for HIV around the world. And recently, Dr. Montaner's lifesaving concept of "treatment as prevention" was cited by the Joint United Nations Programme on HIV/AIDS (UNAIDS) as the basis for their radical new approach to HIV treatment, dubbed "Treatment 2.0." In a tribute video shown at the congratulatory event, Françoise Barré-Sinoussi, Nobel Laureate and co-discoverer of HIV, said: "Julio not only have you achieved excellent and pioneering work in the field of HIV treatment and prevention, but your research has always been guided by a high sense of solidarity and social justice for the benefit of all. As an engaged scientist, you truly are an example for all generations of researchers." In further recognition of his work, Dr. Montaner received the Order of British Columbia in a ceremony held in the ballroom of Government House in Victoria on October 21. Dignitaries representing the public sector, industry, academia, First Nations, sport, philanthropy and science attended the event. In addition, Dr. Montaner was recently named recipient of the 2010 "Albert Einstein" World Award of Science by the World Cultural Council, an international organization based in Mexico. Dr. Montaner was chosen for this honour for his relentless advancements in the treatment and prevention of HIV/AIDS since the early 1980s and for providing global leadership in establishing new strategies to defeat the epidemic. And, in November this year, Montaner received the 2010 Prix Galien Canada award, which is the most prestigious award, referred to as the "Nobel Prize" in the field of Canadian pharmaceutical research and innovation. | Forecast Newsletter | Download | |||||||||||||||||||||||
| October, 2010 | Drug Treatment Program Update (September 2010) | A key component of the Centre’s mandate is to monitor the impact of HIV/AIDS on British Columbia. The BC-CfE provides essential information to local health authorities, treating physicians and the community-at-large on an ongoing basis. The Drug Treatment Program Update is one example of the Centre’s commitment. In B.C., all anti-HIV medications are distributed at no cost to eligible HIV-infected individuals through the Centre’s Drug Treatment Program (DTP). The DTP Update provides an important overview of available anti-HIV drugs, common drug combinations and distribution of active DTP participants throughout the province. DTP participants are typically followed at three-monthly intervals at which time routine blood sampling is performed. Information from all recipients is entered into a database, providing data for clinical and virological outcome studies of patients receiving antiretroviral therapy. These studies form the basis of ongoing revisions to the Centre’s treatment guidelines. | Drug Treatment Program | Download | |||||||||||||||||||||||
| October, 2010 | Drug Treatment Program Update (August 2010) | A key component of the Centre’s mandate is to monitor the impact of HIV/AIDS on British Columbia. The BC-CfE provides essential information to local health authorities, treating physicians and the community-at-large on an ongoing basis. The Drug Treatment Program Update is one example of the Centre’s commitment. In B.C., all anti-HIV medications are distributed at no cost to eligible HIV-infected individuals through the Centre’s Drug Treatment Program (DTP). The DTP Update provides an important overview of available anti-HIV drugs, common drug combinations and distribution of active DTP participants throughout the province. DTP participants are typically followed at three-monthly intervals at which time routine blood sampling is performed. Information from all recipients is entered into a database, providing data for clinical and virological outcome studies of patients receiving antiretroviral therapy. These studies form the basis of ongoing revisions to the Centre’s treatment guidelines. | Drug Treatment Program | Download | |||||||||||||||||||||||
| September, 2010 | Drug Treatment Program Update (July 2010) | A key component of the Centre’s mandate is to monitor the impact of HIV/AIDS on British Columbia. The BC-CfE provides essential information to local health authorities, treating physicians and the community-at-large on an ongoing basis. The Drug Treatment Program Update is one example of the Centre’s commitment. In B.C., all anti-HIV medications are distributed at no cost to eligible HIV-infected individuals through the Centre’s Drug Treatment Program (DTP). The DTP Update provides an important overview of available anti-HIV drugs, common drug combinations and distribution of active DTP participants throughout the province. DTP participants are typically followed at three-monthly intervals at which time routine blood sampling is performed. Information from all recipients is entered into a database, providing data for clinical and virological outcome studies of patients receiving antiretroviral therapy. These studies form the basis of ongoing revisions to the Centre’s treatment guidelines. | Drug Treatment Program | Download | |||||||||||||||||||||||
| September, 2010 | STOP HIV/AIDS Pilot Project Indicators Report (Sept 2010) | Seek and Treat, STOP HIV/AIDS | Download | ||||||||||||||||||||||||
| August, 2010 | STOP HIV/AIDS Update (Spring/Summer 2010) | Seek and Treat for Optimal Prevention of HIV/AIDS (STOP HIV/AIDS) will will expand access to HIV/AIDS medications among hard-to-reach and vulnerable populations in Vancouver’s Downtown East Side and Prince George. For more information on STOP HIV/AIDS, including updates on progress, please refer to our regular bulletin. The first edition is now available for download in PDF format. | Seek and Treat, STOP HIV/AIDS | Download | |||||||||||||||||||||||
| August, 2010 | Drug Treatment Program Update (June 2010) | A key component of the Centre’s mandate is to monitor the impact of HIV/AIDS on British Columbia. The BC-CfE provides essential information to local health authorities, treating physicians and the community-at-large on an ongoing basis. The Drug Treatment Program Update is one example of the Centre’s commitment. In B.C., all anti-HIV medications are distributed at no cost to eligible HIV-infected individuals through the Centre’s Drug Treatment Program (DTP). The DTP Update provides an important overview of available anti-HIV drugs, common drug combinations and distribution of active DTP participants throughout the province. DTP participants are typically followed at three-monthly intervals at which time routine blood sampling is performed. Information from all recipients is entered into a database, providing data for clinical and virological outcome studies of patients receiving antiretroviral therapy. These studies form the basis of ongoing revisions to the Centre’s treatment guidelines. | Clinical Programs, Drug Treatment Program, Epidemiology and Population Health | Download | |||||||||||||||||||||||
| August, 2010 | July/August 2010 | UNAIDS Treatment 2.0 based on made-in-B.C. "treatment as prevention" strategy
Mr. Sidibé, a world-renowned and longtime advocate of innovative ways to curb the HIV/AIDS epidemic, said Treatment 2.0 will reshape the global response to AIDS. It will help achieve two crucial benefits: a dramatic reduction in AIDS-related deaths and a decrease in new HIV infections. The lifesaving concept of "treatment as prevention" – developed at the BC Centre for Excellence in HIV/AIDS (BC-CfE) – provided the building blocks for this new treatment approach. In his speech at the opening session of AIDS 2010, Mr. Sidibé cited the groundbreaking work coming out of B.C. as evidence supporting the UNAIDS' push for Treatment 2.0 – a global HIV treatment revolution. "Treatment is a right, treatment is a smart investment. It reduces HIV transmission, TB, and maternal and child deaths," he told thousands of attendees in a sprawling auditorium onsite and countless others watching via video links worldwide. AIDS 2010 endorses BC-CfE initiative as key pillar in fight against HIV and AIDS "Thanks to the support of British Columbia Premier Gordon Campbell, and the dedication of Julio Montaner, the world now knows that treatment as prevention is a reality that works for the three Ps: It works for the patient, it works for the people and it works for the pocket." UNAIDS has estimated that if Treatment 2.0 is successfully implemented, it could avert 10 million HIV/AIDS deaths by 2025. B.C. research inspires Treatment 2.0Mr. Sidibé's remarks at AIDS 2010 came soon after the BC-CfE released a study in Vienna showing that the introduction of highly active antiretroviral therapy (HAART) for HIV patients has halved the number of new HIV diagnoses in B.C. since 1996. "Dr. Montaner's study, published in The Lancet, was the strongest confirmation yet that treatment and prevention are two sides of the same coin," said The Economist. "The study, together with previous work showing that HAART reduces the rate of transmission between discordant couples (in which only one partner is infected) by more than 90%, points to the conclusion that widespread use of antiretroviral drugs helps to explain the 17% fall in the rate of new HIV infections seen around the world between 2001 and 2008." In a front-page story, Dr. Montaner, director of the BC-CfE, told The Province newspaper that July 18 was a great day for British Columbia, as the made-in-B.C. initiative put the province at the forefront of the HIV and AIDS response. "While treatment is highly cost-effective on its own merits because it is a life-saving, disease-preventing intervention, it has a multiplier effect on the prevention axis, which makes this a very attractive investment," he said. Dr. Montaner stated that expanding HAART coverage will have multiple benefits including decreasing tuberculosis, decreasing the number of orphans and preserving and strengthening health systems in affected countries around the world. "Universal access to care, treatment and prevention is the fundamental building block for maternal and child health. Let me say this once more, there cannot be maternal and child health without universal access," he said. G8 fails to fulfill universal access pledgeG8 nations promised in 2005 to fund universal access by 2010, but have not lived up to their commitment. Dr. Montaner noted that his own federal government, led by Canadian Prime Minister Stephen Harper, has failed to fully fund universal access and missed an opportunity to put the HIV strategy firmly back on track when it largely ignored universal access during recent G8 meetings in Canada. He noted, however, that France's First Lady, Carla Bruni-Sarkozy, has strongly supported treatment as prevention and the need to deliver on the promise of universal access. "We ask her to ensure that her husband, the president of France, becomes a forceful advocate for that position when France hosts next year's G8 meeting," he said. Dr. Montaner added that governments around the world will now say they face a crisis of resources when asked for money to provide funding for universal access, but resources are not the issue. "The challenge is not finding money, but changing priorities," Dr. Montaner noted. "When there is a Wall Street emergency or an energy crisis, billions upon billions of dollars are quickly mobilized. People's health deserves a similar financial response and much higher priority." Meanwhile, high-level speakers at the conference – including former U.S. President Bill Clinton and billionaire philanthropist Bill Gates – added their thoughts on ways forward to combat HIV and AIDS. A total of 193 countries were represented at the conference and 19,100 people participated at AIDS 2010, and all were left with a sobering reminder from Dr. Montaner as they left the conference. "As we say farewell to each other and pack our bags to leave Vienna, we must remember that another 7,000 people will become infected today, as they did yesterday and will again tomorrow," said Dr. Montaner. "This epidemic is our life's work. Let's ensure that the epidemic ends, soon and forever." | Aboriginal, Harm Reduction, HIV Clinical Care | Forecast Newsletter | Download | ||||||||||||||||||||||
| July, 2010 | Drug Treatment Program Update (May 2010) | A key component of the Centre’s mandate is to monitor the impact of HIV/AIDS on British Columbia. The BC-CfE provides essential information to local health authorities, treating physicians and the community-at-large on an ongoing basis. The Drug Treatment Program Update is one example of the Centre’s commitment. In B.C., all anti-HIV medications are distributed at no cost to eligible HIV-infected individuals through the Centre’s Drug Treatment Program (DTP). The DTP Update provides an important overview of available anti-HIV drugs, common drug combinations and distribution of active DTP participants throughout the province. DTP participants are typically followed at three-monthly intervals at which time routine blood sampling is performed. Information from all recipients is entered into a database, providing data for clinical and virological outcome studies of patients receiving antiretroviral therapy. These studies form the basis of ongoing revisions to the Centre’s treatment guidelines. | Clinical Programs, Drug Treatment Program, Epidemiology and Population Health | Download | |||||||||||||||||||||||
| June, 2010 | Safety Alert - Pharmacovigilance Program (June 2010) | Clinical Programs, Quality and Safety | Download | ||||||||||||||||||||||||
| June, 2010 | Drug Treatment Program Update (April 2010) | A key component of the Centre’s mandate is to monitor the impact of HIV/AIDS on British Columbia. The BC-CfE provides essential information to local health authorities, treating physicians and the community-at-large on an ongoing basis. The Drug Treatment Program Update is one example of the Centre’s commitment. In B.C., all anti-HIV medications are distributed at no cost to eligible HIV-infected individuals through the Centre’s Drug Treatment Program (DTP). The DTP Update provides an important overview of available anti-HIV drugs, common drug combinations and distribution of active DTP participants throughout the province. DTP participants are typically followed at three-monthly intervals at which time routine blood sampling is performed. Information from all recipients is entered into a database, providing data for clinical and virological outcome studies of patients receiving antiretroviral therapy. These studies form the basis of ongoing revisions to the Centre’s treatment guidelines. If you would like to request archived Drug Treatment Program reports, please contact Andrea Keesey. | Clinical Programs, Drug Treatment Program, Epidemiology and Population Health | Download | |||||||||||||||||||||||
| June, 2010 | SAFETY ALERT: RITONAVIR AND INTRA-ARTICULAR TRIMCINOLONE ACETONIDE INJECTION | June, 2010 - The Pharmacovigilance Program at the BC Centre for Excellence in HIV/AIDS has received four reports of suspected drug interaction between ritonavir and triamcinolone acetonide intra-articular injection leading to symptoms of corticosteroid excess (Cushingoid features) and adrenal suppression. The affected patients were HIV-infected adults whose antiretroviral therapy included a protease inhibitor boosted with ritonavir 100-200 mg daily. All patients received one or more injections of triamcinolone acetonide 40-80 mg into shoulder or knee joints. Adrenal suppression (morning serum cortisol <28 nmol/L, reference range 175-685 nmol/L) was diagnosed four to 14 weeks after the first triamcinolone acetonide injection. | Pharmacovigilance Initiative, Quality and Safety | HIV Clinical Care | Download | ||||||||||||||||||||||
| June, 2010 | Jun-10 |
| HIV Clinical Care | Forecast Newsletter | Download | ||||||||||||||||||||||
| May, 2010 | May-10 |
| Forecast Newsletter | Download | |||||||||||||||||||||||
| April, 2010 | Drug Treatment Program Update (March 2010) | A key component of the Centre’s mandate is to monitor the impact of HIV/AIDS on British Columbia. The BC-CfE provides essential information to local health authorities, treating physicians and the community-at-large on an ongoing basis. The Drug Treatment Program Update is one example of the Centre’s commitment. In B.C., all anti-HIV medications are distributed at no cost to eligible HIV-infected individuals through the Centre’s Drug Treatment Program (DTP). The DTP Update provides an important overview of available anti-HIV drugs, common drug combinations and distribution of active DTP participants throughout the province. DTP participants are typically followed at three-monthly intervals at which time routine blood sampling is performed. Information from all recipients is entered into a database, providing data for clinical and virological outcome studies of patients receiving antiretroviral therapy. These studies form the basis of ongoing revisions to the Centre’s treatment guidelines. If you would like to request archived Drug Treatment Program reports, please contact Andrea Keesey. | Clinical Programs, Drug Treatment Program | Download | |||||||||||||||||||||||
| March, 2010 | Mar-10 |
| AIDS Research Program | HIV Clinical Care | Forecast Newsletter | Download | |||||||||||||||||||||
| February, 2010 | Feb-10 | B.C. government funds $48-million Seek and Treat programThe Government of B.C. and the BC Centre for Excellence in HIV/AIDS (BC-CfE) made history at St. Paul's Hospital on the morning of February 4, 2010. In the hospital's expansive New Lecture Theatre, B.C. Health Services Minister, Kevin Falcon, stepped up to the podium in front of staff members, persons living with HIV, media, BC-CfE partners and government officials, and pledged $48 million for a life-saving pilot program that has been more than five years in the making. The pilot, called Seek and Treat, will be implemented in Vancouver's Downtown Eastside and Prince George and is the first of its kind in Canada and internationally. Over four years, it will expand access to HIV and AIDS medications among hard-to-reach populations, including sex trade workers, injection drug users and men who have sex with men. The Seek and Treat program will enable health care workers to reach out to more British Columbians living with HIV and to engage those individuals who are medically eligible to gain access to medications to stop HIV's progression to AIDS. Meanwhile, with more people suffering from HIV enrolled in effective HAART treatment, the virus' ability to spread to others in the community will be significantly reduced or even eliminated. "Seek and Treat promises to decrease HIV and AIDS-related suffering and further prevent the spread of HIV," said Falcon, to appreciative applause from those celebrating this milestone in the battle to defeat HIV and AIDS. "British Columbia continues to be a recognized global leader in the fight against HIV/AIDS with this groundbreaking approach thanks to the BC Centre for Excellence in HIV/AIDS at St. Paul's Hospital, under the leadership of Dr. Julio Montaner," Falcon added. | AIDS Research Program, Clinical Research | Harm Reduction | Forecast Newsletter | Download | |||||||||||||||||||||
| January, 2010 | Jan-10 | A decade of progress against HIV, but gains at riskDr. Julio Montaner, director of the BC Centre for Excellence in HIV/AIDS (BC-CfE) and president of the International AIDS Society (IAS), has travelled in recent months to Moscow, Japan, Germany and Washington, D.C. Everywhere, he had a simple message for government officials: HIV/AIDS can be defeated if Canada and other G8 nations follow the lead of the United States, and live up to their funding commitments. During a wide-ranging interview focusing on progress and setbacks in HIV treatment during the past decade, Dr. Montaner commended the U.S. for playing what he called a ‘critical role' in accelerating HIV treatment and care in the developing world. He pointed out that if it weren't for PEPFAR (the U.S. President's Emergency Plan for AIDS Relief), the rollout of highly active antiretroviral therapy (HAART) would be nowhere close to where it's today. "If we often complain about the fact that we are only half way where we should be, the real reason is not for lack of support from the U.S., it's because of the inability of other G8 nations, including and in particular Canada, to match the U.S. contribution on a gross domestic product basis," said Dr. Montaner. Following his recent visit and discussions with government officials in Washington D.C., Dr. Montaner said the U.S. is ready to embrace the made-in-B.C. HIV treatment-as-prevention model (BC-CfE STOP HIV & AIDS) as part of its agenda to combat the HIV epidemic in Washington, D.C., which has one of the worst HIV epidemics in the country. In addition to furthering the way forward in HIV/AIDS treatment and prevention with HIV experts and senior White House officials, Dr. Montaner was in Washington, D.C. to participate and show solidarity for the U.S. government's landmark decision to lift the HIV travel ban after more than two decades. "We are extremely pleased that HIV-positive people will be able to have a more normal life as a result of this decision. The ban represented another example of stigma and discrimination at work. This should have been done a long time ago," said Dr. Montaner. On his way home from Washington, D.C., Dr. Julio Montaner was a guest on CBC's The Hour in December 2009. In conversation with host George Stroumboulopoulos, Dr. Montaner stressed that it's critical for the G8 nations, including Canada, to live up to their funding commitments in order to conquer the HIV/AIDS epidemic. During his visit, the IAS announced that the 2012 International AIDS Conference will be held in Washington, D.C. as a tangible sign of appreciation for the administration's work in striking the ban. The U.S. has been setting several excellent examples for the rest of the world to follow in combating HIV/AIDS, including a recent announcement by the National Institute on Drug Abuse (NIDA) to fund research up to US$50 million over five years to evaluate the treatment-as-prevention strategy (again based on the BC-CfE STOP HIV & AIDS) in the criminal justice setting | Harm Reduction | Forecast Newsletter | Download | ||||||||||||||||||||||
| December, 2009 | Dec-09 | Will Harper's G8 leadership advance the fight against HIV/AIDS?Today, on World AIDS Day, Canadians and indeed all citizens of the world have much to aspire to. We are now at a tipping point. We have extremely effective HIV treatment and the means to deliver it to millions of HIV-infected people worldwide. The treatment, called highly active antiretroviral therapy (HAART), was developed in part by Canadians and has been successfully used around the world to stop HIV from progressing to AIDS and death. HAART has been shown to prevent HIV transmission from an infected mother to the baby, to the point that vertical HIV transmission has been effectively eliminated in Canada. If the global community comes together — now — and tackles HIV with purpose and passion, we have a unique opportunity to dramatically change the course of the pandemic within a decade. Reaching that goal will have cost implications — billions of dollars — and will demand true leadership rather than empty promises. Today, Canada has an opportunity to play a major role in moving the agenda forward towards the global control of HIV/AIDS. We must demand that our political leadership delivers on earlier promises. In 2005, at the Group of Eight (G8) Summit in Gleneagles, Scotland, Canada committed to help fund universal access to HIV prevention, treatment and care by 2010 and to turn the tide against HIV/AIDS by 2015. This included a pledge to deliver lifesaving HAART to everyone in medical need by 2010. Canada has failed to keep its word: only weeks away from 2010 HAART coverage is less than 50 per cent, according to the most optimistic estimates. Canada will host next year's G8 Summit in Muskoka, Ontario. As the G8 meeting host, Harper will set the agenda for the June 2010 meetings, which will also bring together the influential Group of 20 (G20). The Muskoka Summit — just six months before the 2010 United Nation's deadline for universal access — offers an ideal opportunity to recommit to achieve this goal before 2015. Everything will be lost if we fail to recommit. The real cost of the G8's failure is the estimated 7,400 people who become newly infected with HIV daily and the nearly 5,500 who will die each day from AIDS-related illness. All of which are preventable. Prime Minister Harper must lead now to help curb global death and despair due to HIV/AIDS. | AIDS Research Program | Forecast Newsletter | Download | ||||||||||||||||||||||
| October, 2009 | Oct-09 | NIDA invests $50 million to evaluate made-in-BC strategy for control of HIV/AIDSThe US National Institute on Drug Abuse (NIDA) intends to fund research worth up to US$50 million over five years to evaluate the "seek-and-treat" strategy originally developed at the BC Centre for Excellence in HIV/AIDS (BC-CfE). Momentum growing for seek and treatDr. Montaner introduced the seek-and-treat strategy in 2006. He explained that voluntary testing combined with an immediate and aggressive roll out of HAART to every infected person could potentially eliminate HIV. | AIDS Research Program, STOP HIV/AIDS | HIV Clinical Care, Treatment as Prevention® | Forecast Newsletter | Download | |||||||||||||||||||||
| September, 2009 | Sep-09 | BC-CfE Researchers Running Key International Research ProgramsTwo international programs led by Dr. Thomas Kerr and Dr. David Moore are continuing to enhance the global reputation of the BC Centre for Excellence in HIV/AIDS (BC-CfE) for innovative research. These programs provide new information that will help fight the HIV/AIDS pandemic. For the past 17 years, BC-CfE's multidisciplinary team of researchers has led several leading-edge international projects in countries such as Argentina, South Africa and Thailand. "I am truly humbled by the commitment BC-CfE researchers have shown towards identifying and understanding the many factors that affect the health of vulnerable populations around the world," said Dr. Julio Montaner, director of the BC-CfE. Study reveals Thailand's ‘war on drugs' is a failureAlarmed by the growing drug use, especially among youth, and worried about the negative impact it could have on the future of the children in Thailand, then Thai Prime Minister Thaksin Shinawatra launched the Thai ‘war on drugs' in 2003. Although in theory the war on drugs emphasized treating drug users as ‘patients' rather than criminals, in practice it focused on arresting and incarcerating suspected drug users and dealers. This resulted in extra-judicial killings of over 2,200 alleged drug dealers. In 2008, when Thailand revived its aggressive drug war policy of 2003, a research team led by Dr. Thomas Kerr started a research project titled the ‘Mitsampan Community Research Project' in Thailand. The project employed a community-based approach, with the peer-run (run by Thai injection drug users (IDUs)) Mitsampan Harm Reduction Centre (MSHRC) contributing a 15-member team of peer researchers. The Thai AIDS Treatment Action Group (TTAG) and the Chulalongkorn University also collaborated on this project. The team surveyed more than 250 local IDUs between June and September 2008. This project is one of the first to demonstrate how Thailand's war-on-drugs policy has affected the health and well-being of Thai IDUs. The following key findings raise serious questions about the merits of the government's current policy: • While slightly over half the study participants reported observing an increase in police presence, the study found no evidence that these individuals had significantly different drug use behaviours compared to other study participants. • Forty-eight per cent of participants reported having drugs planted on them by police. • Seventy-eight per cent of participants had been incarcerated at some point in the past and eighty-one per cent of those individuals who were incarcerated reported syringe sharing while in prison. "Our findings suggested negative consequences of the Thai war-on-drugs policy, including human rights violations and adverse health impacts," said Dr. Kerr. "The findings reinforce what we have always suspected – that a policy solely based on drug law enforcement will not reduce, but perpetuate more ills related to drug addiction." | Forecast Newsletter | Download | |||||||||||||||||||||||
| July, 2009 | Safety Alert - Pharmacovigilance Initiative (July 2009) | Clinical Programs, Quality and Safety | Download | ||||||||||||||||||||||||
| July, 2009 | SAFETY WARNING: ABACAVIR USE IN HLA-B*5701 POSITIVE PATIENTS AND UNTESTED PATIENTS | July, 2009 - The Pharmacovigilance Initiative at the BC Centre for Excellence in HIV/AIDS received a report of an HLA-B*5701 positive patient who had tolerated long term abacavir therapy, discontinued antiretroviral drugs for several months, then developed a diffuse rash, respiratory distress and fever shortly after re-initiating an abacavir-containing regimen. The symptoms and rapid onset were consistent with a clinical diagnosis of abacavir hypersensitivity reaction. | Pharmacovigilance Initiative, Quality and Safety | HIV Clinical Care | Download | ||||||||||||||||||||||
| July, 2009 | July/August 2009 | Forecast Newsletter | Download | ||||||||||||||||||||||||
| June, 2009 | Jun-09 | 5th IAS conference to be held in Cape TownBetween July 19 and 22, 5,000 scientists, community leaders and implementers will refocus attention on AIDS in Africa at the IAS 2009 Conference, to be held at the Cape Town International Convention Centre in South Africa. South Africa bears the largest burden of the AIDS pandemic of any country in the world, with an estimated 5.7 million people living with HIV in 2007. The decision to hold IAS 2009 in southern Africa reflects organizers' desire to refocus the attention of the international scientific community on the continued challenges facing a region that is battling a generalized epidemic, and to highlight the latest efforts to fight it. "The need for evidence-based interventions has never been more important," said Dr. Julio Montaner, International AIDS Society (IAS) President and IAS 2009 Conference Chair, and Director of the BC Centre for Excellence in HIV/AIDS. "Good science must inform good policy and programming to ensure the best outcomes for individuals and communities. Science has given us the ability to save lives; now is not the time to be short-sighted." The 5th IAS Conference on HIV Pathogenesis, Treatment and Prevention will focus on evidence-based approaches to HIV prevention, treatment, care and support, while emphasizing the continued need to strategically invest in HIV research, including operations research, to guide implementation of programs. The opening session will highlight the convergence of science and activism, and feature a scientific keynote address by 2008 Nobel Laureate and IAS Governing Council member Professor Françoise Barré-Sinoussi. While continuing its strong emphasis on basic, clinical and biomedical prevention sciences, IAS 2009 will feature a new program track focusing on operations research. The new track is intended to further emphasize the defining objective of the IAS conference: how to quickly translate scientific discoveries into practical interventions that respond to current challenges in HIV prevention, treatment and care, particularly in low- and middle-income countries. In addition to abstract-driven sessions, the conference will feature a variety of symposia and bridging sessions. Presentations will include: • Reuben Granich (US): Highly Active Antiretroviral Therapy (HAART) as Prevention • Amalio Telenti (Switzerland): HIV and Host Genetics • Louise Kuhn (South Africa): Prevention of Mother-to-Child Transmission • Wafaa El-Sadr (US): Inflammation and HIV: A New Paradigm • Ron Gray (UK): Biomedical Prevention, Including Microbicides, Vaccines, Circumcision and Pre-Exposure Prophylaxis (PrEP) • Bruce Walker (US): Immune Control of HIV Replication • Stefano Bertozzi (Mexico): Financing the Long-Term Response to HIV • Prashini Moodley (South Africa): HIV and Extremely Drug-Resistant Tuberculosis • Gerald Friedland (US): Advances in Operations Research Addressing the Convergent HIV and TB Epidemics • Pedro Cahn (Argentina): Antiretroviral Therapy in 2009: Successes and Challenges • Rachel Jewkes (South Africa): Gender and Sexuality: Recent Data and its Implications for HIV Prevention, Treatment, Care and Support • Jerald Sadoff (US): Developments in Tuberculosis Vaccine Research Full conference program details and registration information are available at www.ias2009.org. During the conference, links to all abstracts, as well as webcasts, session slides and speeches will be available on the website. | Forecast Newsletter | Download | |||||||||||||||||||||||
| May, 2009 | May-09 | Pharmacovigilance project celebrates successThe BC Centre for Excellence in HIV/AIDS (BC-CfE) has successfully completed a demonstration project that is helping B.C.'s health care system monitor side effects (adverse drug reactions) to antiretroviral medications. Adverse drug reactions can gravely affect patients' health and compromise treatment success. Although all drugs are tested for safety before they are approved for sale in Canada, pre-marketing clinical trials cannot study enough patients to be able to detect rare or delayed onset drug reactions, or reactions that predominantly affect special groups, such as women, seniors or specific ethnic groups. These types of adverse reactions may not be discovered until after a drug is marketed and widely used. Ongoing surveillance of adverse drug reactions is required to detect unexpected toxicities as soon as possible, so that health care providers and patients can be warned of new safety concerns. This type of monitoring activity is conducted through pharmacovigilance programs which collect, evaluate and analyze reports of drug toxicity and use this information to understand and prevent drug-related problems. Health care professionals and patients themselves are the most important sources of information in identifying a drug's potential toxicity. Since its inception, the BC-CfE has been active in collecting and reporting antiretroviral treatment-related information and has published numerous scientific studies and issued public safety alerts. However, until recently, the BC-CfE lacked the resources to operate an ongoing adverse drug reaction reporting and monitoring program. Thanks, in part, to the generous support of the Canadian Patient Safety Institute, the BC-CfE was able to launch a pharmacovigilance program as a demonstration project in July 2008. The first HIVfocused reporting mechanism of its kind in B.C., the program provides an opportunity for all health care professionals and for patients themselves to submit reports of suspected adverse drug reactions to antiretroviral medications. "Because the BC-CfE Drug Treatment Program provides all antiretroviral medications within B.C., we can estimate the proportion of people taking a drug or drug regimen who experience a particular adverse reaction," explained Kathy Lepik, project coordinator. "The BC-CfE sets the HIV treatment guidelines for the province, so we will also be able to respond rapidly and translate reports of unexpected drug toxicities into safety alerts for health care providers and people living with HIV/AIDS." During the first nine months of pharmacovigilance program operation, approximately 5,000 people living with HIV/AIDS were treated with antiretroviral medications and the program received 435 reports of adverse drug effects via prescription forms and spontaneous reports. Approximately 80 per cent of these reports were submitted by physicians, and 20 per cent by pharmacists and nurses. Dr. Rolando Barrios, project leader, noted, "Reporting patterns to date have been consistent with the known adverse reaction profiles of the commonly used antiretroviral medications, which suggests that there are no identifiable biases in the reporting process. We are presently closely monitoring and investigating some potential safety concerns." | Forecast Newsletter | Download | |||||||||||||||||||||||
| April, 2009 | Apr-09 | BC Liberals commit to HIV/AIDS pilot projectPremier Gordon Campbell announced a commitment to a pilot project that will expand access to HIV and AIDS drugs to the street-involved population in downtown Prince George and Vancouver's Downtown Eastside. The program will decrease AIDS-related suffering and further prevent the spread of HIV disease. "People living on the streets and other ‘hard to reach' populations are much less likely to access appropriate care and support or to have a family doctor, and are more likely to have undiagnosed and untreated HIV/AIDS," said Premier Campbell. "Through the excellent work of Dr. Julio Montaner and the BC Centre for Excellence in HIV/AIDS, a pilot project is being proposed to connect with people on an individual basis and get them a chance to access the services they need." Both downtown Prince George and the Downtown Eastside of Vancouver are areas which have been profoundly affected by HIV/AIDS. The pilot will involve integration by health system partners from public health and non-governmental community-based organizations, to low-threshold interdisciplinary primary care clinics and private practice physicians. While the proposal will facilitate access to HIV testing and care, engagement will be strictly voluntary and will fully respect standard practices, including participants' informed consent. The proposal places a greater emphasis on enhanced care and support using specialist and tertiary care resources in a more focused way. Once fully operational, the pilot project will cost about $20 million per year. It is estimated that more than 12,000 people in B.C. are living with HIV, and approximately 27 per cent of these individuals remain undiagnosed. Highly active antiretroviral therapy (HAART), introduced in 1996 at the Vancouver International Conference on AIDS, is considered the ‘gold standard' for treatment of HIV, and was in large part driven by groundbreaking, internationally recognized work at the BC Centre for Excellence in HIV/AIDS. Today's pilot project commitment will facilitate access to life-saving HAART drugs for at-risk populations. "We have made great strides in HIV/AIDS treatment, allowing individuals to live longer lives," said Dr. Montaner. "The challenge we face now is reaching out to individuals who would otherwise fall between the cracks and cannot access treatment. This program is aimed at bringing the treatment to the people in need. I want to thank Premier Campbell for his leadership and commitment to this important and innovative initiative." "Dr. Julio Montaner is a recognized international leader, who is passionate about the care, treatment and support of HIV infected persons. We are fortunate to have him lead the BC Centre for Excellence in HIV/AIDS," said Premier Campbell. "Because of their work right here in B.C., people's lives around the world are changed for the better." At an individual level, HAART treatment slows disease progression, extends life expectancy, and significantly reduces the number of new AIDS-related diseases and HIV-related deaths. At a population level, the BC Centre for Excellence in HIV/AIDS has provided strong evidence that treatment of people living with HIV in a given jurisdiction can also dramatically decrease the transmission of the disease. Mathematical modelling suggests that this pilot project in these two regions could avert as many as 173 HIV infections in the first five years, which in turn represents about $65 million in avoided lifetime HIV treatment costs alone. | Forecast Newsletter | Download | |||||||||||||||||||||||
| March, 2009 | Mar-09 | Minister Abbott opens international summit in Vancouver | Forecast Newsletter | Download | |||||||||||||||||||||||
| February, 2009 | Feb-09 | Japanese AIDS health care representatives visit BC-CfERecently, two AIDS care nurses from Japan's AIDS Clinical Center (ACC) have returned to the BC-CfE to continue learning from its progressive and effective approach to HIV/AIDS treatment and care. The ACC was established in 1997, as part of the settlement to compensate the victims of transfusion related HIV. Today, it provides treatment, information, clinical research and outreach services throughout Japan. Headquartered in Tokyo, the ACC maintains seven regional AIDS clinics throughout the country. Since 1998, 10 ACC coordinator nurses have visited the BC-CfE and HIV/AIDS programs in Vancouver. The coordinator nurses act as case managers and carry high case-loads of patients; their main focus is to support adherence to antiretroviral therapy. During previous visits, they were there to observe the collaborative care models in action. They intended to integrate this model—which brings hospitals, non-governmental organizations and the broader community together to co-ordinate better care for HIV/AIDS patients—into the Japan's system of care. In February 2009, Irene Goldstone, director of Professional Education and Care Evaluation for the Centre, facilitated the most recent visit for ACC care nurses Drs. Kazuko Ikeda, Patient Care Consultant, and Megumi Shimada, Nursing Consultant. The focus for this visit was improving home care, creating capacity for long-term residential care and creating outreach services to street-involved people with AIDS. "The challenges that Vancouver faces now are becoming more widespread in Japan," explained Dr. Ikeda. She cites intravenous drug use, the street sex trade and increasing numbers of street-involved youth as some of the issues that are contributing to an increase in HIV infections. The situation is worsened by national policies that do not support harm reduction such as needle exchange or methadone programs. Japan, along with the United States and Sweden, is among the few G8 countries that have not adopted harm-reduction policies in the response to HIV/AIDS. Expanding home care and access to long-term residential care for people with HIV/AIDS is also a priority in Japan for this year's delegation. Dr. Shimada explains that although home care and residential care are available for geriatric patients, younger people, most of whom are men who have sex with men, have not been integrated into residential care programs. Tragically, because of the stigma of the disease itself and of homosexuality, many of these men received treatment for HIV very late in their illness and consequently require long-term care. For these people, home care and residential care are needed to prevent undue suffering and preserve their dignity; it is also a critical step in conserving hospital resources and making hospital beds available for acutely ill people. In addition to learning from the Centre's knowledge-base and infrastructure, Drs. Ikeda and Shimada said they are also being exposed to cultural differences that have an impact on AIDS care. "We are impressed with the diversity of the staff in Vancouver; most of the staff who work in HIV/AIDS-related care in Japan are women in their thirties. Here, you have different ethnicities, genders and ages working together and sharing different perspectives." Dr. Shimada added, "We're inspired by the way staff members are confident in their own expertise and not afraid to ask others to contribute theirs. They share information freely and harness synergies that take everyone further in their understanding and capabilities." | Forecast Newsletter | Download | |||||||||||||||||||||||
| January, 2009 | Jan-09 | Aboriginal street youth more likely to be HIV-positiveIn Canada, there are upwards of 150,000 homeless and street-involved youth, and they are far more vulnerable to HIV and other sexually transmitted infections. In fact, infection rates for diseases such as chlamydia and gonorrhea are 10 times that of the general adolescent population in the country. And certain factors, including ethnicity, can increase a youth's risk profile even more. In particular, the Aboriginal population in Canada is represented disproportionately among HIV infections. Although only 3.3% of Canadians identify as American Indian, First Nations, Inuit or Métis, Aboriginal people accounted for 18.8% of positive HIV test reports in 1998. That number surged to 27.3% in 2006. Researchers with the BC Centre for Excellence in HIV/AIDS looked at HIV infection among a group of more than 500 Vancouver street youth between the ages of 14 and 26 who were homeless or street-involved and spent most of their time in the Downtown Eastside. The study drew from the At Risk Youth Study (ARYS), a prospective cohort of more than 500 drug-using and street-involved youth who live in the Vancouver area. A total of 529 participants, with a median age of 22 years, completed a baseline survey and were eligible for this analysis. Of these, 76.4% had been homeless in the past six months, and 41.8% reported ever injecting drugs. One hundred and twenty-seven participants (24%) self-identified as Aboriginal, American Indian, First Nations, Inuit, or Métis. Research showed that 2% of the non-Aboriginal youth in the study were infected with HIV, while among Aboriginal youth the figure was 5.5%. This means that Aboriginal youth were nearly three times as likely to test positive for the virus that causes AIDS. Surveys distributed to participating youth included questions about their injection drug use, syringe sharing, history of incarceration, history of sex work and history of sexual abuse. The fact that the HIV-infected Aboriginal youth were less likely to report injection drug use and be co-infected with hepatitis C suggests that factors such as unsafe sexual activity and sex work may be responsible for a significant proportion of infections. More than half of youth participating in the study reported experiencing sexual abuse. Previous Vancouver-based studies have identified incarceration as increasing HIV risk behaviours and HIV incidence; this study similarly linked a high prevalence of incarceration among the youth with a high risk of infection. All seven Aboriginal youth who tested positive for HIV also reported a history of incarceration. The research points to the immediate need for culturally appropriate and evidence-based programs to support HIV-positive Aboriginal youth and to prevent further infections among this marginalized population. The results of this study also support statements by the Assembly of First Nations and the Canadian AIDS Aboriginal Network that programs for Aboriginal young people are chronically under-funded. Further investment in existing programs and the creation of new evidence-based strategies, with the full participation of the Aboriginal community, are urgently required to prevent further infections among Aboriginal youth and to support those who are already infected. | AIDS Research Program, Epidemiology and Population Health | Aboriginal, HIV Clinical Care | Forecast Newsletter | Download |