STOP HIV/AIDS®
Documents & Reports
HIV Monitoring Quarterly Reports, Third Quarter 2018
- HIV Monitoring Quarterly Report for British Columbia, Third Quarter 2018
- HIV Monitoring Quarterly Report for Fraser Health, Third Quarter 2018
- HIV Monitoring Quarterly Report for Interior Health, Third Quarter 2018
- HIV Monitoring Quarterly Report for Northern Health, Third Quarter 2018
- HIV Monitoring Quarterly Report for Vancouver Coastal Health, Third Quarter 2018
- HIV Monitoring Quarterly Report for Island Health, Third Quarter 2018
Are we close to the end of AIDS?

Just two years ago, UNAIDS announced a window of opportunity to end the AIDS epidemic by 2030 by fast-tracking towards meeting the 90-90-90 Target. There was tempered optimism this ambitious goal was within reach. Now, the international HIV community is experiencing a sense of urgency: complacency is moving us perilously close to an HIV rebound.
This was a main focus when experts, advocates and community gathered for the most recent AIDS conference in Amsterdam this past summer. According to the World Health Organization, there are too many people not accessing care which will impede reaching the Target goals of 90% of all those living with HIV being diagnosed, 90% of all those diagnosed accessing treatment and 90% of those on treatment achieving viral suppression.
Some leading governments have stalled funding towards helping to expand access to treatment for ending AIDS. After widening access to treatment in Africa from a baseline of 50,000 to 14 million, funding for PEPFAR, the United States President’s Emergency Plan for AIDS Relief, has generally plateaued for the past decade. This, despite the fact that HIV treatment is still not accessible in many health care settings in low- and middle-income countries.
At a time when we have reached consensus on the made-in-BC 90-90-90 Target as a means to end AIDS as a pandemic, the international community’s investment is faltering. Canada needs to lead the charge in asking for the expansion of the funding envelope to provide universal coverage for effective HIV treatment and prevention drugs.
At the last Global Fund Replenishment Conference in 2016, Canada boosted its international funding for fighting HIV by 20%. Canada must be a model in ending AIDS here at home and deliver on the promise of the Treatment as Prevention (TasP) strategy. The winning and cost-effective TasP strategy, implemented in BC, involves expanding access to testing and the immediate, universal provision of HIV antiretroviral treatment upon diagnosis. More recently, seven Canadian provinces, including BC, expanded coverage of the HIV prevention drug, PrEP (pre-exposure prophylaxis).
The goal set to end AIDS by 2030 is not an arbitrary one. With a growing global population and strains to be imposed by climate change, we need to end AIDS before resources are shifted.
Climate change will impact progress on global health in ways both expected and unexpected. Food insecurity and drought can make it difficult to use HIV antiretroviral medications, even when available, as many must be taken with food. Triggered by the effects of changes in weather and landscape, mass migration is anticipated to increase.
Beyond the absence of action, discriminatory laws and policies in some world regions are targeting vulnerable groups such as people who use drugs and the LGBTQ community. Eastern Europe and Central Asia are seeing sharp increases in new HIV cases. By the end of 2017, official estimates from Russia showed around 1 million people living with HIV and only about one third receiving treatment, well below the 90-90-90 Target. Each year the country is seeing around 100,000 HIV cases, one of the highest rates of new infections in the world.
North America is experiencing pockets of HIV growth, for example in regions of Western Canada and the Southern United States. Marginalization and a lack of access to testing, treatment, care and other supports creates an environment for the HIV virus to spread and thrive.
BC can show the world what is possible by reducing our yearly number of new HIV cases to double digits. We have seen a steady decline from around 900 at the peak of the epidemic to around 200 cases in 2016.
Mathematical modelling shows that TasP when combined with PrEP could catalyze our progress towards ending AIDS. Also, integral to stopping HIV are outreach programs to address the basic needs of the most hard-to-reach populations, including barriers to treatment such as lack of housing or poverty.
This is not a drill. We know what will end AIDS is reducing stigma while expanding access to testing and treatment. Now, we need upfront investment in effective programs that could help locally, nationally and globally. Canada must lead by example by ensuring free access to TasP and PrEP nationwide to end AIDS and curb the spread of HIV.
HIV Monitoring Quarterly Reports, Second Quarter 2018
- HIV Monitoring Quarterly Report for British Columbia, Second Quarter 2018
- HIV Monitoring Quarterly Report for Fraser Health, Second Quarter 2018
- HIV Monitoring Quarterly Report for Interior Health, Second Quarter 2018
- HIV Monitoring Quarterly Report for Northern Health, Second Quarter 2018
- HIV Monitoring Quarterly Report for Vancouver Coastal Health, Second Quarter 2018
- HIV Monitoring Quarterly Report for Island Health, Second Quarter 2018
Spring ARV Update: Publicly-funded PrEP off to strong start in BC
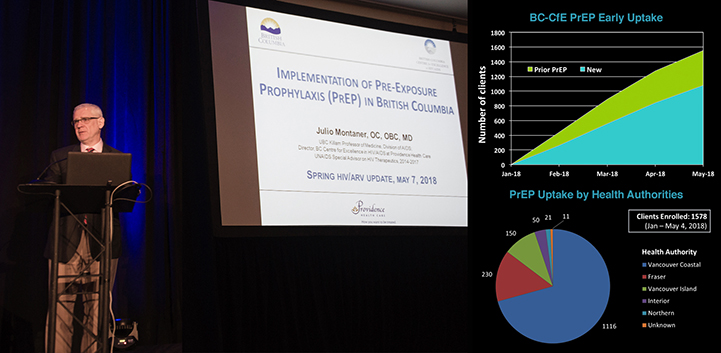
An HIV prevention program, available at no cost to people at high risk of HIV, is enrolling over 400 participants – primarily men who have sex with men (MSM) – every month right across BC. PrEP (pre-exposure prophylaxis) is a daily oral antiretroviral medication that prevents new HIV infection when taken consistently.
“Treatment as Prevention® has worked remarkably well here at home and around the world to bring down the rate of new HIV infections; however, we see a persistent rate of ongoing transmissions among MSM,” says Dr. Julio Montaner, Director of the BC Centre for Excellence in HIV/AIDS (BC-CfE). “Our research shows PrEP will drastically reduce new cases of HIV in BC.”
Since it’s official rollout in January of 2018, over 1,500 people have enrolled in the publicly funded PrEP program across BC. The median age of enrollees is 34 and 99% of them are male. Approximately 30% have accessed PrEP before while a larger number (70%) are new to the program.
Junine Toy, Senior Manager of the BC-CfE Drug Treatment Program (DTP), expected to see a small number of prescribers join the PrEP program initially and was surprised by the results. One of the foundational programs of the BC-CfE, the DTP is funded by the provincial government (PharmaCare) to distribute anti-HIV drugs based on guidelines generated by the Therapeutic Guidelines Committee.
“We thought we would only get a small number of prescribers with a high number of patients, but we have seen over 300 prescribers across the province, many with only one or two PrEP clients,” says Toy. “This is truly heartening because it tells us people in BC are having important conversations with their family doctors about their health, preventatively and proactively.”
Most eligible individuals fall into the following groups — MSM, transgender women, those who have used NPEP (non-occupational post-exposure prophylaxis) more than once, people with ongoing relationships with HIV positive sex partners without a suppressed viral load and people who inject drugs with a known HIV-positive partner without a suppressed viral load. Many PrEP clients are assessed and provided with a HIRI-MSM score (HIV Incidence Risk Index for men who have sex with men) to determine their eligibility.
Enrollees must have MSP coverage, reside in BC, be HIV-negative and be able to withstand the effects of the medication. Once eligibility is established, the approval process is efficient, according to Toy. Once approved, clients should pick up their prescription promptly to prevent any delay in initiation and continue to be monitored regularly. After the initial screening, clients are checked after one month for HIV infection, renal function, tolerability, adherence, and ongoing risk, and then every three months thereafter.
“Doctors in BC can submit a request and within a few days, get approved and navigate the process by accessing the BC-CfE website, RACE (Rapid Access to Consultative Access), REACH (Rapid Expert Advice and Consultation for HIV) and the St. Paul’s Hospital Pharmacy PrEP phonelines for any additional information,” says Toy. “Physicians should monitor PrEP clients every three months – tying together the follow-up and prescription refills, allowing doctor and patient to reconnect frequently.”
MSM community groups and HIV researchers alike see the program as a pivotal part of ending the HIV epidemic among the MSM population in BC.
“Gay, bisexual and other men who have sex with men are disproportionally affected by the HIV epidemic in BC, with 46% of new cases occurring in this population,” says Montaner. “We developed a mathematical transmission model and determined the combination of Treatment as Prevention® and PrEP could lead to HIV elimination in BC among MSM over the next ten years (or by 2026).”
PrEP joins existing programs offered by the BC-CfE such as PEP (post-exposure prophylaxis) which has been developed and managed by the BC-CfE for twenty years. It provides HIV prevention medication in instances of sexual assault and occupational exposure. NPEP (non-occupational post-exposure prophylaxis) covers individuals who may have been exposed to HIV through consensual drug use or sexual encounters. NPEP started out as a pilot project and expanded provincially to coincide with the launch of PrEP.
HIV Monitoring Quarterly Reports, First Quarter 2018
- HIV Monitoring Quarterly Report for British Columbia, First Quarter 2018
- HIV Monitoring Quarterly Report for Fraser Health, First Quarter 2018
- HIV Monitoring Quarterly Report for Interior Health, First Quarter 2018
- HIV Monitoring Quarterly Report for Northern Health, First Quarter 2018
- HIV Monitoring Quarterly Report for Vancouver Coastal Health, First Quarter 2018
- HIV Monitoring Quarterly Report for Island Health, First Quarter 2018
HIV Monitoring Quarterly Reports, Fourth Quarter 2017
- HIV Monitoring Quarterly Report for British Columbia, Fourth Quarter 2017
- HIV Monitoring Quarterly Report for Fraser Health, Fourth Quarter 2017
- HIV Monitoring Quarterly Report for Interior Health, Fourth Quarter 2017
- HIV Monitoring Quarterly Report for Northern Health, Fourth Quarter 2017
- HIV Monitoring Quarterly Report for Vancouver Coastal Health, Fourth Quarter 2017
- HIV Monitoring Quarterly Report for Island Health, Fourth Quarter 2017


